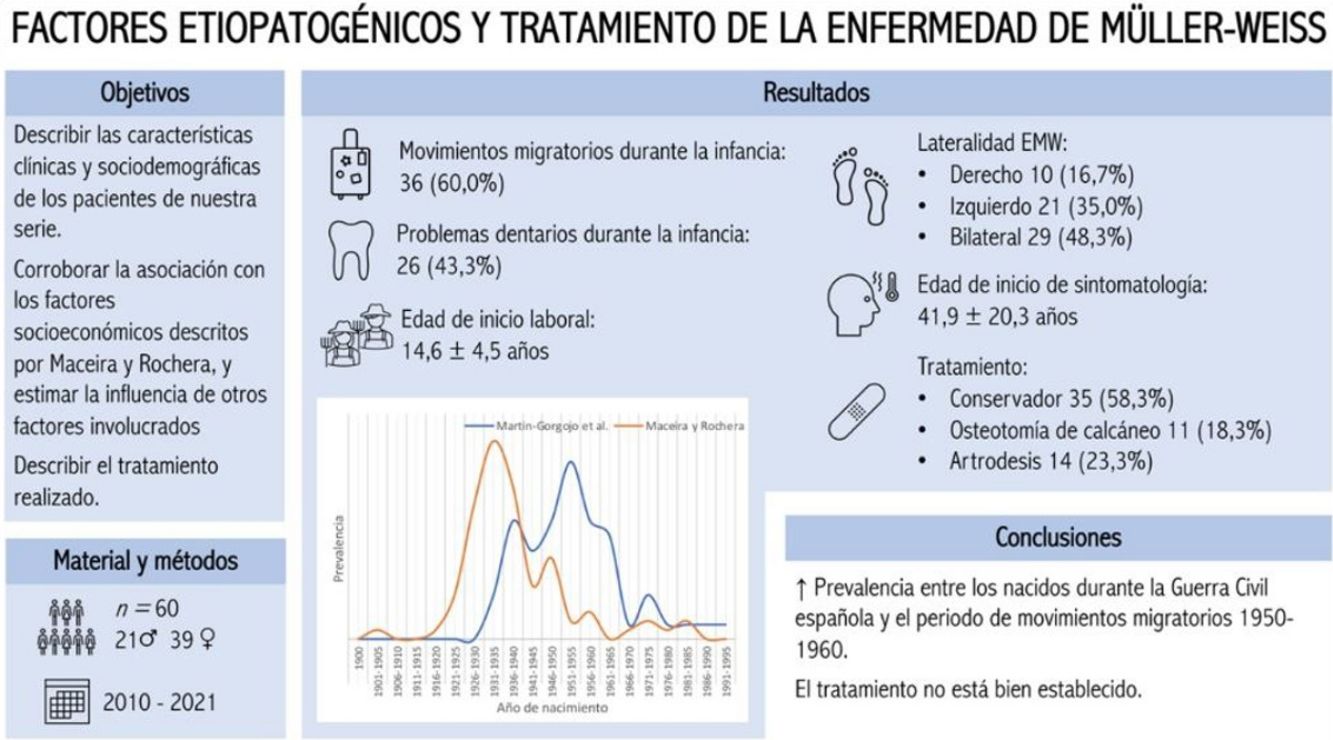
Müller-Weiss disease (MWD) is a rare anomaly of the tarsal scaphoid. Maceira and Rochera proposed the most commonly accepted etiopathogenic theory, in which dysplastic, mechanical, and socioeconomic environmental factors would be involved. The aim is to describe the clinical and sociodemographic characteristics of patients with MWD in our setting, corroborate their association with the socioeconomic factors previously described, estimate the influence of other factors involved in the development of MWD, and describe the treatment carried out.
Materials and methodsRetrospective study of 60 patients diagnosed with MWD in 2 tertiary hospitals of Valencia (Spain) between 2010 and 2021.
ResultsSixty patients were included, 21 (35.0%) men and 39 (65.0%) women. In 29 (47.5%) cases, the disease was bilateral. The mean age of onset of symptomatology was 41.9±20.3 years. During childhood, 36 (60.0%) patients suffered migratory movements, and 26 (43.3%) had dental problems. The mean age of onset was 14.6±4.5 years. Thirty-five (58.3%) cases were treated orthopedically versus 25 (41.7%) treated surgically, 11 (18.3%) by calcaneal osteotomy, and 14 (23.3%) with arthrodesis.
