Hip resurfacing arthroplastys are a valid alternative for the treatment of degenerative hip disorders in young adults. Poor results and adverse soft tissue effects have been reported with high levels of chromium and cobalt, limiting its indications. Objective is to analyse clinical and functional survival results of the Durom system 10 years after its implementation in a public hospital. The hypothesis is that better results and survival are obtained in patients selected according to FDA criteria.
Material and methodsRetrospective cohort study of 83 patients, 91 hips in 76 men and 7 women operated between 2005 and 2013 with Durom-type prostheses. Demographic study, diagnosis, BMI, radiological study, serum chromium cobalt levels, functional assessment according to MPD and HSS, complications and survival at 10 years of follow-up. A cohort of active men under 65 years of age and heads over 48mm is selected.
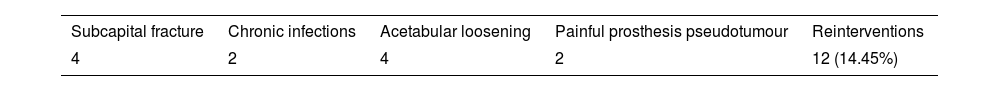
ResultsFollow-up time of 121 months with a range from 84 to 176 months. With a mean age of 52.78 years, with 4 deaths and loss of follow-up of 3 cases. There are 12 complications that require reoperation (14.45%) with 2 chronic infections, 4 femoral neck fractures, 4 acetabular loosening and 2 cases of pseudotumors. With an overall survival of 85.4% (71–91.9) and 87.85% (85.5–91.1) in the absence of infection. No statistical relationship between complications and neck narrowing and the angles of inclination of the components. In selected patients, 69 men and 73 hips, we obtained an overall survival of 91.82% and excluding infection of 93.18% at 10 years.
ConclusionsThe indication of the Durom system in the treatment of degenerative processes in selected active young patients presents better results and survival at 10 years, although somewhat lower than other highly indicated veneering models.
Las prótesis de recubrimiento son una alternativa válida para el tratamiento de los trastornos degenerativos de cadera del adulto joven, pero han sido reportados malos resultados y efectos adversos en partes blandas con niveles altos de cromo y cobalto, limitándose sus indicaciones. Nuestro objetivo es analizar resultados clínicos, funcionales y de supervivencia del modelo Durom a los 10años de su implantación en un hospital público. La hipótesis es que se obtienen mejores resultados y supervivencia en pacientes seleccionados según criterios de la FDA.
Material y métodosEstudio retrospectivo de cohortes con 83 pacientes —91 caderas en 76 hombres y 7 mujeres— operados entre 2005 y 2013 con prótesis tipo Durom. Estudio demográfico, diagnóstico, IMC, radiológico con posición de implantes, estrechamiento del cuello y tipo de unión ósea, niveles de cromo y cobalto en suero, valoración funcional según MPD y HSS, complicaciones y supervivencia a los 10años de seguimiento. Se selecciona una cohorte de varones activos menores de 65años y cabezas superiores a 48mm para la misma valoración.
ResultadosEl tiempo de seguimiento fue de 121meses, con un rango de 84 a 176meses. La edad media fue de 52,78años, con 4 defunciones y pérdida de seguimiento de 3 casos. Se producen 12 complicaciones que precisan reintervención (14,45%) con 2 infecciones crónicas, 4 fracturas del cuello femoral, 4 aflojamientos acetabulares y 2 casos de pseudotumores. La supervivencia global fue del 85,4% (71-91,9), y del 87,85% (85,5-91,1) en ausencia de infección a los 10años. No hubo relación estadística entre las complicaciones y el estrechamiento de cuello y los ángulos de inclinación de los componentes. En pacientes seleccionados —69 hombres y 73 caderas— obtenemos una supervivencia global del 91,82% y, excluyendo la infección, del 93,18% a los 10años.
ConclusionesLa indicación del sistema Durom en el tratamiento de procesos degenerativos de los pacientes jóvenes activos seleccionados presenta mejores resultados y supervivencia a los 10años, aunque algo inferior a otros modelos de recubrimiento muy indicados.
