Describe the location of traumatic lesions of the oral mucosa that develop after the installation of complete dentures, as well as to quantify the number of post-operative controls that are required. A descriptive study was conducted by examining 84 patients who attended the dental center of Universidad de Los Andes, San Bernardo, during the period from July 2012 to July 2013. A sample of 120 edentulous patients was obtained. After the fabrication and installation of the complete dentures, at least 3 post-operative controls were performed and the location of oral lesions was recorded. Documentation of the association between the patient's clinical variables and the appearance of oral lesions during the first 3 controls was performed using a logistic regression.
ResultsFor maxillary dentures, 5 post-operative visits were made and 6 controls for mandible dentures. In the upper jaw the anatomical areas of higher incidence of traumatic injuries were: canine fossa (23.9%), average bridle (23.1%), and distobuccal sulcus (20.1%). In the lower jaw, the highest number of lesions were recorded on the anterior lingual flank (16.5%), anterior and posterior lingual flank (13.4%), and distobuccal sulcus (12.8%). A significant association was observed between subjects who reported consumption of cholesterol-lowering medications and the development of traumatic lesions of the oral mucosa (OR: 0.25 and 95% CI: 0.055–0.939). The installation of complete dentures does not determine that the treatment has ended. Post-operative controls are needed to assess areas of erythema and ulceration.
Describir la ubicación y frecuencia de las lesiones traumáticas de la mucosa oral que se generan después de la instalación de las prótesis dentales completas, y cuantificar el número de controles postoperatorios necesarios. Se realizó un estudio descriptivo, examinando a 84 pacientes que asistieron al centro dental de la Universidad de Los Andes, durante el período comprendido entre de julio de 2012 y julio del de 2013. Se obtuvo una muestra de 120 pacientes edéntulos. Después de la fabricación e instalación de las dentaduras completas se realizaron por lo menos 3 controles postoperatorios y la localización de las lesiones orales fue registrada. La documentación de la asociación entre las variables clínicas de los pacientes y la aparición de lesiones orales durante los 3 primeros controles fue realizado por medio de una regresión logística.
ResultadosPara prótesis maxilar 5 visitas de controles postoperatorios fueron realizados y 6 para mandibulares. En el maxilar superior las zonas de mayor incidencia de lesiones traumáticas fueron: fosa canina (23,9%), flanco medio (23,1%) y distovestibular del surco (20,1%). En la mandíbula se registraron mayor frecuencia de las lesiones en el flanco lingual anterior (16,5%), anterior y posterior (13,4%) y distovestibular del surco (12,8%). Una asociación significativa se observó entre los sujetos que reportaron consumo de medicamentos reductores del colesterol y el desarrollo de las lesiones traumáticas de la mucosa oral (o: 0,25 e IC: 0,055-0,939). La instalación de las prótesis dentales completas no determina que el tratamiento haya terminado. Los controles postoperatorios son necesarios para evaluar las áreas de eritema y ulceración.
The prevalence of edentulous patients worldwide varies in between 8.0% to 6.3%.1,2 In Chile, the 2003 national survey on health (ENS) revealed a national prevalence of 5.5%, and 33.4% in subjects over 65 years of age. These results are of great importance because the loss of teeth not only creates a negative impact on facial esthetics, but also produces alterations of mental state, oral language and nutrition of the elderly population, resulting in a decrease in the quality of life.3 The rehabilitation of the edentulous by means of removable complete dentures (PTR) has proven to be a successful, cost-effective therapeutic option capable of increasing the quality of life in these patients.4
The rehabilitation by means of dentures does not terminate after their delivery and installation.5 The day's posterior installation of the prosthetic devices is characterized as a period of discontent, were the stability, retention and support of the dentures is affected. This condition is reflected by the appearance of erythema and ulcerated lesions in relation to the supporting tissues of the prosthetic bases. For this reason, post-operative control visits are essential to assess both the acceptance of the dentures by the patient and the tissues adaptation to the prosthetic device.5–7
In this regard, there are two studies reported in literature, the first by the authors Kivovics et al. in Hungary (2007)4 and the second by Sadr et al. in Iran (2011),8 in which the number of controls necessary to identify areas of ulceration and discomfort, and control the functionality of the device was established posterior installation of the complete dentures.
On the other hand, it has been described that traumatic oral mucosal lesions vary significantly according to ethnicity, race and sex of the subjects in study,9 so that it is not possible to extrapolate the results of both studies to the commune of San Bernardo, place where the students of dentistry of University of the Andes carried out their clinical practice. In addition, variables that could influence the process of adaptation of the patient to the new devices during the first days posterior to installation have not been described, such as the systemic condition and use of pharmaceuticals. The level of pain perceived by patients in each prosthetic control in association with the appearance of traumatic injuries has not been described either.10
The apparition of traumatic lesions in the oral mucosa reflects a failure in between the adaptation of the acrylic prosthetic bases and the supporting prosthetic tissues associated. It is for this reason that locating areas of high frequency of occurrence of traumatic injuries can lead to an improvement in the method of confection, allowing to avoid or minimize discomfort and pain in patients during the immediate post-operative period as well as reducing the number of controls required to achieve a comfortable treatment.11
The purpose of the study is to describe the areas of higher frequency of occurrence of traumatic lesions of the oral mucosa during the postoperative installation of total prostheses or complete dentures in edentulous adults attending the dental center of San Bernardo in the Universidad de Los Andes. In addition, the purpose is to improve previous studies, considering variables that could influence the process of adaptation of the prosthetic device to the stomatognathic system, such as systemic condition, pharmaceutical therapies and materials used during the confection of the working cast, beside describing the level of pain reported by patients in each control.
