In orthopaedic surgery, it is clear that an optimal standardised closure technique has not yet been developed. Locally, there are no objective data describing the standard surgical practice in wound closure. The aim of this study is to analyse the clinical practice of surgical wound closure in orthopaedic surgery by means of a survey of a representative local sample and thus obtain information on the context of closure in Spain.
Material and MethodAn ad hoc group of specialists in orthopaedic surgery and traumatology was formed. The group of experts, after analyzing the literature, developed a questionnaire of 32 closed multiple-choice questions divided into the following blocks: hemostasis, surgical wound closure (deep, superficial, and cutaneous), and dressings.
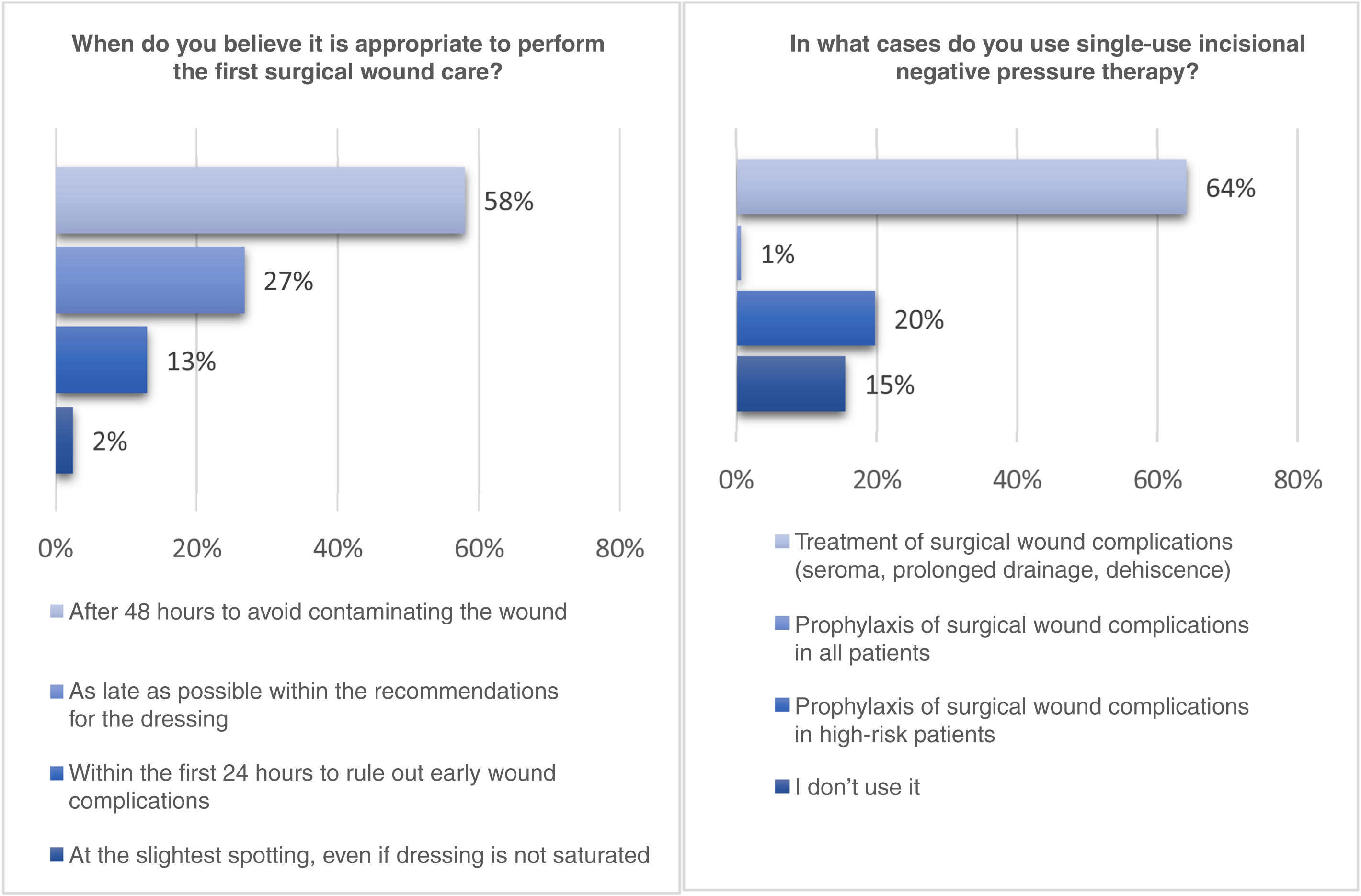
ResultsA total of 471 surgeons responded to the survey completely and with sufficient information to perform the descriptive analysis. 79% believe that ATX can influence the decrease in surgical site infection rate. 96% believe that the type of deep closure at the level of the arthrotomy could influence outcomes and complications after hip and/or knee replacements. 85% believe that the type of shallow closure at the subcutaneous level may influence outcomes and complications after hip and/or knee replacement. 64% of surgeons use single-use incisional negative pressure therapy for the treatment of surgical wound complications (seroma, prolonged drainage, dehiscence).
ConclusionsThere is a high level of variability in wound closure in our setting and a low level of training on the subject. The authors recommend that the different scientific societies invest resources to improve training in this field and reduce the percentage of surgeons who are considered inadequately trained, as well as adapting closure techniques to those considered gold standard according to the evidence.
En cirugía protésica de rodilla (PTR) y cadera (PTC) está claro que aún no se ha desarrollado una técnica de cierre estandarizada óptima. A nivel local no existen datos que describan la práctica quirúrgica habitual en cierre de herida. El objetivo de este trabajo es analizar el cierre de herida en cirugía protésica a través de una encuesta sobre una muestra representativa a nivel nacional y así obtener información sobre el contexto del cierre en España.
Material y métodoEl estudio se conforma de un grupo ad hoc de especialistas en cirugía protésica. El grupo de expertos, posterior al análisis de la literatura, elabora un cuestionario de 32 preguntas cerradas de opción múltiple, divididas en los siguientes bloques: hemostasia, cierre quirúrgico de la herida y apósitos.