Metal-on-metal resurfacing prostheses have been a valid alternative for arthroplasty treatment of degenerative hip disease, especially in young active male patients.1 The wide range of motion, the absence of dislocations and their great tribological advantages have beenhighlighted.1 However, the health alert raised by functional adverse effects and soft tissue disturbances (pseudotumours) with high serum chromium and cobalt levels, with perivascular lymphocytic infiltrates in anatomopathological studies (ALVAL), especially in women,1 have limited the indication for this type of arthroplasty, making patient selection very important. Overall, the results reported in the literature depend on the model of resurfacing arthroplasty and the demographics of the population in which it is implanted, according to the 2016 Australian Registry.2 In 2005, the Durom-type resurfacing prosthesis and its MMC version (Zimmer-Biomet, Warsaw, IN, USA) were introduced in the orthopaedic surgery and traumatology department of the Parc de Salut Mar of the Autonomous University of Barcelona (Fig. 1). In 2016, the US Food and Drug Administration (FDA) set limited indications for resurfacing arthroplasty and selected only 2 approved models,3 Birmingham Hip Resurfacing by Smith & Nephew and Conserve Plus Micropore.
The aim of the present study is to analyse the results, complications and 10-year survival of this type of implant. Our hypothesis is that better results and survival are obtained in patients selected according to FDA criteria.
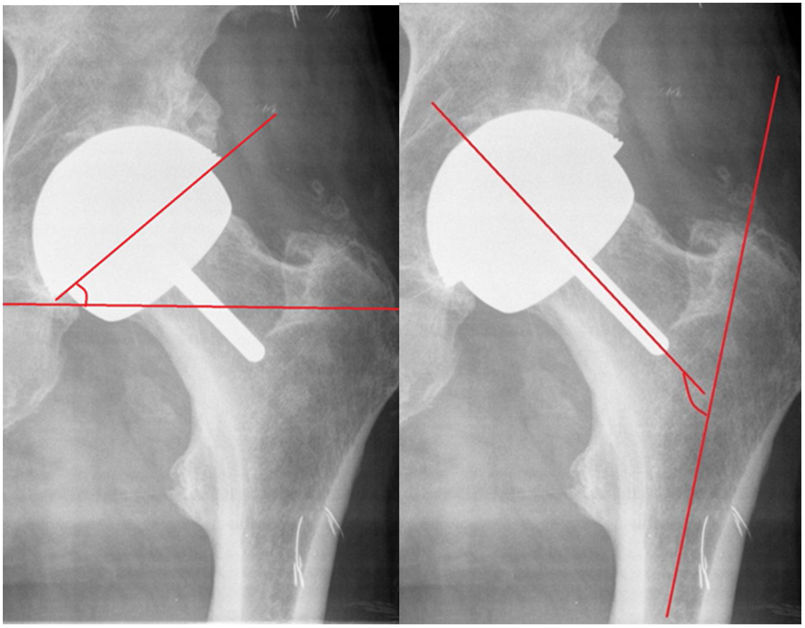
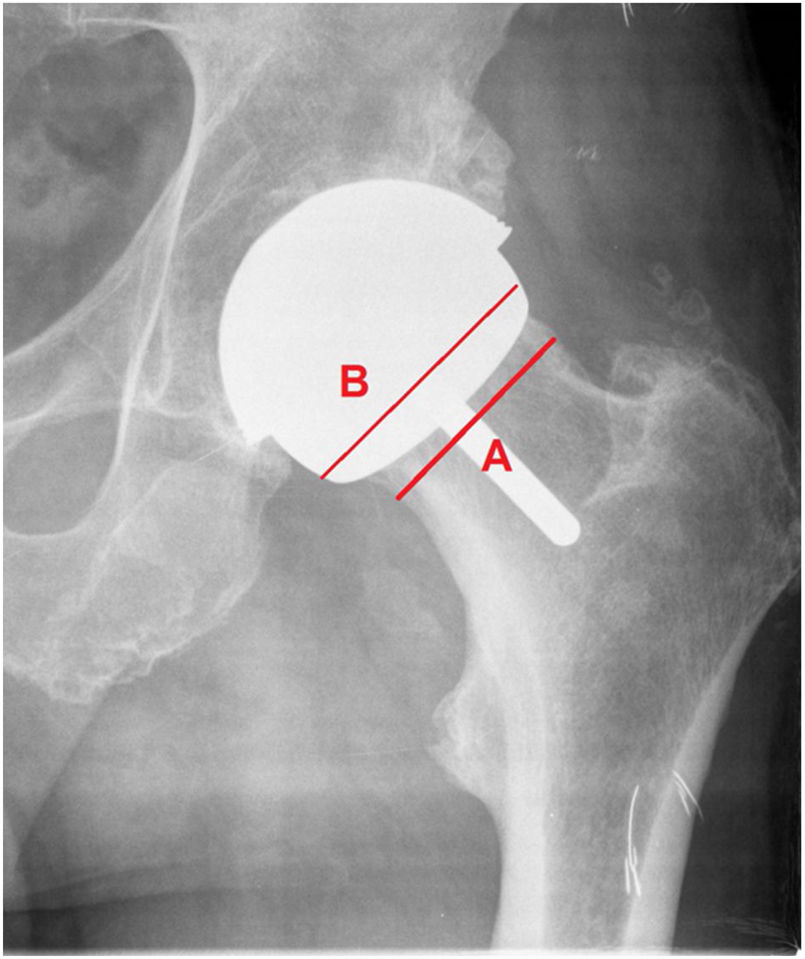
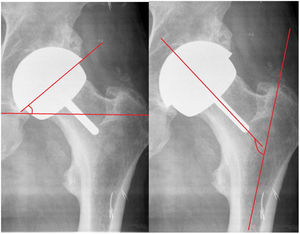
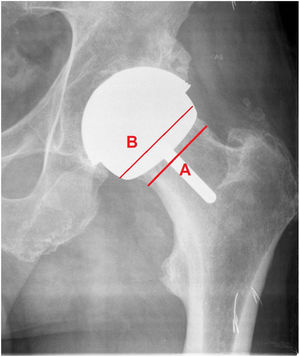
Material and methodsThis is a retrospective cohort study of patients who underwent surgery in our centre with a total resurfacing prosthesis using the Durom model and its MMC Cup version in the period from 2005 to 2013 with a follow-up of 84 to 176 months, and a mean of 121 months. We conducted a demographic study, including diagnosis, body mass index, complications, reinterventions, and implant survival. Functional assessment according to the Merle Postel D’Aubigné and Harris Hip Score scale, radiological assessment with PACS, evaluating: acetabular and femoral component position in frontal and axial projections (Fig. 2), radiolucencies in the Lee and Charnley areas of the cup; radiolucencies in the stem area according to the method of Pollard et al.,4 neck narrowing according