Periprosthetic hip fractures show increasing incidence and complexity, representing a challenge for the surgeon. We aimed to evaluate the survival of uncemented modular tapered stems in the treatment of periprosthetic Vancouver B2 and B3 type fractures and review the main complications and factors associated with decreased survival.
Materials and methodsWe performed a retrospective study of patients submitted to revision arthroplasty for treatment of periprosthetic femoral stem Vancouver B2 and B3 type fractures with an uncemented modular fluted tapered stem (MRP-Titan). Demographic and radiographic parameters were analyzed. The survival rate (free of reoperation) was calculated at 2- and 5-years using the Kaplan–Meier survivorship analysis.
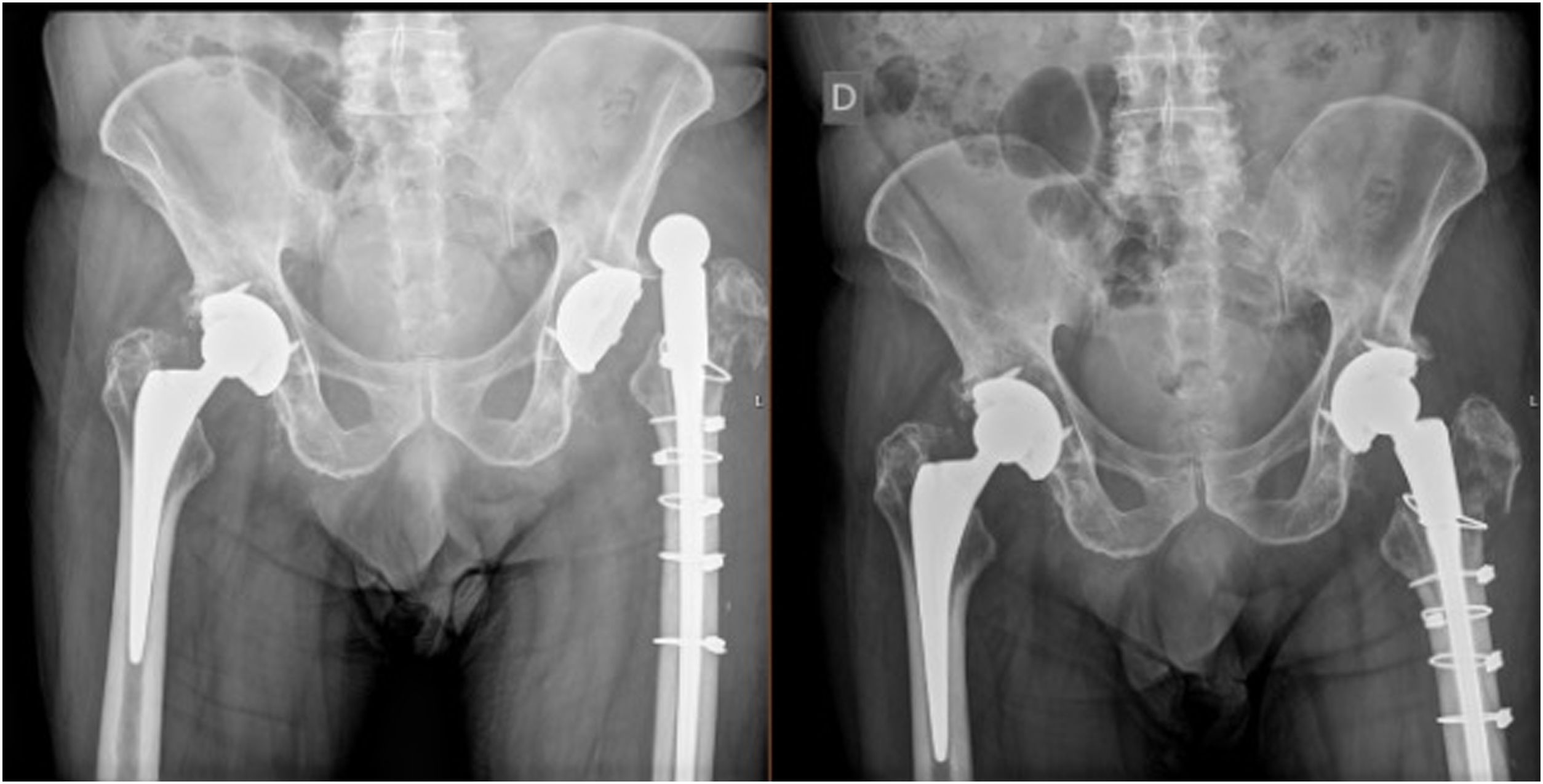
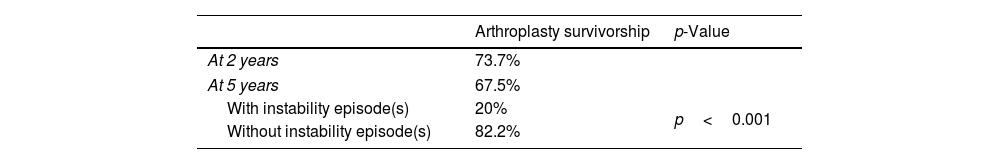
ResultsThirty-nine patients were included with a mean age of 73.5 years and a mean follow-up of 5 years. Arthroplasty survivorship at 2 years was 73.7% and at 5 years was 67.5% (mean 8.4 years; range 6.7–10.2). Survivorship was inferior in the patients with episodes of instability (mean 2.5 years; range 0–5.42) (p<0.001). At least one episode of instability occurred in 26.3% of patients and 60% of these patients had a femoral head size 32mm or lower. At least one episode of instability occurred in 71.4% of patients with a greater trochanter fracture (p=0.008). The consolidation rate was 90.6% and the mortality rate was 23.7%. In the group of patients that died, 55.6% were submitted to at least one revision surgery (p=0.044).
ConclusionSurvivorship of an uncemented modular stem (MRP-Titan) in revision for PHF is significantly reduced by episodes of instability.
Las fracturas periprotésicas de cadera muestran una incidencia creciente. Nuestro objetivo fue evaluar la supervivencia de los vástagos modulares cónicos no cementados en el tratamiento de las fracturas periprotésicas tipo Vancouver B2-B3 y revisar factores asociados a una menor supervivencia.
MétodosRealizamos un estudio retrospectivo de los pacientes sometidos a artroplastia de revisión para el tratamiento de fracturas tipo Vancouver B2-B3 con vástago cónico estriado modular no cementado (MRP-Titan). Se analizaron parámetros demográficos y radiográficos. La tasa de supervivencia (libre de reoperación) se calculó a los 2 y 5años mediante el análisis de supervivencia de Kaplan-Meier.