ResultadosUn total de 471 cirujanos respondieron la encuesta de forma completa y con información suficiente para efectuar el análisis descriptivo; de estos, 79% cree que el ácido tranexámico (ATX) puede influir en la disminución de tasa de infección de sitio quirúrgico; por otro lado, 96% piensa que el tipo de cierre profundo a nivel de la artrotomía podría influir en los resultados y complicaciones tras prótesis de cadera y/o rodilla; mientras, 85% considera que el tipo de cierre superficial a nivel subcutáneo es el que puede influir en los resultados y las complicaciones después de prótesis de cadera y/o rodilla; de los cirujanos, 64% utiliza la terapia de presión negativa incisional de simple uso para el tratamiento de las complicaciones de la herida quirúrgica (seromas, drenaje prolongado, dehiscencias).
ConclusionesExiste en nuestro entorno una alta variabilidad en el cierre de la herida y una baja inversión en formación sobre este tema. Los autores recomiendan a las diferentes sociedades científicas la inversión de recursos para mejorar la formación en dicho campo y reducir el porcentaje de cirujanos que se consideran inadecuadamente formados, así como adaptar las técnicas de cierre a aquellas estimadas patrón oro según la evidencia.
In Spain, according to data published by the Ministry of Health regarding surgical procedures by speciality in 2020, 1,219,639 operations were performed in orthopaedic surgery and traumatology at a rate of 257.57 per 10,000 inhabitants, which, together with general and digestive surgery (rate of 235.22 per 10,000 inhabitants), makes them the most common at the national level.1
Surgical wounds in prosthetic surgery differ from wounds in other surgical fields in a number of aspects. These include the presence, in most cases, of an orthopaedic implant, the existence of highly contused tissues due to the trauma itself, and the fact that, more often than not, prosthetic surgery is performed on patients with many comorbidities and a high risk of complications.1 Despite multiple studies and promising advances in this field, it is clear that an optimal standardised closure technique has yet to be developed.2
Optimising wound closure can contribute to reducing postoperative adverse events, such as surgical site or periprosthetic infection, improving patient functional recovery, and potentially lowering healthcare costs and healthcare resource use.3,4