to the scale of Spencer et al.5 at 3 months (Fig. 3), and horizontal offset variation. Engh's score was used for cup osseointegration (union, stable fibrous union, non-union) and Brooker's score for periarticular calcifications. Blood chromium and cobalt levels were measured annually in a laboratory validated for the general population. We also studied survival and complications in the cohort of patients to which the FDA criteria for the indication of this type of implant were applied: active males aged less than 60 years and femoral heads greater than 48mm.6–8
Durom and MMC cupHemispherical titanium vanadium vacuum and plasma sprayed hemispherical press-fit cup with an angle of 165° (less than a 1.5mm hemisphere), flattened at the pole with a Metasul interior with equatorial grooves to increase the primary press-fit, and whose MMC version adds 3 longitudinal grooves removing the equatorial groove.
The femoral component was designed to be cemented with an alignment stem with recesses for cement extrusion to achieve a layer of 3mm to 4mm, is sized in 2mm increments, and is 6mm less than the acetabular component.
This implant was no longer marketed in 2013, and therefore no longer implanted in our department, and the indication for resurfacing prosthesis was discontinued, but clinical controls continue to date.
A modified lateral approach of Hardinge was used in all cases and antibiotic prophylaxis with cefazolin was used, or vancomycin in allergic patients. The indications for the specific technique previously used in cadavers were followed and a visit was made to a surgeon who was an expert in this technique and implanted using the same approach.
Antithrombotic prophylaxis was administered with enoxaparin during the first postoperative month, and no prophylaxis with indomethacin for periarticular calcifications was administered. The patient was allowed to sit at 24h and underwent gait re-education partially weight-bearing with 2 crutches, with outpatient controls at one month, 3 and 6 months, one year and, thereafter, every two years. In cases of loss to follow-up, the shared clinical history of Catalonia was used, with access to clinical data and complementary examinations. All patients underwent serum analysis to determine chromium and cobalt levels, renal function, and CRP annually. Ultrasound and magnetic resonance imaging (MRI) with metal artefact attenuation software were performed in cases of unexplained pain and suspected pseudotumour.