ConclusionsAs in the series of Maceira and Rochera, we found a higher prevalence of MWD among those born around the Spanish Civil War and the period of massive migratory movements that occurred in the fifth decade of the 20th century. Treatment is still not well established.
La enfermedad de Müller-Weiss (EMW) es una anomalía poco frecuente del escafoides tarsiano. Maceira y Rochera propusieron la teoría etiopatogénica más comúnmente aceptada, en la que estarían implicados factores displásicos, mecánicos y ambientales socioeconómicos. Se pretende describir las características clínicas y sociodemográficas de los pacientes de nuestro entorno con EMW, corroborar su asociación con los factores socioeconómicos descritos previamente, estimar la influencia de otros factores descritos en el desarrollo de la EMW, así como describir el tratamiento realizado.
Materiales y métodosEstudio retrospectivo de 60 pacientes diagnosticados de EMW en 2 hospitales terciarios de Valencia (España) entre los años 2010 y 2021.
ResultadosSe incluyeron 60 pacientes, 21 (35,0%) hombres y 39 (65,0%) mujeres. En 29 (47,5%) casos la afectación fue bilateral. La media de edad de inicio de la sintomatología fue de 41,9±20,3 años. Durante la infancia, 36 (60,0%) pacientes sufrieron movimientos migratorios, y 26 (43,3%) problemas dentarios. La edad media de inicio laboral fue de 14,6±4,5 años. Se trataron de forma ortopédica 35 (58,3%) casos frente a 25 (41,7%) tratados quirúrgicamente, 11 (18,3%) mediante osteotomía de calcáneo y 14 (23,3%) con artrodesis.
ConclusionesAl igual que en la serie de Maceira y Rochera, encontramos una mayor prevalencia de EMW entre los nacidos alrededor de la Guerra Civil española y el periodo de movimientos migratorios masivos acontecidos en la quinta década del siglo xx. El tratamiento sigue sin estar bien establecido.
Müller-Weiss disease (MWD) was described for the first time in 1927 by the German surgeon Walther Müller1 and the Austrian radiologist Konrad Weiss.2 Both of them observed an anomaly in the tarsal scaphoid, which had a condensed, compressed or fragmented appearance. Nevertheless, this condition was actually first described by Schmidt in 1925.1
The aetiology and pathogenesis of this disease gave rise to controversy throughout the twentieth century. In 2004, Maceira and Rochera,3 after analysing 101 patients with MWD, proposed that it consists of dysplasia in tarsal scaphoid development due to a delay in its ossification. They also considered that unequal compression forces on the scaphoid had to be present, centred on the lateral part of the same, to cause the typical deformity. It would therefore be associated with an almost constant varus rear foot. They also suggest that there is a link between the appearance of MWD and certain socioeconomic environmental factors, wars or mass migrations which may cause nutritional stress with repercussions on the overall growth of an individual, or the isolated growth of the tarsal scaphoid. However, Doyle et al.4 could not confirm this association in their series of 12 patients.
Although MWD usually commences in childhood, it does not usually have any clinical manifestations until the fourth or fifth decade of life.5 It appears more often in women, and it has a tendency to be bilateral.6 The patients with this condition have insidious chronic pain with mechanical characteristics in the dorsomedial region of the mid to rear foot that is sometime associated with swelling.7 When untreated it gives rise to the form of a flat food with rear foot varus (which is also known as “paradoxical flat foot”) that evolves into different degrees of arthrosis in the periscaphoid joints.3
Although MWD is considered to be a rare disease, its actual incidence is unknown.7 This may be because it is often asymptomatic or because it is diagnosed in advanced radiological studies, when astragalus-scaphoid arthrosis has already become established.