Given the substantial variability of the surgical wound in prosthetic surgery, similar diversity in the approach and management of this wound is to be expected.1 Nevertheless, there are no local objective data that describe the average standard surgical practice in wound closure, and thereby contrast practice against current recommendations for approach in this field.
The aim of this paper is to analyse the clinical practice of surgical wound closure in prosthetic surgery by means of a survey of a nationally representative sample, so as to glean information concerning the context of wound closure in Spain. In addition, the findings may represent a starting point from which to explore future changes in how closure is performed as recommendations and management guidelines are published as well as to assess compliance with such publications, similar to the PREVENCOT5 project on surgical wound infection prevention. Furthermore, the results of this study can highlight the need to standardise wound closure in prosthetic surgery on the basis of the best evidence available in the form of guidelines or consensus papers.
MethodologyIn order to prepare the survey, an ad hoc group was formed of specialists in orthopaedic surgery and traumatology, with extensive expertise in prosthetic surgery. After a review of the literature and the critical steps of the closure procedure, the group of experts developed a questionnaire of 32 closed multiple-choice questions divided into the following categories:
- •
Haemostasis
- •
Surgical wound closure (deep plane, superficial, and cutaneous)
- •
Dressing
The survey was generated using specific software (BSJ.plus, Valladolid, Spain) and sent via the database of the Spanish Society of Orthopaedic Surgery and Trauma Medicine (SECOT) from 15 February 2021 to 3 March 2021.
With the results received, a descriptive analysis of the results was conducted to determine the trends in wound closure in prosthetic surgery in Spain and to extract the most representative characteristics of the dataset.
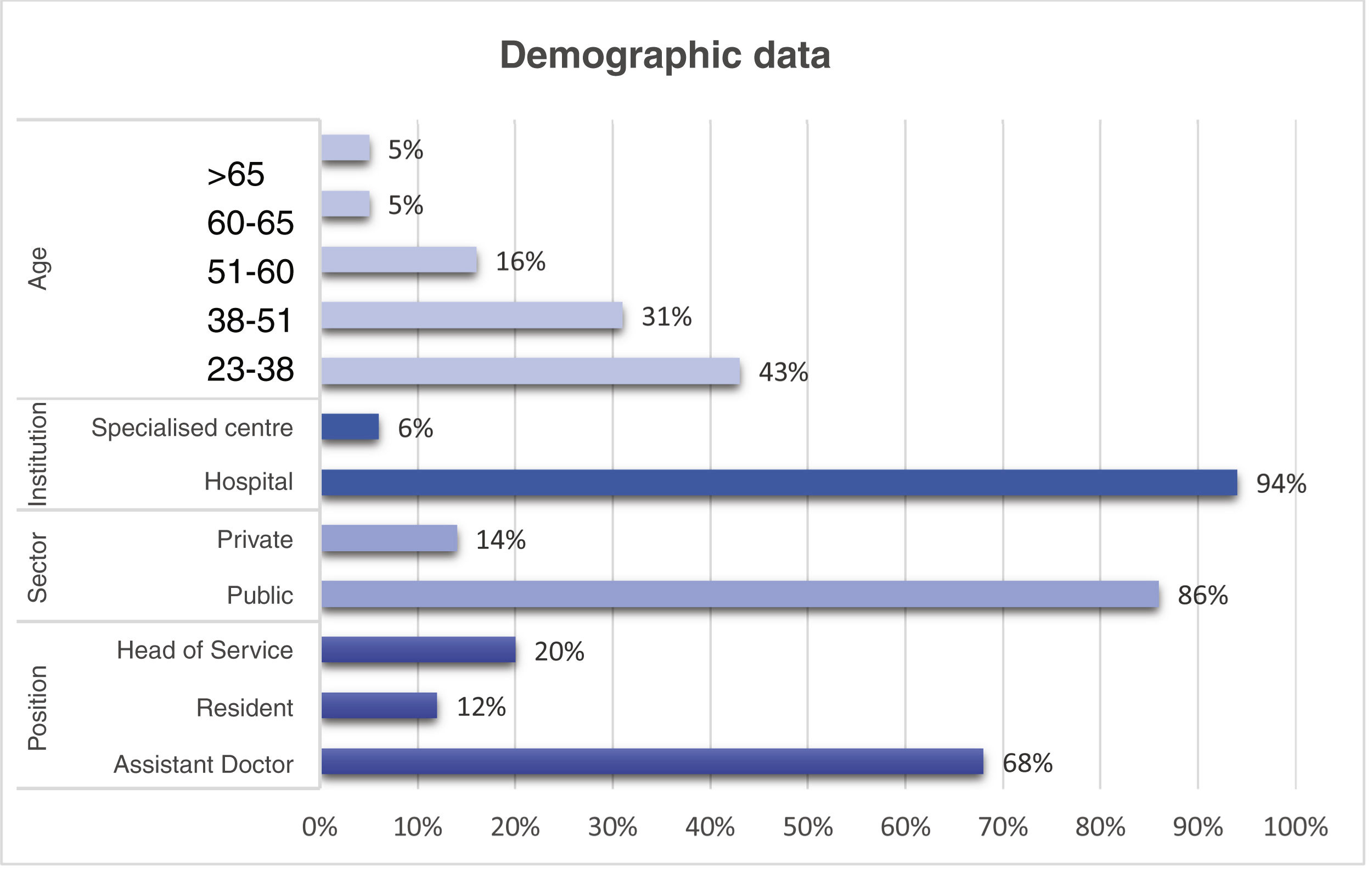
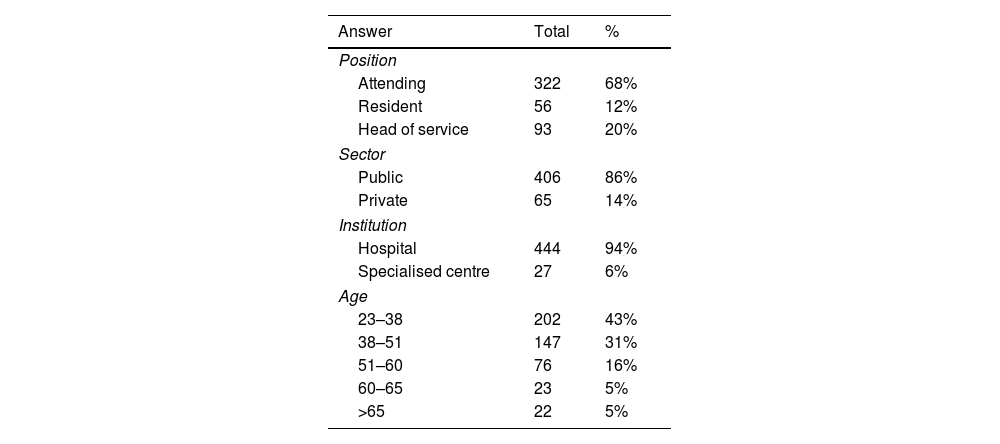
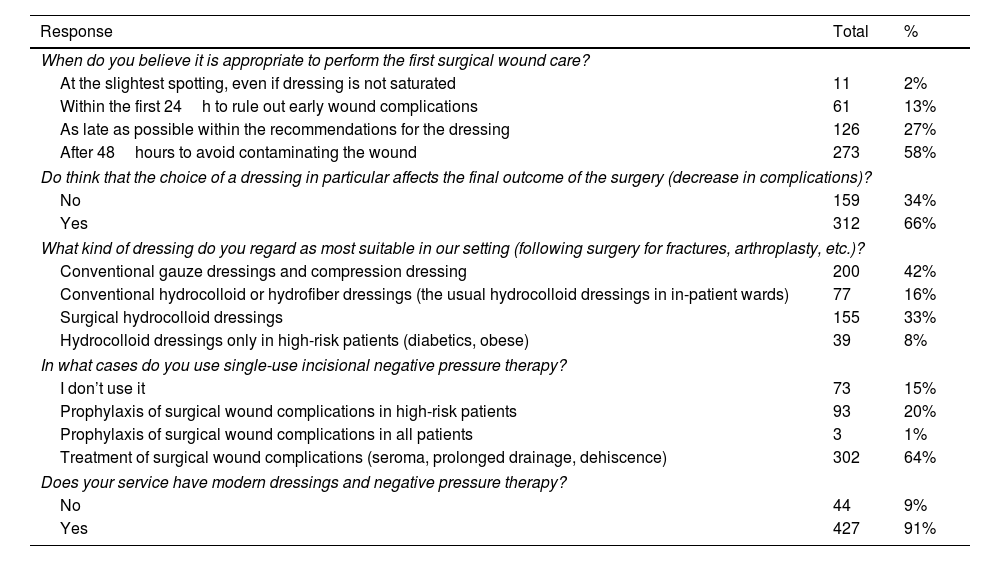
ResultsA total of 471 surgeons fully completed the survey with enough information to allow for descriptive analysis; 68% are attendings, 20% are residents, and 12% are heads of service. Eighty-six percent (86%) of the responses were from surgeons practising in the public sector; 74% of the respondents were between the ages of 23 and 51 years. The description of the sample is depicted in Table 1 and Fig. 1.