ResultadosSe incluyeron 39 pacientes con una edad media de 73,5años y un seguimiento medio de 5años. La supervivencia a los 2años fue del 73,7%, y a los 5años, del 67,5% (media 8,4años; rango 6,7-10,2). El 26,3% de los pacientes tuvieron al menos un episodio de inestabilidad y su supervivencia fue inferior (p<0,001) (media 2,5años; rango 0-5,42). De estos pacientes, el 60% tenían un tamaño de la cabeza femoral de 32mm o inferior. El 71,4% de los pacientes con fractura del trocánter mayor presentaron al menos un episodio de inestabilidad (p=0,008). La tasa de consolidación fue del 90,6% y la tasa de mortalidad fue del 23,7%. En el grupo de pacientes que fallecieron, el 55,6% fueron sometidos al menos a una cirugía de revisión (p=0,044).
ConclusionesLa supervivencia de un vástago modular no cementado (MRP-Titan) en revisión por FPH se reduce significativamente por episodios de inestabilidad.
Hip arthroplasty remains as one of the most successful surgeries, with great clinical results.1,2 With the increase in global life expectancy and expanding indications in younger patients, the number of active patients with hip arthroplasties is rapidly rising.3,4 Consequently, periprosthetic hip fractures (PHF) (Fig. 1) emerge as a burden5 for health care services and patients as they represent significant morbidity and mortality.6
Abdel et al.3 in a review of 32644 primary total hip arthroplasties, found a 3% incidence rate of intra-operative periprosthetic femoral fractures in uncemented stems, 14 times more often than in cemented ones. In the same study, the cumulative probability of fracture at 20 years was 7.7% for uncemented and 2.1% for cemented stems. In revision surgery, the frequency is significantly greater, around 6%.4
Patients’ characteristics, surgical technique and type of stem fixation are known factors that influence the incidence of this complication. Older age and presence of osteoporosis are identified demographic risk factors.7
PHF around the stem can be treated according to the stem stability status with osteosynthesis in a well-fixed stem (Vancouver classification8 type B1) or with stem revision in loose stems (B2 or B3).6 Osteosynthesis in loose stems may be reserved for patients with significant comorbidities although with higher revision rates, according to some authors.6,9 There are multiple revision stems available, ranging from cemented to uncemented stems, fully coated monoblock systems or modular tapered stems.6,10,11 Survivorship of revision arthroplasty using uncemented modular tapered stems in the context PHF has not been completely studied. This remains a complex surgery requiring specially trained surgeons and is still linked to high morbidity.12,13
The main purpose of this study was to evaluate the survival of an uncemented modular tapered stem in the treatment of periprosthetic Vancouver B2 and B3 type fractures. A secondary goal was to review the main complications and factors associated with decreased survival.