There is currently no agreement on the therapeutic management of this disease.5 Treatment is usually conservative at first, based on the modification of everyday activities, the use of orthopaedic insoles or external orthoses, and analgesic-anti-inflammatory drugs. Surgical treatment is reserved for when orthopaedic treatment has failed, and the options used the most often are foot arthrodesis at different levels or corrective osteotomy of rear foot varus. Some authors prefer to use calcaneal osteotomy as the first choice for surgery in the treatment of MWD, regardless of its radiographic stage.5,8 Nevertheless, there is no clear algorithm for treatment, so that each case has to be evaluated on an individual basis.7
To the best of our knowledge, this is the first study in our country since the one by Maceira and Rochera in 2004, and it is one of the few studies published at an international level with the aim of investigating the aetiopathological factors associated with MWD.
ObjectivesGeneral/main objectiveTo describe the incidence of MWD and the socioeconomic factors which give rise to its appearance, in the Orthopaedic Surgery and Traumatology Departments of the Hospital Clínico Universitario and the Hospital Universitario y Politécnico La Fe, Valencia.
Specific objectives- -
To describe the clinical and sociodemographic characteristics of patients with MWD.
- -
To confirm the association between MWD and the socioeconomic factors described by Maceira and Rochera.3 Another aim is to estimate the influence of other factors which have been said to affect the development of MWD.5
- -
To describe the treatment received by each patient.
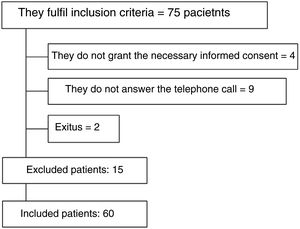
An observational retrospective study was undertaken that included all of the patients diagnosed in the outpatient surgeries of Orthopaedic Surgery and Traumatology and treated for MWD from 2010 to 2021 in 2 tertiary hospitals of the City of Valencia: Hospital Clínico Universitario and Hospital Politécnico La Fe. All of the patients who did not give their consent to take part in the study were excluded, as were those who died during the follow-up.
Patient data were collected on the following study variables: age, sex, place of birth, migratory movements during their childhood and adolescence, the age at which they started work and if they had worked in jobs with high functional demands, as well as if they had suffered dental problems during childhood (as an expression of nutritional or ossification disorders). Other clinical variables were also recorded, including age at the onset of symptoms, age at the time they first consulted, the presence of rear foot varus found in the physical examination, or, if this were not shown, by measuring the angle talus-calcaneus (Kite) angle in the dorsoplantar X-ray image under load, the presence of index minus, laterality, MWD staging according to Maceira's classification (1, minimum changes; 2, horizontalization of the astralagus; 3, fatigue fracture; 4, gradual approximation of the astralagus and the wedge bones, and equinization of the heel; 5, complete extrusion of the scaphoid, forming an astragalus-wedge bone joint),3,9 as well as the treatment applied (orthopaedic or surgical, and the surgical technique used).
A descriptive analysis of the results was carried out using version 25 of the IBM® SPSS® statistical calculation programme. The data corresponding to quantitative variables is expressed as an average±standard deviation, and qualitative variables are expressed as absolute numbers and percentages, except those which are expressly shown as otherwise. Likewise, the Microsoft® Excel computer programme was used to draw up a double curve graph which shows the prevalence of MWD according to the year of birth of the patients in our series and the series of Maceira and Rochera.3
The Clinical Research Ethics Committee of our hospital (INCLIVA) approved this study. All of the patients included gave their verbal informed consent to participate in it.
ResultsInitially 75 patients fulfilled the inclusion criteria. 15 of these patients were then excluded (Fig. 1), so that our series included a total of 60 patients. Of the total number of patients included in our study, 21 (35.0%) were from the Hospital Clínico Universitario and 39 (65.0%) were from the Hospital Politécnico La Fe. 21 (35.0%) patients were men and 39 (65.0%) were women.
The median year of birth of the patients included in the study was 1952 [1932–1993], and their average age at the moment data were gathered was 68.3±13.3 years. Fig. 2 shows a double curve, comparing the prevalence of MWD according to the year of birth of the patients in our series with prevalence in the 2004 series of Maceira and Rochera3 [1900–1990].