Survival was calculated according to the Kaplan–Meier method, with revision pending or revision performed for any reason at the end of follow-up.
SPSS (version 14, SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Differences between pre- and postoperative data for functional scales and radiographic parameters were analysed with the Student's t-test for normal distribution, and the data based on means and SD.
ResultsWe obtained a cohort of 83 patients, 91 hips in 76 men and 7 women, 43 right, 40 left and 8 bilateral, with a mean age of 52.78±8 years, and a body mass index of 28.42. The surgery was performed by 3 surgeons with expertise in hip surgery.
Indications: 69 hips for osteoarthritis, 21 for sequelae of AVN, and one case for proximal femoral deformity, not indicated in sequelae of dysplasia.
At the end of follow-up there had been 4 deaths (one due to AMI and 3 due to neoplasia) and 3 patients were lost to follow-up, resulting in a final cohort of 76 patients with 82 operated hips in 69 men and 7 women, with a mean follow-up of 121 months.
The mean functional assessment (Merle Postel D’Aubigné) preoperatively was 13.56, and 17.5 and 17.44 at 5 and 10 years, respectively, with statistically significant differences. The mean preoperative Harris Hip Score was 57.9±12 and the postoperative HHS at the end of follow-up was 96.3±5.9, equally significant, which was maintained at the end of follow-up.
The mean acetabular diameter was 56±3mm (65–52) and head diameter was 50±3mm (56–42).
The mean acetabular angle obtained was 38.42±8.05 and femoral angle was 143.54±8.2, pre- and postoperative offset ratio of .94. Neck narrowing was observed in 7 cases (8.53%) in the first 3 months, remaining stable over time, and type II calcifications in 3 cases (3.65%).
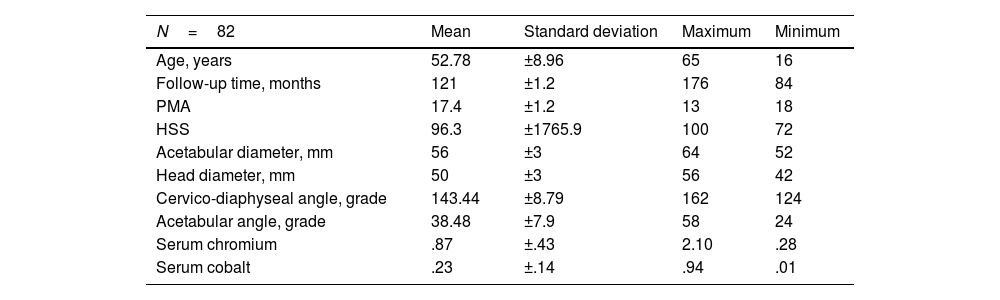
Radiolucencies were observed in Lee and Charnley zone i in 2 cases, in zone II in 3 cases, and in both zones in 2 cases. A sclerotic line was detected at the tip of the femoral stem (type I pedestal sign) in 8 patients, with no radiolucency observed in the entire periphery of the stem (type III). Following Engh's score, 78 integrated cotyles, no stable fibrous union and 4 cases of loosening were obtained. Mean serum chromium and cobalt levels were .87μg/l (.55–1.1) and .23μg/l (.15–.29), respectively (Table 1), the normal reference in our laboratory (Catalonia reference) being lower than 2 for cobalt and lower than 4.6 for chromium.
Series.