Materials and methodsWe conducted a retrospective study of patients submitted to revision arthroplasty for treatment of periprosthetic femoral stem fractures. We reviewed all patients admitted at our Institution between 2010 and 2020 with periprosthetic Vancouver B2 and B3 type fractures and included all patients treated with revision arthroplasty with an uncemented modular fluted tapered stem (Fig. 2). Patients with less than a year of follow-up or submitted to osteosynthesis were excluded. Patients treated with simultaneous acetabular revision were also excluded. The study was approved by the Ethics Committee of our centre. As this was a retrospective observational study, exemption from informed consent was obtained.
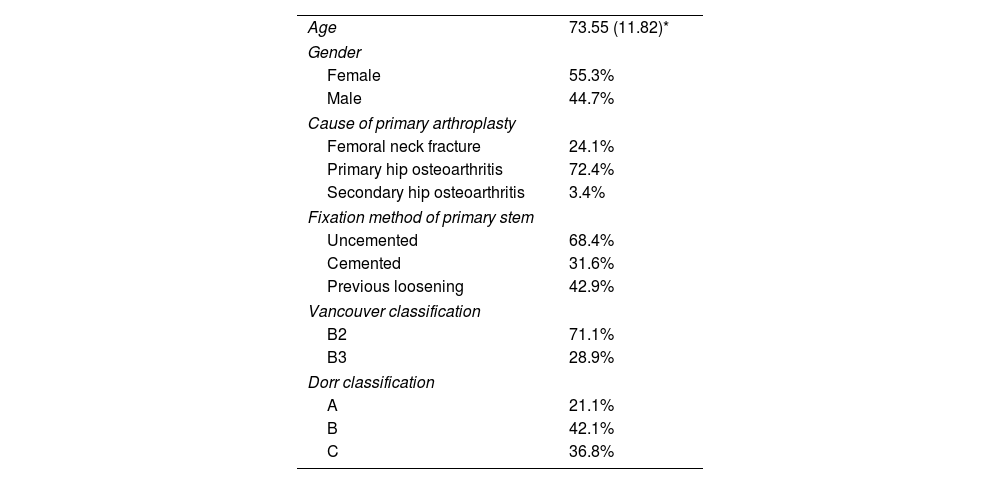
Demographic data like gender, age, cause for primary hip arthroplasty, type of stem fixation in the primary setting and time from primary arthroplasty to fracture were reported. The reoperation rate and causes, the number of instability episodes (defined as arthroplasty dislocation) and the infection rate were also registered. This study included 39 patients with a mean age of 73.5 years, with 55.3% of the female sex, and a mean follow-up period of 62 months (range 12–180 months) (Table 1).
Demographic characteristics and preoperative assessment.
| Age | 73.55 (11.82)* |
| Gender | |
| Female | 55.3% |
| Male | 44.7% |
| Cause of primary arthroplasty | |
| Femoral neck fracture | 24.1% |
| Primary hip osteoarthritis | 72.4% |
| Secondary hip osteoarthritis | 3.4% |
| Fixation method of primary stem | |
| Uncemented | 68.4% |
| Cemented | 31.6% |
| Previous loosening | 42.9% |
| Vancouver classification | |
| B2 | 71.1% |
| B3 | 28.9% |
| Dorr classification | |
| A | 21.1% |
| B | 42.1% |
| C | 36.8% |
All cases were revised using a posterolateral approach in lateral decubitus, recurring to a transfemoral approach (extended trochanteric osteotomy) for stem or cement removal when needed.