Year of birth of the patients in our series, compared with the 2004 series of Maceira and Rochera [1900–1990]. Adapted and reproduced with the permission of Maceira and Rochera.3
With respect to the place of birth, Table 1 shows the province and autonomous community (or country, in the case of births outside Spain) where the patients in our series were born. Fig. 3 shows these results more graphically, over a political map of the Spanish provinces.
Place of birth.
| Total, n (%) | |
|---|---|
| Spain | |
| Andalusia | 12 (20.0) |
| Cordoba | 1 (1.7) |
| Granada | 1 (1.7) |
| Huelva | 1 (1.7) |
| Jaen | 4 (6.7) |
| Malaga | 2 (3.3) |
| Seville | 3 (5.0) |
| Aragón | 1 (1.7) |
| Teruel | 1 (1.7) |
| Castile-La Mancha | 6 (10.0) |
| Albacete | 1 (1.7) |
| Ciudad Real | 1 (1.7) |
| Cuenca | 4 (6.7) |
| Comunidad Valenciana | 28 (46.7) |
| Alicante | 1 (1.7) |
| Castellon | 2 (3.4) |
| Valencia | 25 (41.7) |
| Extremadura | 2 (3.3) |
| Badajoz | 2 (3.3) |
| Murcia | 2 (3.3) |
| Melilla | 2 (3.3) |
| Other countries | |
| Africa | 4 (6.7) |
| Algeria | 1 (1.7) |
| Equatorial Guinea | 1 (1.7) |
| Morocco | 1 (1.7) |
| Nigeria | 1 (1.7) |
| Europe | 2 (3.3) |
| Germany | 1 (1.7) |
| France | 1 (1.7) |
| South America | 1 (1.7) |
| Bolivia | 1 (1.7) |
Table 2 shows data corresponding to the personal histories of the patients in the study, including information on migratory movements during infancy, dental problems during the said period, the age at which they started work and an estimation of the patients who had worked in jobs with a high level of functional demand (generally heavy work in the countryside or as assistants in high intensity jobs that were unsuitable for their age). Additionally, although intense sports training from an early age was not formally recorded, we believe that we should mention that the only patient under 30 years of age in our series had been a federated football player from his childhood.
Data on the childhood of the patients.
| Total | |
|---|---|
| Migratory movements during childhood, n (%) | 36 (60.0) |
| Dental problems during childhood, n (%) | 26 (43.3) |
| Age at starting work (years), average±SD | 14.6±4.5 |
| Estimation of patients who performed highly functionally demanding work at early ages, n (%) | 21 (35.0) |
Table 3 shows the foot anatomy data of the patients in the series, as well as the laterality of MWD, its stage and the treatment used.
Data on the foot anatomy of the patients, laterality and stage of MWD, as well as the treatment applied.
| Total, n (%) | |
|---|---|
| Rear foot varus | 58 (96.7) |
| Index minus | 40 (66.7) |
| Laterality | |
| Right | 10 (16.7) |
| Left | 21 (35.0) |
| Bilateral | 29 (48.3) |
| MWD stage | |
| 1 | 2 (3.3) |
| 2 | 10 (16.7) |
| 3 | 16 (26.7) |
| 4 | 15 (25.0) |
| 5 | 17 (28.3) |
| Treatment | |
| Conservative | 35 (58.3) |
| Calcaneal osteotomy | 11 (18.3) |
| Arthrodesis | 14 (23.3) |
Table 4 shows the type of surgical technique used (calcaneal osteotomy vs. arthrodesis) depending on the MWD stage. The calcaneal osteotomy used in our hospitals consisted of a Dwyer-type external wedge with a lateral translation, or an inverted Koutsogiannis. If arthrodesis was used, the techniques used were astralagus-scaphoid arthrodesis and, in cases of very severe arthrosis which involved the scaphoid-wedge joint, astralagus-scaphoid-wedge arthrodesis. The selection of one surgical technique or another varied depending on the preferences of each surgeon, and there was no single protocol at the time this study was performed. However, we have observed a recent change in the treatment tendency in our hospitals, which has evolved from arthrodesis in the older cases to increased indication for calcaneal osteotomy, regardless of whether changes caused by arthrosis are present or not.