- •
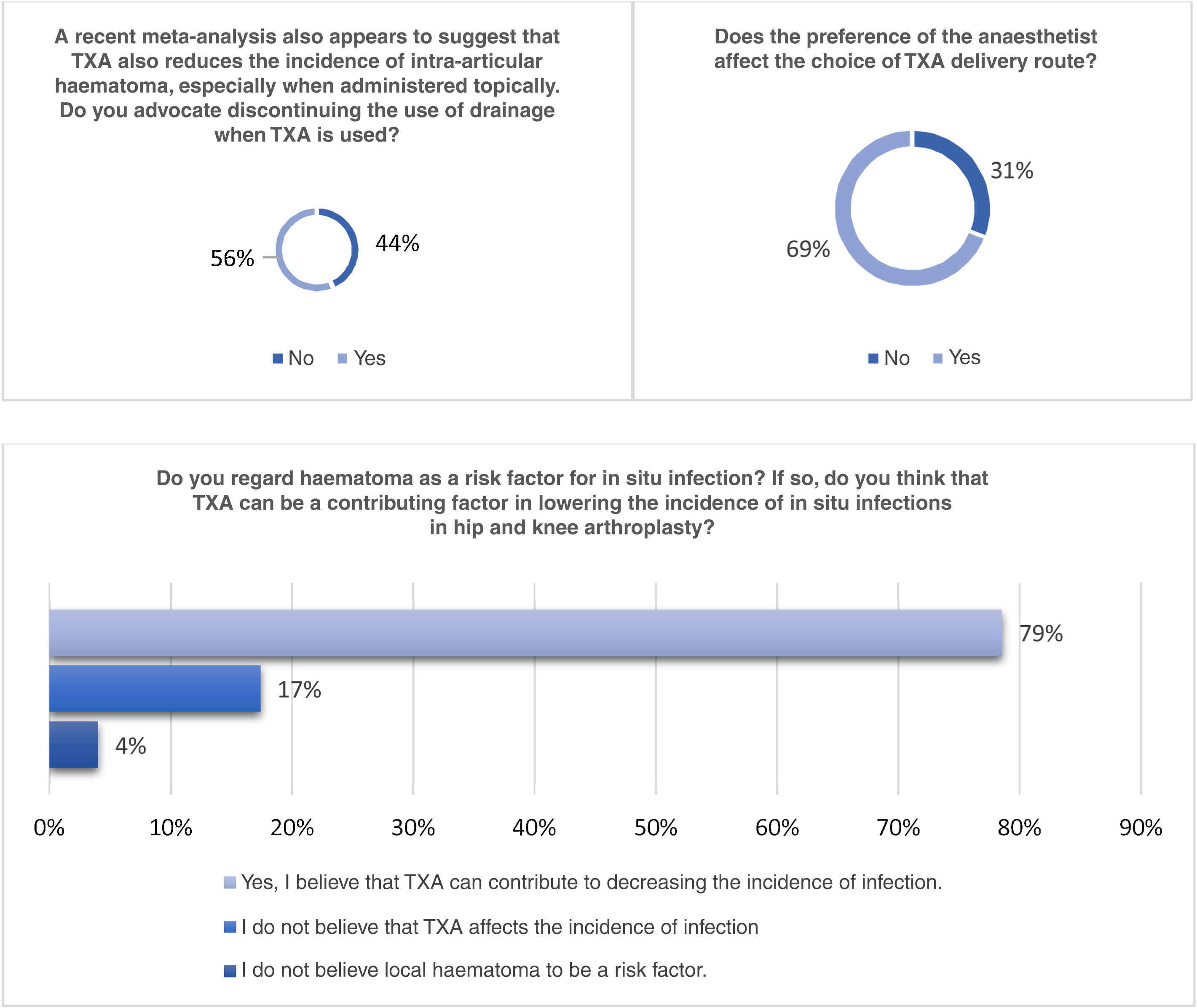
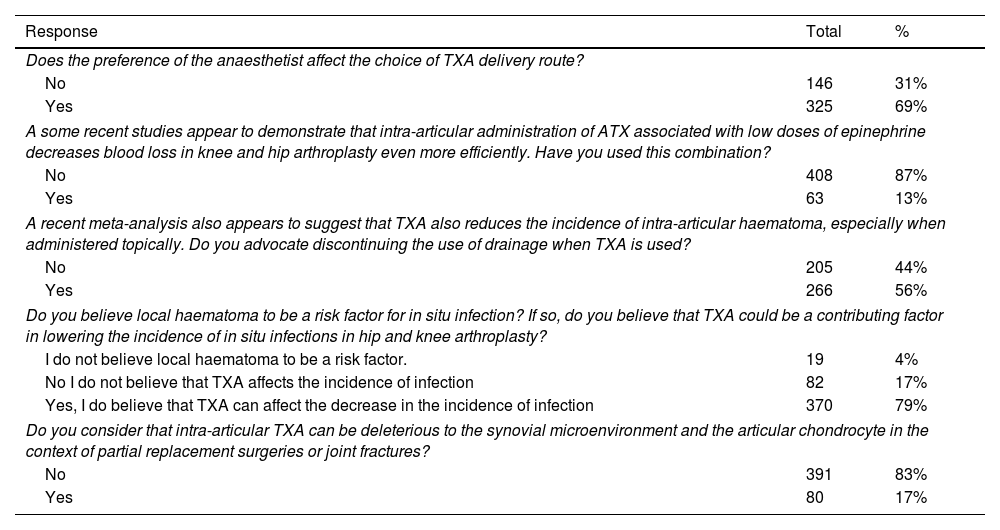
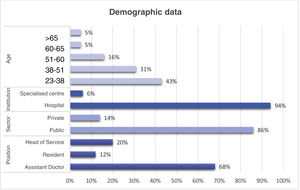
Sixty-nine percent (69%) believe that the anaesthesiologist's preferences impact the non-administration of tranexamic acid (TXA) (Fig. 2).
- •
Eighty-seven percent (87%) has not used the intra-articular combination of TXA associated with a low dose of epinephrine.
- •
Fifty-six percent (56%) advocates not continuing to use a drain when TXA is administered.
- •
Seventy-nine percent (79%) believe that TXA can contribute to decreasing the rate of surgical wound infection rate.
- •
Eighty-three percent (83%) do not believe that intra-articular TXA can be deleterious to the synovial microenvironment and the articular chondrocyte in the context of partial replacement surgeries or joint fractures.