| N=82 | Mean | Standard deviation | Maximum | Minimum |
|---|---|---|---|---|
| Age, years | 52.78 | ±8.96 | 65 | 16 |
| Follow-up time, months | 121 | ±1.2 | 176 | 84 |
| PMA | 17.4 | ±1.2 | 13 | 18 |
| HSS | 96.3 | ±1765.9 | 100 | 72 |
| Acetabular diameter, mm | 56 | ±3 | 64 | 52 |
| Head diameter, mm | 50 | ±3 | 56 | 42 |
| Cervico-diaphyseal angle, grade | 143.44 | ±8.79 | 162 | 124 |
| Acetabular angle, grade | 38.48 | ±7.9 | 58 | 24 |
| Serum chromium | .87 | ±.43 | 2.10 | .28 |
| Serum cobalt | .23 | ±.14 | .94 | .01 |
After 10 years we have 76 patients and 82 hips with 12 complications (14.45%) and reinterventions, with 2 chronic infections, 4 femoral neck fractures, 4 aseptic acetabular loosening, and 2 cases of painful prosthesis and pseudotumour with normal chromium and cobalt levels: 1.1/.13 and .5/.17, respectively (Table 2). Overall survival was 85.54% (95% CI 71.1–91.9) and 87.85% (95% CI 85.5–91.1) in the absence of infection. Minor complications not requiring intervention included one case of trochanteric pain, one case of neurapraxia of the external popliteal sciatic nerve, which resolved spontaneously, and one case of persistent Trendelenburg gait.
It is important to note that of the 4 subcapital fractures, 2 occurred in women aged 65 and 53 years, respectively, with heads of 52mm and 44mm, in the first and second month after implantation. Of the 4 cases of acetabular loosening, one occurred in a 55-year-old male at 3 months after implantation, and of the other 2, one case was noteworthy in a 60-year-old female at 9 weeks.
Statistical analysis showed no relationship between complications and neck narrowing and angles of inclination of the prosthetic components.
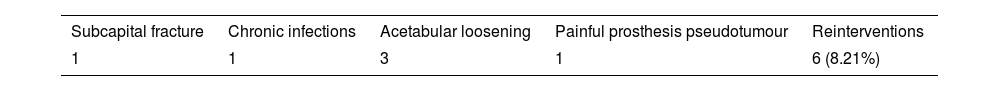
After applying the FDA criteria (active males under 60 years of age with heads greater than 48mm), we obtained a cohort of 73 hips in 69 men. Six complications requiring rescue were obtained: one infection, one fracture, one pseudotumour, and three cases of acetabular loosening (one of them already referred to above, at 3 months), and we obtained an overall survival rate of 91.82% and a survival rate excluding infection of 93.18% at 10 years (Table 3).
DiscussionThe poor results obtained in young patients when conventional hip prostheses with metal-to-metal friction torque and non-crosslinked-polyethylene were indicated were the reason for the resurgence of resurfacing prostheses.9 These prostheses had tribological advantages, with the use of the metal-to-metal friction torque, with better bone preservation and good functional outcomes, and in meeting patient expectations.9–11
Resurfacing prostheses are technically demanding, with a recognised learning curve, and require correct patient selection and preoperative planning.10
In some published series the current failure rate is much higher than expected. The figures are worrying, therefore, in national registries of major arthroplasties.2,3,7
The most frequent complications described are fixation failure of the acetabular component, subcapital fracture and abnormal reactions to high serum chromium and cobalt levels that cause an ALVAL-type tissue response and pseudotumours.2,12,13
In 2010, the Spanish Agency of Medicines and Medical Devices and other international agencies issued a health alert regarding the use of the ASR model (DePuy Johnson & Johnson, Warsaw, In, USA), due to the high rate of mechanical failure and elevated levels of serum chromium and cobalt metal ions with toxic implications, and warned of the high number of wear particles in periarticular tissues. The Australian Registry2 reported a 10-year revision rate of 7% with the use of this type of implant, a rate that is considered unacceptable.
The Durom resurfacing prosthesis was designed by Grigoris et al.14 in 2000 and brought to the Spanish market in 2001, and was modified and replaced by the MMC model in 2009, both of which were withdrawn from the market in 2013.
There are few studies on the implantation of resurfacing prostheses using a modified lateral approach of Hardinge as indicated by Delgado en 2009,15 and the only reference using the Durom model and this approach is by Gravius et al.,16 with good functional results without Trendelenburg gait and with good survival, although with a short follow-up.
Neck narrowing occurred in 7 cases (8.53%) in our series, low compared to other series reporting up to 25%.5 No statistically significant association with mechanical complications was found, consistent with other studies.5,9 This phenomenon has not been explained, possibly related to biomechanical changes or circulation disorders, as they are more frequently described after posterior approaches,17,18 which would explain the low frequency with our lateral approach.