In cases in which femoral stem was considered fixed intra-operatively (Vancouver B1 instead of B2), fracture osteosynthesis was performed instead of revision arthroplasty.
The stem used for revision was the MRP-Titan (Peter Brehm, Weisendorf, Germany). This is an uncemented modular tapered stem which consists of a distally fixed stem with variable lengths available, a metaphyseal section for limb length adjustment and a neck portion with normal and lateralized options that permits 360° of version adjustment for higher versatility. The titanium stem has longitudinal ribs that promotes bone ingrowth, preservation of bone stock and immediate rotational stability. The stem-neck coupling is made using a morse taper junction in conjunction with a torque-specific bolt.
In cases of where great trochanter (GT) fracture was present, plate or cables osteosynthesis was added according to the surgeon's decision.
In the immediate post operative, it was allowed immediate toe touch weight bearing with progressive progression to partial weight bearing as tolerated. Radiographic control was performed immediately post operatively during the hospital stay, at the two weeks consultation, at three, six and twelve months.
Radiographic analysisThe preoperative, immediate post operative and at the last follow-up visit radiographs were reviewed by the authors. The Vancouver classification and the Dorr classification were applied, leg length discrepancy (LLD), centre of rotation offset (COR offset), fracture union, presence GT fracture and presence of signs of stem loosening prior to fracture were also noted. LLD was measured using the method described by Ranawat14 as the vertical distance between the inter-teardrop line and the apex of the lesser trochanter; COR offset was measured as the perpendicular distance from the centre of rotation of the femoral head and a line bisecting the femoral diaphysis. Stem subsidence was calculated as Parry et al.,15 by subtracting the distance from the tip of the stem to a fixed point on the femur (like the nearest cable) between the last follow-up radiograph and the immediate post operative. Stem subsidence was considered significant when the difference was >5mm.15–17 The distance the stem bypassed the fracture was also determined by measuring in the immediate post operative radiograph the distance of tip of the stem to the most distal part of the fracture and calculating a ratio by dividing it by the diameter of the femur in the zone of the fracture.15 No acetabular component analysis was performed.
Statistical analysisChi-square analysis was used for determination of differences between nominal variables and parametric tests for continuous variables with normal distribution. Paired t test analysis was used for paired continuous variables with normal distribution and non-parametric tests were used for variables with non-normal distribution.
The survival rate (free of reoperation) was calculated at 2- and 5-years using the Kaplan–Meier survivorship analysis, and log-rank and Wilcoxon tests were performed to determine significant difference in implant survivorship between groups. All tests used a significance level of α=0.05. Statistical analysis was performed using IBM SPSS Statistics version 28.0.1.
ResultsThe overall cumulative proportion of arthroplasty survivorship (free of reoperation) was 73.7%% at 2 years and 67.5% at 5 years (mean 8.4 years; standard error (SE) 0.9; 95% confidence interval (CI), range 6.7–10.2). In the patients with episodes of instability the cumulative proportion of survivorship was 20% at 5 years (mean 2.5 years; (SE) 1.5; 95% (CI), range 0–5.42), significantly inferior to patients without episodes of instability (log-rank test and Wilcoxon (p<0.001)) (Table 2).
At the end of the follow-up period, the consolidation rate was 90.6%.
The mean time from primary arthroplasty to fracture was 347 months and the primary diagnosis was femoral neck fracture in 24.1% of the cases and primary hip osteoarthritis in 72.4%. In 68.4% of the cases the stem was uncemented. At the time of PHF, most of the femurs were classified as Dorr B. Previous signs of loosening were present in 42.9% of the cases. According to the Vancouver classification, 71.1% of the fractures were B2 (Table 1).