- •
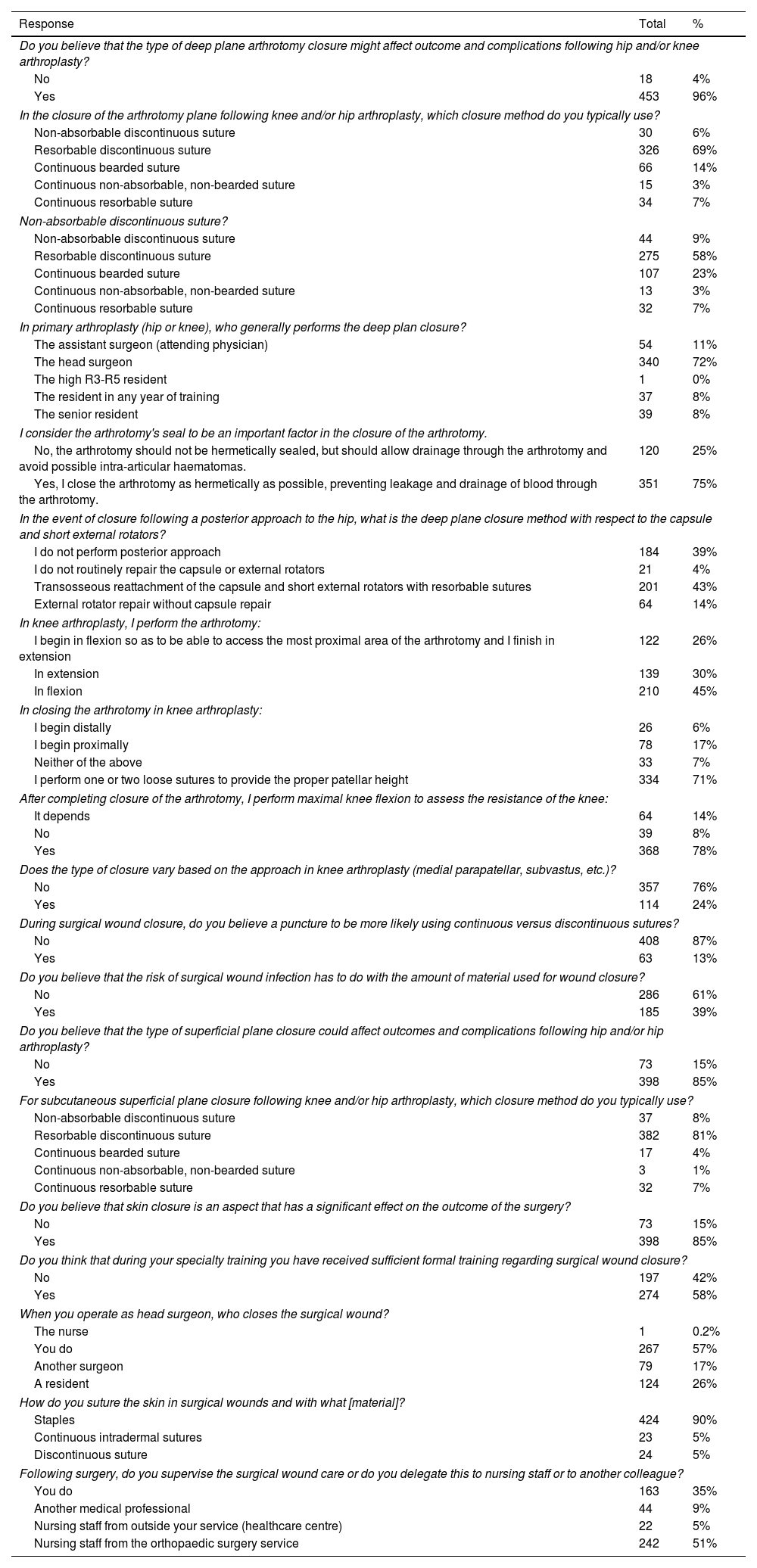
Ninety-six percent (96%) believe that the type of deep plane closure of the arthrotomy could affect the results and complications following hip and/or knee prosthetics.
- •
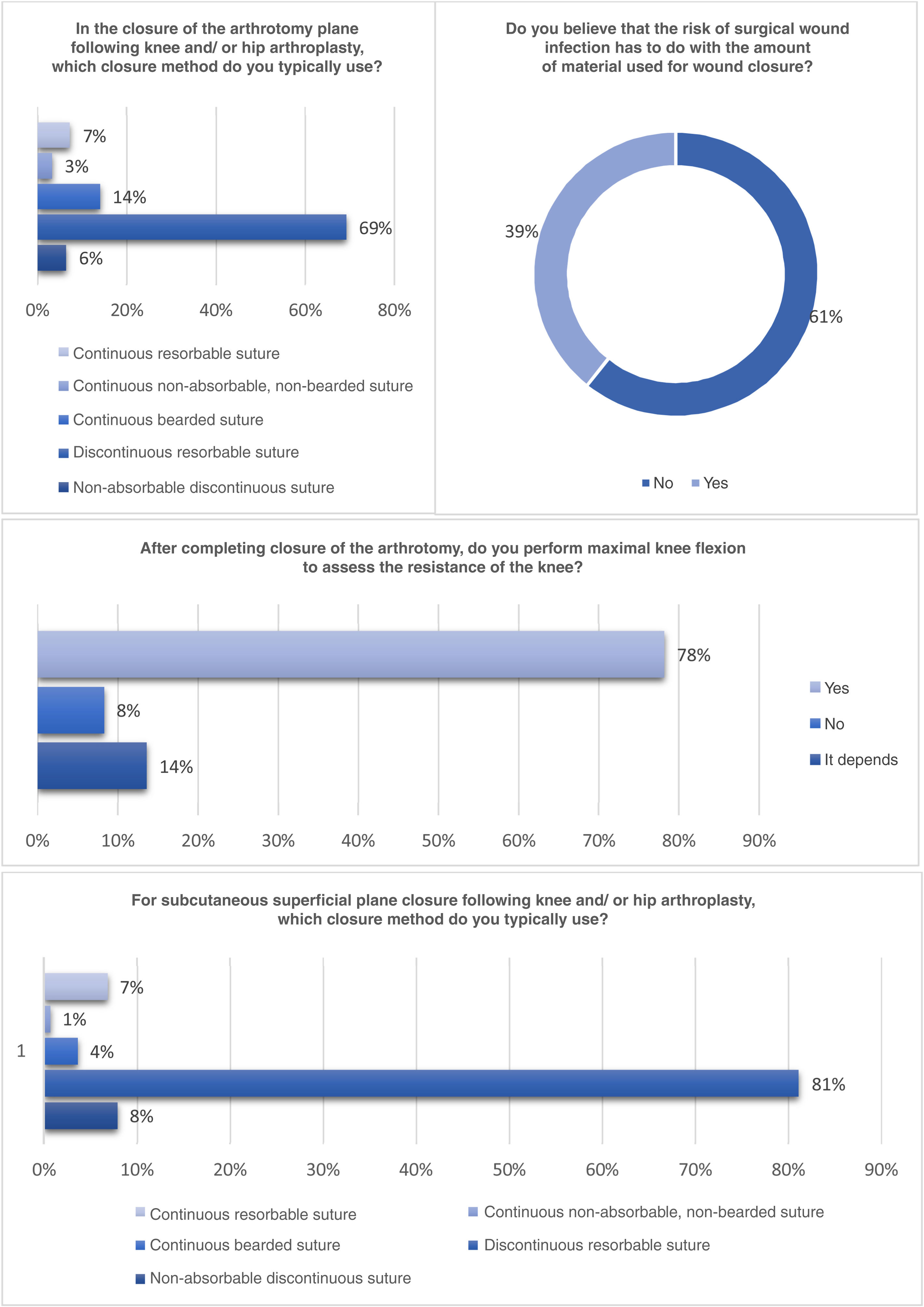
Sixty-nine percent (69%) of the surgeons close the arthrotomy plane of the knee and/or hip with resorbable discontinuous sutures; 14% close with continuous barbed suture.