In our series we reported a 5-year mechanical failure rate of the Durom cup of 3.3%, with a survival of 96.7% in the absence of infection and at 10 years of 87.85%, which contrasts with the 2010 results of Long et al.19 of 11% failure, and of Migaud et al.20 in 2012 of 6%, compared with Vendittoli et al.21 with 0% in 2007, and Grigoris et al.14 with .05% in 2006. Data from the Australian Registry report that the Durom model has a cumulative revision rate at 5 years of 6.7%,22 with poor outcomes.
On analysis of mechanical complications at 10 years, we observe 4 subcapital fractures in 3 women and 1 man, 2 of which occurred within the first 3 months, at the ages of 56 and 63 years; we also observed 4 acetabular loosenings in 3 men and 1 woman, and 2 of these occurred within the first 3 months of implantation, at the ages of 56 and 60 years. These data indicate, on the one hand, poor patient selection (women over 55 years of age), and on the other, a learning curve for the procedure, as indicated by many studies using the same implant.16,21,23 Regarding the remaining complications that required intervention, we had 2 chronic infections that required replacement in 2 stages and that were finally cured according to the standards for prosthetic hip infection in our department for patients in that age range.
Two cases of pseudotumour and painful prosthesis (2.4%) were detected at 6 and 9 years, respectively, by ultrasound and MRI with metal artefact attenuation. No significantly high chromium and cobalt levels were detected in these two cases. They were replaced with conventional hip prostheses with a polyethylene ceramic torque, with good results. Our incidence of pseudotumours is lower compared to the 3.3% for large cysts and 8.3% for small cysts described by Robinson et al.24 and the reported incidence of 16.5 and 10.6% for cysts larger than 1cm. This could be because we only performed ultrasound and MRI in cases of suspicion due to pain and other symptoms (limitation of the study).
In a previous study by the same group (Cuenca et al.25), a relationship was found between chromium levels and the greater angle of position in the frontal plane of the femoral component with functional results, with significant differences being observed with angles greater than 143°.
The overall survival of our series of 85.54% at 10 years is lower than expected when compared to conventional primary arthroplasty series, which exceed 93% in most studies.6,7,26,27
In 2014 and 2017, the National Institute for Health and Care Excellence recommended the use of resurfacing prostheses to treat osteoarthritis of the hip if a revision rate of less than 5% was achieved at 10 years with the prosthetic models reported, advising their indication in young males. The FDA8 accepted only 2 prosthetic models, the Birmingham Hip Resurfacing (Smith & Nephew) being the most widely used in the American market in active male patients under 60 years of age with femoral heads over 48mm.
Once our cohort of patients was selected according to these criteria, we obtained an overall all-cause survival of 91.82% and 93.18% if infection was ruled out, below expectations, with a good functional outcome according to the scales used (Merle Postel D’Aubigné and Harris Hip Score), with chromium and cobalt levels not significantly above the reference values, which contrasts with other studies with worse survival rates, such as that of Naal et al.,28 at 88.2% with the same implant, and Seppanen et al.,29 with a survival rate of 72%. The most frequent complication is mechanical loosening of the acetabular component, as emphasised by Long et al.19
If we compare survival in patients selected according to the same criteria, but using the Birmingham hip resurfacing implant, we obtain better survival rates, such as that shown by Ford et al.,3 of 98.2% at 10 years, and that of Van der Straeten,30 of 95% at 10 years and 90% at 22 years, excluding arthroplasties with the ASR and CORMET devices.
In the same work by Van der Straten,30 survival in men is 99% at 10 years and 92.5% at 21 years, whereas in women it is 90% and 81.3%, respectively.
The limitations of the study include its retrospective nature, the inclusion of all cases (learning curve) with some early complications that would be avoidable with greater experience in implantation, and the performance of MRI and ultrasound scans only in suspected cases of pseudotumour or local soft tissue complication due to symptoms, and not being able to rule out detection of these abnormal reactions in asymptomatic patients.
In conclusion, we believe that the use of the Durom/MMC resurfacing system for the treatment of degenerative processes in selected patients (active men under 60 years of age), and once the learning curve has been completed, shows better results, with good survival. However, results are inferior to those of other resurfacing models on the market, and this highlights the problems of acetabular fixation.
Level of evidenceLevel of evidence iv.
Conflict of interestsThe authors have no conflict of interests to declare.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.