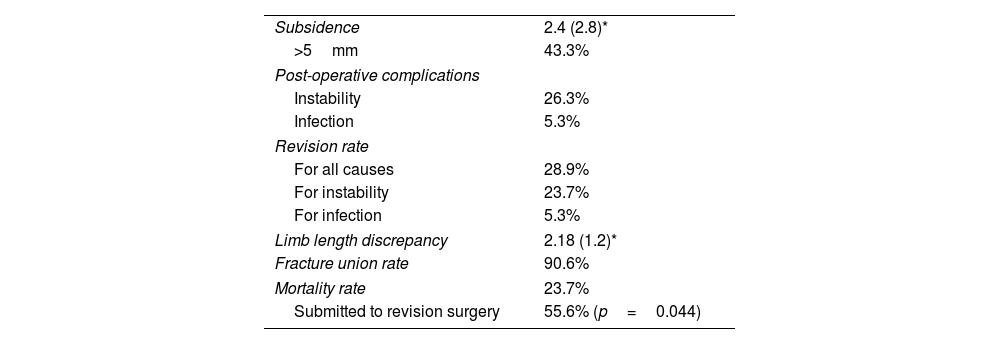
Stem subsidence >5mm occurred in 43.4% of the patients (mean 2.4±2.8cm), without difference for the studied variables (p>0.05) (Table 3). Limb length discrepancy was 2.18±1.2cm. The mean COR offset was inferior (p<0.001) in the operated hip (32.5±8.2mm) comparing to the contralateral hip (40.1±6.8mm), but COR offset was not significant for instability risk.
Postoperative radiographic assessment and complications analysis.
The revision rate for all causes was 28.9%. Twenty six percent of the patients had at least one episode of instability and the infection rate was 5.3%. In the subgroup of patients with an episode of dislocation (n=10), 6 patients (60%) had a 32-mm size head or lower, and 2 patients (20%) had a 36-mm head, 2 patients (20%) had no information regarding femoral head size.
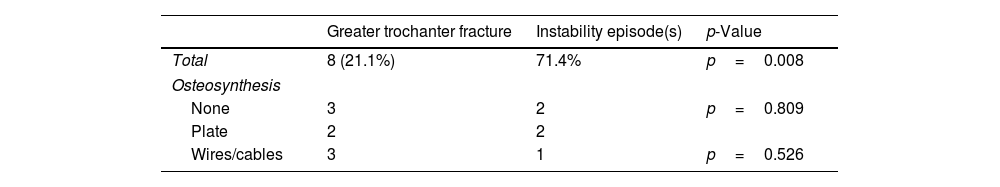
Seventy one percent of the patients with GT fracture had at least one episode of instability (p=0.008) (Table 4 and Fig. 3). Whether the GT fracture was fixed or not, as well as the type of fixation in those fixed, revealed no differences in instability rate (p>0.05).
The mortality rate was 23.7%. Death occurred at a mean of 25 months since the fracture. In the group of patients that died in the period of the study, 55.6% were submitted to at least one revision surgery (p=0.044).
DiscussionThe treatment of periprosthetic Vancouver B-type fractures remains a demanding task for the orthopaedic surgeon. The distinction between a well-fixed and a loose stem is challenging and sometimes only possible intra-operatively but influences the best treatment strategy.6 In Vancouver B2 and B3-types, several implants are available to revise the loose stem, with the aim to bypass the fracture and provide stability distally. Tapered fluted stems were initially introduced by Wagner18,19 in 1980s in a monoblock version. They allow axial stability by pressing the stem mainly in the diaphysis and isthmus after successive reaming and allow immediate rotational stability by the presence of flutes. Modularity of the diaphyseal–metaphyseal–neck junction was later introduced, adding versatility to the system.
The literature reports good survival of the uncemented modular fluted tapered stems, with survivorship reaching 90% at five years in some studies.20,21 Parry et al.15 found an 89% survival rate at five years in their series and Wirtz et al.22 even reported 97% survival rate at 10 years and 85% after 15 years. Survivorship free of reoperation for any cause in our study was significantly lower, with 67.5% at 5 years. Stem design may be a contributing factor for survival, but further studies comparing different stems designs are needed.
Our revision rate for all causes was 28.9%. Lindahl et al.,23 reported a reoperation rate of 16.2%. This may be partially explained by the high dislocation rate encountered in our series, reaching 26.3% which significantly reduced survivorship (p<0.001).
Instability was higher than the reported in other studies, with values between 8% and 21%.24,25 Lindahl et al.,23 in their series of 425 patients treated with uncemented modular stems for femur periprosthetic fracture, reported a hip dislocation rate of 5.4%. Abdel et al.,24 reported instability as the most common complication in their series of 44 patients, with a rate of 11%. The metaphyseal–neck junction with 360° of version adjustment of this stem has been proposed to improve versatility and stability, but higher instability rates suggest that this feature may not be sufficient to prevent dislocation.