- •
Fifty-eight percent (58%) deem resorbable discontinuous sutures to be the ideal closure type for the arthrotomy plane in knee and/or hip surgery.
- •
Twenty-three percent (23%) believe that continuous barbed sutures to be the optimal means of closure.
- •
In primary hip or knee prosthetic surgery, the lead surgeon closes the deep plane in 72% of the cases; in 11% of the cases, it is performed by the assistant surgeon.
- •
Seventy-five percent (75%) of the respondents close the arthrotomy as hermetically as possible, keeping blood from leaking and draining through the wound.
- •
Twenty-five percent (25%) consider arthrotomy should not be closed hermetically and that drainage should be allowed to occur through the close and avoid possible intra-articular haematoma.
- •
In the event of closure following a posterior approach to the hip, 43% perform transosseous capsular reattachment and short external rotators with resorbable sutures; 39% do not perform posterior approach, and 14% repair rotators without capsular repair.
- •
In prosthetic knee surgery, 45% of the surgeons close in flexion, 30% in extension, and 26% initiate closure in flexion and finish in extension.
- •
In knee arthrotomy closure, 71% of surgeons perform one or two loose stitches to provide proper patellar height; 17% begin proximally.
- •
Seventy-eight (78%) of the respondents perform maximum knee flexion to check the strength of the knee once the arthrotomy closure has been completed.
- •
Eighty-seven percent (87%) consider that they are no more likely to suffer a puncture using continuous or discontinuous sutures or loose stitches.
- •
Sixty-one percent (61%) do not believe that the risk of surgical wound infection has anything to do with the amount of material used for wound closure.
- •
Eighty-five percent (85%) believe that the type of subcutaneous surface closure can have a bearing on outcomes and complications after hip and/or knee replacements.
- •
In subcutaneous surface plane closure post knee and/or hip replacement, 81% use resorbable discontinuous stitches for suturing.
- •
Eighty-five percent (85%) deem skin closure to be an aspect that significantly affects post-operative outcome.
- •
Forty-three percent (43%) of the surgeons state that they do not perform the closure of their operations themselves (with a resident, another surgeon, or a nursing staff member performing the closure of the surgical wound).
- •
Forty-two percent (42%) of the surgeons believe that they have not received sufficient formal training in surgical wound closure during the course of their speciality training.
- •
In 57% of the cases, the first surgeon performs the cutaneous closure of the surgical wound.
- •
Ninety percent (90%) of the surgeons use staples to close the surgical wounds in prosthetic surgery.
- •
Fifty-one percent (51%) report that the nursing staff of the Orthopaedic Surgery and Traumatology Department supervises post-operative wound care.
The most representative results obtained in the category addressing wound closure are summarised in Fig. 3.
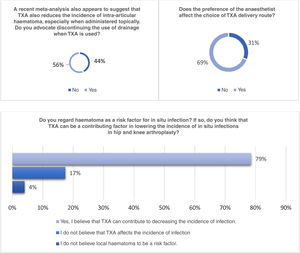
Dressing (Fig. 4)- •
Fifty-eight percent (58%) of the respondents believe it is appropriate to perform the first surgical wound care after 48h to keep the wound from becoming contaminated; 27% feel that the first wound care should be performed as late as possible within the dressing recommendations (Fig. 4).
- •
Sixty-six percent (66%) of the surgeons think that the choice of a dressing in particular affects the final outcome of the surgery.
- •
Forty-two percent (42%) regard conventional gauze dressings and compressive bandages to be the most suitable in our setting.
- •
Thirty-three percent (33%) believe that surgical hydrocolloid dressings are the most appropriate.
- •
Sixty-four percent (64%) of the respondents use simple incisional negative pressure therapy to treat surgical wound complications (seroma, prolonged drainage, dehiscence).
- •
Ninety-one percent (91%) of the surgeons have modern dressings and negative pressure therapy devices in their departments.
Tables 2–4 present the comprehensive results of the survey.
Results of haemostasis block according to the survey.
| Response | Total | % |
|---|---|---|
| Does the preference of the anaesthetist affect the choice of TXA delivery route? | ||
| No | 146 | 31% |
| Yes | 325 | 69% |
| A some recent studies appear to demonstrate that intra-articular administration of ATX associated with low doses of epinephrine decreases blood loss in knee and hip arthroplasty even more efficiently. Have you used this combination? | ||
| No | 408 | 87% |
| Yes | 63 | 13% |
| A recent meta-analysis also appears to suggest that TXA also reduces the incidence of intra-articular haematoma, especially when administered topically. Do you advocate discontinuing the use of drainage when TXA is used? | ||
| No | 205 | 44% |
| Yes | 266 | 56% |
| Do you believe local haematoma to be a risk factor for in situ infection? If so, do you believe that TXA could be a contributing factor in lowering the incidence of in situ infections in hip and knee arthroplasty? | ||
| I do not believe local haematoma to be a risk factor. | 19 | 4% |
| No I do not believe that TXA affects the incidence of infection | 82 | 17% |
| Yes, I do believe that TXA can affect the decrease in the incidence of infection | 370 | 79% |
| Do you consider that intra-articular TXA can be deleterious to the synovial microenvironment and the articular chondrocyte in the context of partial replacement surgeries or joint fractures? | ||
| No | 391 | 83% |
| Yes | 80 | 17% |
TXA: tranexamic acid.
Results of the closure block according to the survey.