Type of surgical treatment received according to MWD stage.
| MWD stage | ||||||
|---|---|---|---|---|---|---|
| Total | 1 | 2 | 3 | 4 | 5 | |
| Calcaneal osteotomy, n (%) | 11 (44.0) | 0 (0.0) | 4 (36.4) | 1 (9.1) | 3 (27.3) | 3 (27.3) |
| Arthrodesis, n (%) | 14 (56.0) | 1 (7.1) | 0 (0.0) | 4 (28.6) | 5 (35.7) | 4 (28.6) |
| Total, n (%) | 25 (100.0) | 1 (4.0) | 4 (16.0) | 5 (20.0) | 8 (32.0) | 7 (28.0) |
The average age at which symptoms commenced was 41.9±20.3 years, while the first visit shown in computerized clinical histories was at an average age of 59.6±13.2 years.
DiscussionThe series shown is the second in terms of the number of patients it includes, after the series in the study by Maceira and Rochera,3 who analyzed a total of 101 patients with an average age at diagnosis of 47.6 years, which is slightly younger than in our sample. This may be due to the fact that we record patient age at the time of the first visit shown in their computerized clinical histories, as these patients will often have been seen by other specialists before visiting the outpatient services of the Foot and Ankle Surgery Unit. It should also be pointed out that our series only adds a few years to the one described by Maceira and Rochera,3 which included data from patients who had been born from 1900 to 1990, as opposed to the data from our patients, who were born from 1932 to 1993.
There was a predominance of women in our study, and this coincides with the findings of other studies.3,4 Furthermore, although the bilateral presentation rate was close to 50%, which is higher than the rate described by other authors,8,10 it is in line with the figure given by Monteagudo and Maceira.5 These authors stated that the majority of the patients in different studies had bilateral involvement.
Although MWD was first described in 1927,1,2 it was not until 2004 that Maceira and Rochera3 published the aetiopathogenic theory that is now the most widely accepted. They proposed that delay in the ossification of the scaphoids and abnormal distribution of loads in the foot are of key importance for the development of MWD. The delay in ossification may occur after general or localized alterations in development. Nutritional deficits stand out among the general causes. They may be due to a range of extrinsic causes, such as belonging to a low socioeconomic class, poverty or war. They may also be caused by intrinsic causes, such as endocrine pathologies or metabolic diseases and syndromes causing poor absorption. Thus, in their series Maceira and Rochera3 describe two peaks in incidence: one among individuals born at the end of the 1920s, with a maximum in 1932, just before the Spanish Civil War began (1936–1939). The other lesser peak occurred just before the mass migratory movements which emerged in our countries in the 1950s, from rural regions into Madrid, Barcelona and the coastal provinces.
When our series is analyzed in comparison with the one by Maceira and Rochera,3 it can be seen that in ours, the peaks of disease prevalence occur 10 years later. Although there is no simple explanation for this phenomenon, it seems reasonable to assume that we probably found no peak before the Spanish Civil War because our study occurred at a later date when many of the potential patients would have died. The majority of patients do in fact largely coincide with the second peak described as being due to mass migrations. The gap in time between their data gathering for their study and our later work may be why we observed a larger number of patients who were born after the Spanish Civil War, who in the earlier series would still not have developed the clinically observable disease. When the place of birth of our patients was analyzed, although almost half of them were born in the Comunidad Valenciana, 60.0% of them stated that they had had to move locality or province when they were young, which supports the environmental theory of these authors. Maceira and Rochera3 also found Harris lines and dental enamel hypoplasia in several of the patients in their series, as a result of these periods of “nutritional stress”. Almost half of our patients also had dental problems during childhood.
As well as the delay in the ossification of the tarsal scaphoids in the development of MWD, Maceira and Rochera3 also believe that an abnormal distribution of forces plays a fundamental role by increasing the loads on the lateral portion of the navicular bone. The predisposing conditions for this include primary subtalar varus or a shortened first metatarsus. The data in our study are in agreement with this theory: practically all of the patients had clinical rear foot varus and in more than half of the cases, a minus index. Our study also found an early average age for starting work, in jobs that were often highly demanding in functional terms, which would add to the loads on the feet during growth. Playing high intensity sports at an early age has also been associated with increased loads and the development of MWD,5,11 as is the case with the patient under 30 years old in our study, who was a federated football player from a very young age.