They suggested using larger femoral head diameters, noting that dislocations occurred in patients with 28mm and 32mm. This study reported similar findings, in which 60% of the patients with instability had a femoral head size 32mm or lower. In fact, bigger size femoral heads are described in the literature as offering more stability, by increasing the jump distance26 at the expense of increased polyethylene wear. Recent studies reported good results with the use of dual mobility cups for increasing stability in high-risk patients like in the setting of revision arthroplasty,27,28 although specific studies for revision for periprosthetic fracture are lacking. In fact, dual mobility cups have been linked to increased incidence of periprosthetic fracture in primary hip arthroplasties.29
The presence of great trochanter fracture was a key variable in instability, with 71.4% of the patients with GT fracture having at least one episode of instability (p=0.008). Interestingly, performing GT osteosynthesis and the various types of osteosynthesis used revealed no differences in the instability risk (p>0.05). Despite the GT fracture being a well-established risk factor for instability,11,30 this finding brings further ominous significance to this lesion (Fig. 4). GT fracture osteosynthesis is often difficult due to fracture displacement by the pull of the gluteal muscles30 and poor bone stock, as these fractures are frequently associated with osteolysis.11
Acetabular cup revision was not performed at the index surgery, which may further explain higher instability rates. Polyethylene eccentric wear is associated with osteolysis and aseptic loosening31 and may contribute to instability. Acetabular component position was also not corrected.
Stem subsidence occurred in 43.4% of the patients, but we found no differences in the factors studied. Parry et al.15 found higher amounts of subsidence in Dorr C femurs and in patients with use of strut grafts, proxies for host bone stock deficiency. In this study, proposed risk factors for subsidence like female gender, fracture classification, stem diameter or length, or fracture bypass ratio did not reach statistically significance. Abdel et al.16 in their study observed a trend for higher subsidence in patients with greater femoral bone loss, in patients submitted to aseptic loosening revision. In fact, stem subsidence risk factors are still not well-established in the literature. Furthermore, its clinical significance remains not clearly defined. In our study, although almost half of the patients registered stem subsidence >5mm, no association with instability or limb length discrepancy was found (p>0.05).
COR offset restoration is a critical step in hip arthroplasty, with the aim to preserve hip abductors and external rotators’ function and limb length. We found an inferior COR offset (p<0.001) in the revised operated hip comparing to the contralateral hip. Although this may be expected because in revision setting the COR offset preservation is a difficult task, this fact may contribute for decrease survival and higher instability (although without reaching statistical significance).
The union rate of this type of fracture is reported in the literature to be around 90–100%,32–34,35 like what was found in this study.
A significant finding in our study was the association between revision surgery and increased mortality. The mortality rate found in our series was 23.7% at 2 years. In fact, various studies report the mortality of PHF patients to be similar of those with native proximal femur fracture. The demographic characteristics of these two groups are similar, with mean ages above 70 years old, mostly females and with comorbidities. In fact, patients’ characteristics in our series are similar with the reported in most literature,3,4,6,7 a predominantly female sample with a mean age of 73.5 years with uncemented primary femoral stems. Most of the patients who died during the study (55.6%) sustained at least one revision surgery, with significantly superior mortality in this group (p=0.044). Although the causes for death were not recorded due to lack of data, the revision surgery appears as an important risk factor for mortality.
This study presents some limitations. The retrospective design limits the amount and quality of data that could be evaluated. Functional outcomes were not taken in consideration as a clinical evaluation was not performed, only the data extracted from the clinical files. The short follow-up period was due to loss of follow-up or death but precludes conclusions beyond 5 years.
The lack of acetabular component revision and radiographic analysis is another limitation, as this also contributes to instability and revision survivorship.
Further studies with longer follow-up and clinical outcomes evaluation are in need for additional knowledge in treating such injuries.
ConclusionSurvivorship of this design of uncemented modular stem in revision for PHF is significantly reduced by episodes of instability. PHF treatment with this stem present good union but high instability rates. The use of higher diameter femoral heads and preservation of the greater trochanter may improve results.
Complications and mortality rate are still high and treating these fractures remains a complex task that should be reserved for experienced multidisciplinary teams.
Level of evidenceLevel of evidence II.
Ethical approvalThis study was approved by the Ethics Committee of our centre.
Informed consentAs this was a retrospective observational study, exemption from informed consent was obtained.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone declared.