| Response | Total | % |
|---|---|---|
| Do you believe that the type of deep plane arthrotomy closure might affect outcome and complications following hip and/or knee arthroplasty? | ||
| No | 18 | 4% |
| Yes | 453 | 96% |
| In the closure of the arthrotomy plane following knee and/or hip arthroplasty, which closure method do you typically use? | ||
| Non-absorbable discontinuous suture | 30 | 6% |
| Resorbable discontinuous suture | 326 | 69% |
| Continuous bearded suture | 66 | 14% |
| Continuous non-absorbable, non-bearded suture | 15 | 3% |
| Continuous resorbable suture | 34 | 7% |
| Non-absorbable discontinuous suture? | ||
| Non-absorbable discontinuous suture | 44 | 9% |
| Resorbable discontinuous suture | 275 | 58% |
| Continuous bearded suture | 107 | 23% |
| Continuous non-absorbable, non-bearded suture | 13 | 3% |
| Continuous resorbable suture | 32 | 7% |
| In primary arthroplasty (hip or knee), who generally performs the deep plan closure? | ||
| The assistant surgeon (attending physician) | 54 | 11% |
| The head surgeon | 340 | 72% |
| The high R3-R5 resident | 1 | 0% |
| The resident in any year of training | 37 | 8% |
| The senior resident | 39 | 8% |
| I consider the arthrotomy's seal to be an important factor in the closure of the arthrotomy. | ||
| No, the arthrotomy should not be hermetically sealed, but should allow drainage through the arthrotomy and avoid possible intra-articular haematomas. | 120 | 25% |
| Yes, I close the arthrotomy as hermetically as possible, preventing leakage and drainage of blood through the arthrotomy. | 351 | 75% |
| In the event of closure following a posterior approach to the hip, what is the deep plane closure method with respect to the capsule and short external rotators? | ||
| I do not perform posterior approach | 184 | 39% |
| I do not routinely repair the capsule or external rotators | 21 | 4% |
| Transosseous reattachment of the capsule and short external rotators with resorbable sutures | 201 | 43% |
| External rotator repair without capsule repair | 64 | 14% |
| In knee arthroplasty, I perform the arthrotomy: | ||
| I begin in flexion so as to be able to access the most proximal area of the arthrotomy and I finish in extension | 122 | 26% |
| In extension | 139 | 30% |
| In flexion | 210 | 45% |
| In closing the arthrotomy in knee arthroplasty: | ||
| I begin distally | 26 | 6% |
| I begin proximally | 78 | 17% |
| Neither of the above | 33 | 7% |
| I perform one or two loose sutures to provide the proper patellar height | 334 | 71% |
| After completing closure of the arthrotomy, I perform maximal knee flexion to assess the resistance of the knee: | ||
| It depends | 64 | 14% |
| No | 39 | 8% |
| Yes | 368 | 78% |
| Does the type of closure vary based on the approach in knee arthroplasty (medial parapatellar, subvastus, etc.)? | ||
| No | 357 | 76% |
| Yes | 114 | 24% |
| During surgical wound closure, do you believe a puncture to be more likely using continuous versus discontinuous sutures? | ||
| No | 408 | 87% |
| Yes | 63 | 13% |
| Do you believe that the risk of surgical wound infection has to do with the amount of material used for wound closure? | ||
| No | 286 | 61% |
| Yes | 185 | 39% |
| Do you believe that the type of superficial plane closure could affect outcomes and complications following hip and/or hip arthroplasty? | ||
| No | 73 | 15% |
| Yes | 398 | 85% |
| For subcutaneous superficial plane closure following knee and/or hip arthroplasty, which closure method do you typically use? | ||
| Non-absorbable discontinuous suture | 37 | 8% |
| Resorbable discontinuous suture | 382 | 81% |
| Continuous bearded suture | 17 | 4% |
| Continuous non-absorbable, non-bearded suture | 3 | 1% |
| Continuous resorbable suture | 32 | 7% |
| Do you believe that skin closure is an aspect that has a significant effect on the outcome of the surgery? | ||
| No | 73 | 15% |
| Yes | 398 | 85% |
| Do you think that during your specialty training you have received sufficient formal training regarding surgical wound closure? | ||
| No | 197 | 42% |
| Yes | 274 | 58% |
| When you operate as head surgeon, who closes the surgical wound? | ||
| The nurse | 1 | 0.2% |
| You do | 267 | 57% |
| Another surgeon | 79 | 17% |
| A resident | 124 | 26% |
| How do you suture the skin in surgical wounds and with what [material]? | ||
| Staples | 424 | 90% |
| Continuous intradermal sutures | 23 | 5% |
| Discontinuous suture | 24 | 5% |
| Following surgery, do you supervise the surgical wound care or do you delegate this to nursing staff or to another colleague? | ||
| You do | 163 | 35% |
| Another medical professional | 44 | 9% |
| Nursing staff from outside your service (healthcare centre) | 22 | 5% |
| Nursing staff from the orthopaedic surgery service | 242 | 51% |
Results regarding dressing sealing according to the survey.
| Response | Total | % |
|---|---|---|
| When do you believe it is appropriate to perform the first surgical wound care? | ||
| At the slightest spotting, even if dressing is not saturated | 11 | 2% |
| Within the first 24h to rule out early wound complications | 61 | 13% |
| As late as possible within the recommendations for the dressing | 126 | 27% |
| After 48hours to avoid contaminating the wound | 273 | 58% |
| Do think that the choice of a dressing in particular affects the final outcome of the surgery (decrease in complications)? | ||
| No | 159 | 34% |
| Yes | 312 | 66% |
| What kind of dressing do you regard as most suitable in our setting (following surgery for fractures, arthroplasty, etc.)? | ||
| Conventional gauze dressings and compression dressing | 200 | 42% |
| Conventional hydrocolloid or hydrofiber dressings (the usual hydrocolloid dressings in in-patient wards) | 77 | 16% |
| Surgical hydrocolloid dressings | 155 | 33% |
| Hydrocolloid dressings only in high-risk patients (diabetics, obese) | 39 | 8% |
| In what cases do you use single-use incisional negative pressure therapy? | ||
| I don’t use it | 73 | 15% |
| Prophylaxis of surgical wound complications in high-risk patients | 93 | 20% |
| Prophylaxis of surgical wound complications in all patients | 3 | 1% |
| Treatment of surgical wound complications (seroma, prolonged drainage, dehiscence) | 302 | 64% |
| Does your service have modern dressings and negative pressure therapy? | ||
| No | 44 | 9% |
| Yes | 427 | 91% |
The importance of wound closure in any surgical procedure is beyond any shadow of a doubt. The quality of the wound closure will have a direct impact on the healing process of the surgical wound, as well as being the first barrier to possible external bacterial colonisation or drainage of fluid to the outside. Poor surgical closure will increase the risk of persistent surgical drainage, delayed healing, increased risk of superficial or deep infection, longer hospital stay, and even slower functional recovery.6 While it is true that all these factors are important in any surgery, they are particularly pertinent in the field of prosthetic surgery, in which there has been remarkable development of “enhanced recovery” programmes in recent years, and a great interest in lowering the infection rates associated with prosthetic implants, as demonstrated by the various local/state zero infection projects.7 Despite the evidence as to the importance of surgical wound closure, there is no information on how it should be performed, which hinders its assessment and potential improvement.6 Hence, as a common starting point for any improvement strategy, the current status of how surgical wound closure is performed in our setting must be ascertained.