The most suitable treatment for this condition has yet to be determined, and this is also the case for the technique to be used if the decision to apply surgical treatment is taken. The majority of the patients in our series were treated conservatively, and our subjective opinion based on the remarks of the patients is that the clinical results of this were satisfactory. Treatment is usually conservative at first, and it consists of the administration of NSAIDS, modifying any sports activity, weight loss and the use of supporting insoles7 with lateral wedges in the heel to reduce rear foot varus, as well as good support for the medial arch to prevent the tarsal scaphoids from sinking.5 However, there is no clear evidence for the efficacy of this treatment or how long it should last until improvement is obtained.
If conservative treatment fails, surgical treatment is usually indicated based on the symptoms and functional limitation of patients rather than the radiological stage of the disease, given that the latter does not normally correlate with the severity of the symptoms.5,7,12 Surgical treatment aims to provide symptomatic relief and, as far as is possible, to recover the medial plantar arch. The main therapeutic options include astragalus-scaphoid or astragalus-scaphoid-wedge bone arthrodesis and calcaneal osteotomy.7
At first in our hospitals, we only tended to perform calcaneal osteotomy with lateral translation and an externally based wedge (which combine the inverse Koutsogiannis effect and the Dwyer effect) when joint degeneration was not very marked, reserving arthrodesis for more severe cases. As other authors have reported,7,8,13 the results of calcaneal osteotomy have been satisfactory, as it transfers compression forces from the damaged areas of cartilage at the level of the lateral face of the scaphoids to healthy areas of cartilage in the more medial slope of the scaphoids.5 Some authors now use osteotomy as the procedure of choice regardless of the radiographic stage or degeneration of the different periscaphoid joints.5,8,13 In the same way, when we reviewed our series we found a change of tendency in our indication, passing from arthrodesis in the oldest cases to the use of calcaneal osteotomy in patients operated more recently, without taking changes caused by arthrosis into account.
The treatment of MWD is therefore definitively controversial, and there is no current scientific agreement as to which is the best. Different criteria exist regarding the therapeutic strategy and indications to be applied, although osteotomy techniques predominate over those involving arthrodesis. Further studies are therefore required to establish the best treatment, depending on the stage of the disease in each patient.
The limitations of our study consist of its observational and retrospective nature. The impact of MWD in the population may also be underestimated because it is hard to diagnose, while the majority of cases are treated conservatively in hospitals with specialized departments. Nevertheless, our study has the strength of being the second in terms of the number of patients selected to analyze this disease, and it is also one of the few to verify the epidemiological theory about the origin of MWD proposed by Maceira and Rochera.3
ConclusionsOur series supports the idea that MWD is a rare entity that becomes clinically clear towards the sixth decade of life. It affects women more often, and is bilateral in almost half of all cases.
The results obtained in our study support the aetiopathogenic hypothesis of Maceira and Rochera. We found a higher incidence of MWD among patients who were born around the time of the Spanish Civil War and the mass migrations which occurred in the fifth decade of the twentieth century.
There is still no clearly established treatment, although more than half of our patients obtained good results with conservative treatment. Respecting the surgical treatment of MWD, based on our clinical experience and with supported by the literature, we believe that calcaneal osteotomy should be considered to be the first choice, with arthrodesis as a rescue technique.
Level of evidenceLevel of evidence iv.
Ethical approvalThis study was approved by the Ethics Committee for Research with Medicines of the Hospital Clínico Universitario of Valencia (order number 2022/047). The verbal informed consent of all of the participants included in the study was obtained.
FundingNo financing was received for this work.
Conflict of interestsThe authors have no conflict of interests to declare.













![Year of birth of the patients in our series, compared with the 2004 series of Maceira and Rochera [1900–1990]. Adapted and reproduced with the permission of Maceira and Rochera.3 Year of birth of the patients in our series, compared with the 2004 series of Maceira and Rochera [1900–1990]. Adapted and reproduced with the permission of Maceira and Rochera.3](https://static.elsevier.es/multimedia/18884415/0000006700000005/v3_202404150741/S1888441523001492/v3_202404150741/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)