On the whole, most respondents agree that surgical closure is important and that it influences the outcome of the procedure.8 Nonetheless, it is surprising that while recognising its relevance, almost half of the respondents do not perform surgical closure themselves (43%) or, even more noteworthy, 42% of them acknowledge that they did not receive adequate training in this regard during their residency period.
There is sufficient evidence that adequate haemostasis prior to initiating closure reduces the rate of surgical wound complications.9,10 Of all the tools available, the use of tranexamic acid, be it intravenously or locally administered, has amply established that it is effective in reducing postoperative bleeding, surgical drainage, and the need for post-operative transfusion. Its use does not cause any safety concerns in our setting, as demonstrated by the fact that 87% do not regard it as toxic for chondrocytes in hemiarthroplasty, given how extensively its distribution of use is, and that 56% of those surveyed believe that they can dispense with the use of drains when tranexamic acid is associated. Furthermore, 79% of the respondents feel that using it can decrease the risk of postoperative infection, because of the reduction in postoperative haematomas or prolonged drains.11–13 That said, despite the reported benefits of its use, two thirds of the respondents acknowledge that its indication, dosage, or route of administration are subject to the preferences of the anaesthetist present in the operating theatre.14,15
There is a broad consensus on the importance of deep plane closure (especially in the knee) as demonstrated by the importance given to deep closure by 96% of the respondents; 75% of them try to achieve as tight a closure as possible, and therefore, almost as many (72%) close this plane by the surgeon himself. However, 69% use loose polyglactin 910 stitches (Vicryl©, Ethicon, J&J, USA) as a technique to achieve this tight closure, although only just over half (58%) think that this is the ideal method for this purpose. There are 23% of respondents who consider the bearded continuous suture to be the ideal method, although only half (11%) use it for this closure. To check the integrity of capsular closure in knee arthroplasty, 78% of respondents perform a few flexion-extension movements before moving on to the next plane. Finally, only half of the respondents perform capsular repair after hip arthroplasty despite evidence of its influence in reducing the rate of dislocation.14,15
Historically, little importance has been attached to superficial closure in our speciality, despite the fact that 85% of respondents believe that proper closure of this plane can have a direct effect on the outcome of surgery. This is revealed by the fact that 81% use discontinuous sutures in a similar way to the deep plane closure, using the same suture material, despite them being different types of tissue; 67% of the respondents do not feel that the use of discontinuous sutures with multiple knots can influence the risk of superficial infection or even the risk of an accident (puncture).
Despite the controversy surrounding the use of staples or sutures for cutaneous closure, 90% of the surgeons interviewed admitted to using staples for closure. There are multiple studies that have demonstrated an increased risk of surgical wound complications when staples are used; however, the vast majority of these studies have not been conducted in the field of orthopaedic surgery. In a recent systematic review, Van de Kuit et al.16 observed an increased risk of cutaneous complications with the use of staples in elective hip and knee surgery. It is clear that further studies are still required that address the clinical and functional differences with the use of different closure methods.
There is abundant evidence against performing the first surgical wound dressing within the first 48h of wound evolution,6 unless there is an obvious complication, with 57% of the respondents reluctant to perform the first wound care before this time; 27% attempt to postpone this wound care as much as possible in accordance with the dressing manufacturer's recommendations. Although a smaller proportion of the surgeons surveyed regard dressing selection as important to the outcome of surgery (66%) than those considering closure (approximately 80% depending on the plane), it is interesting that nearly 91% of them have modern passive or active dressings available compared to 26% of those with bearded sutures for deep closure. These percentages are even more striking when up to 42% of the cases consider the classical dressing with compress or gauze to be the most appropriate for their wounds.
This study is not without its limitations. First of all, despite the large sample size of surgeons who responded to the survey (471 surgeons), this is still a small proportion of the orthopaedic surgeons in our country. Nevertheless, we believe that this sample suffices to obtain a representative picture of surgical wound closure practices. Second, all the surgeons questioned were members of SECOT and those who were not were excluded from the survey. However, there is no evidence that belonging to a scientific society can play a role in how wound closure is performed. Third, the position or type of centre can (and does) influence the type of closure used (for example, private hospitals, less use of staples for better cosmesis). Nevertheless, the aim of the present study is to understand the general practices of surgical wound closure in prosthetic surgery; therefore, these modifications depending on the type of centre do not affect the overall picture acquired.
There is consensus concerning the importance of proper wound closure in both TKA and THA; nonetheless, how wound closure is usually performed is not currently known. The results obtained from this study offer a compelling snapshot of our setting in this field. Closure is carried out by the surgeon themself in just over half of the cases (57%), using discontinuous sutures with polyglactin 910 (Vicryl©) for the deep plane (75%) and the superficial plane (89%), and staples for skin closure in 90% of the cases. Wounds are covered with modern dressings in 66% of the cases, albeit the dressing is applied within 48h in half of the cases (58%). Based on the snapshot shown and the fact that 42% of the respondents feel that they are not suitably trained in surgical wound closure, the authors recommend that the various scientific societies invest time and resources in improving training in this field, as well as adapting closure techniques to those regarded as the gold standard or that provide the best results, based on scientific evidence.
Level of evidenceLevel of evidence v.
FundingThe authors declare that there has been no source of funding to conduct this study.
Conflict of interestsP. Sanz Ruiz has participated as a consultant at Ethicon, DePuy Synthes, Link, Smith & Nephew, and Heraeus.
J.R. Caeiro Rey has participated as a consultant, clinical researcher, and/or speaker for the following companies: Amgen, Gebro, Gedeon-Richter, Grünenthal, Lilly, MSD, Synthes, Stryker, Theramex, UCB.
J.C. Martínez Pastor has participated as a consultant for Zimmer, Smith & Nephew, and Link. Consultancies requested for presentations, conferences for Johnson & Johnson MedTech.
J.L. Martín Alguacil Pastor has participated as a consultant at Ethicon, Mitek, Zimmer Biomet, DePuy Synthes, Smith & Nephew, and CONMED Linvatec.
A. Murcia Asensio Pastor has participated as a consultant, clinical researcher, and/or speaker for Johnson & Johnson MedTech.
J. Moreta Suárez Pastor has participated as a consultant for JRI Orthopaedics, MBA Surgical Empowerment, and Ethicon.