Materials and methodsA transversal study was performed, in which all patients who required prosthetic attention for the confection of acrylic total prosthesis were considered, in the dental center of San Bernardo in Santiago – Chile during the months of July 2012 until July 2013. The study included adult edentulous patients, in one or both arches, of any age, gender, systemic condition or pharmacological therapy, who accepted to participate in the study and signed an informed consent. Patients presenting denture stomatitis, hyperplasia o inflammatory lesions of the mucosa and presence of irregularities or alveolar bone spicules where excluded.
The prosthetic treatment was performed by students of dentistry of University of the Andes, under the tutelage of 10 professors, specialists in oral rehabilitation.
During the medical history the students had to complete the following information: patient identification, age, gender, systemic condition and pharmaceutical therapy. Once patient and professor in charge approved the treatment plan, an anatomical impression was performed in order to make an individual acrylic tray. For the final or functional impression, the tray was subjected to a mechanical and functional trim with modeling compound, followed by the impression of the arcades with silicone or zinquenolic paste, according to the preferences of the operator and tutor. After obtaining the working cast, the models were mounted on a semi-adjustable articulator in muscular contact position. All the dentures where manufactured by the same dental laboratory. At the moment of installation stability, retention and support of the devices were revised making the necessary adjustments. At all patients at the time of installation are prosthetic suggests: soft diet until the prosthesis does not generate discomfort, bilateral chewing food if possible, avoid eating “adhesives” foods. Respect the use; Sleeping without prostheses; Clean after each meal with water and toothbrush without toothpaste; Denture adhesive use if necessary; If the prosthesis generates a painful ulcer can stop using it, but you must reinstall it 24h before the dental control.
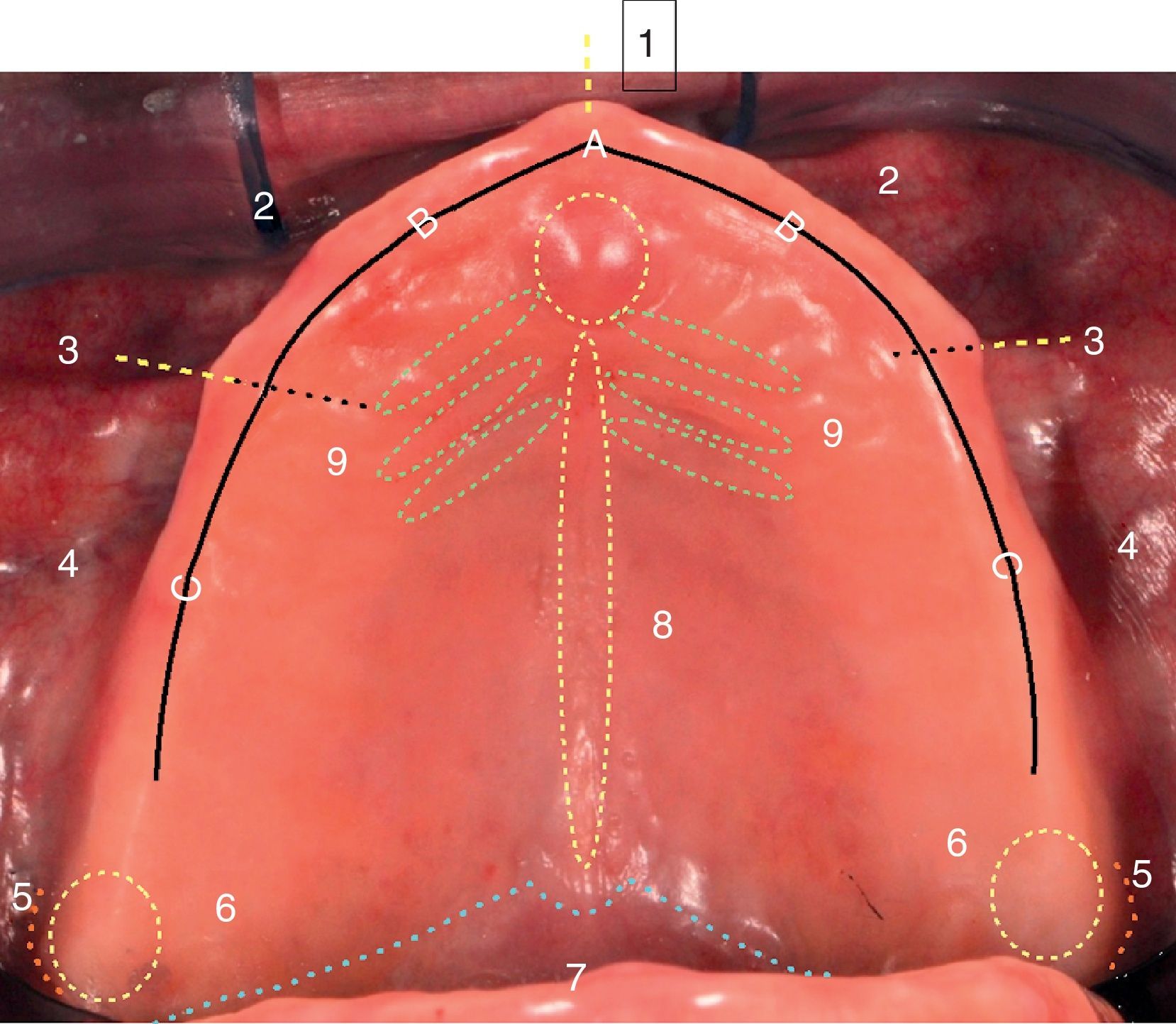
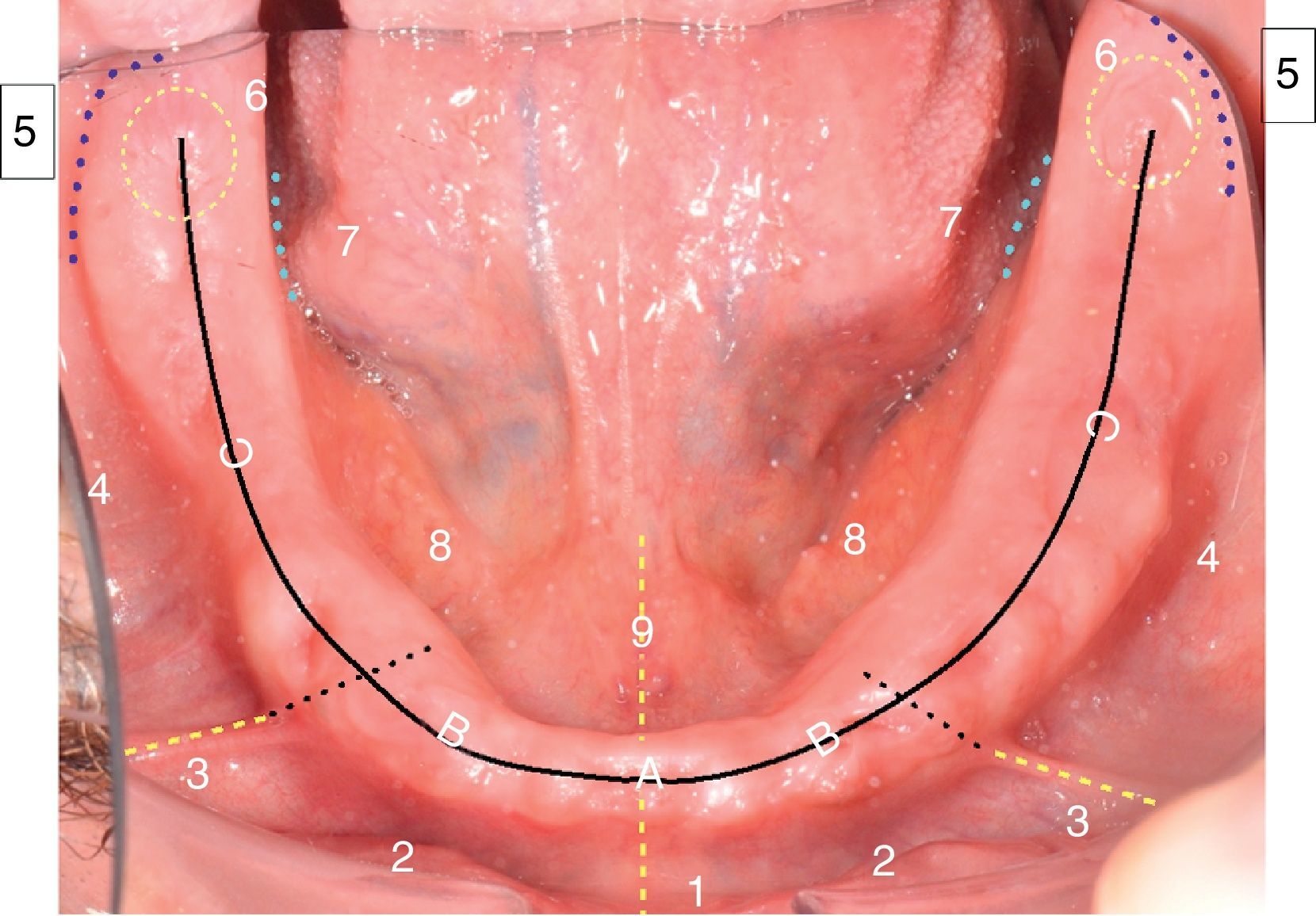
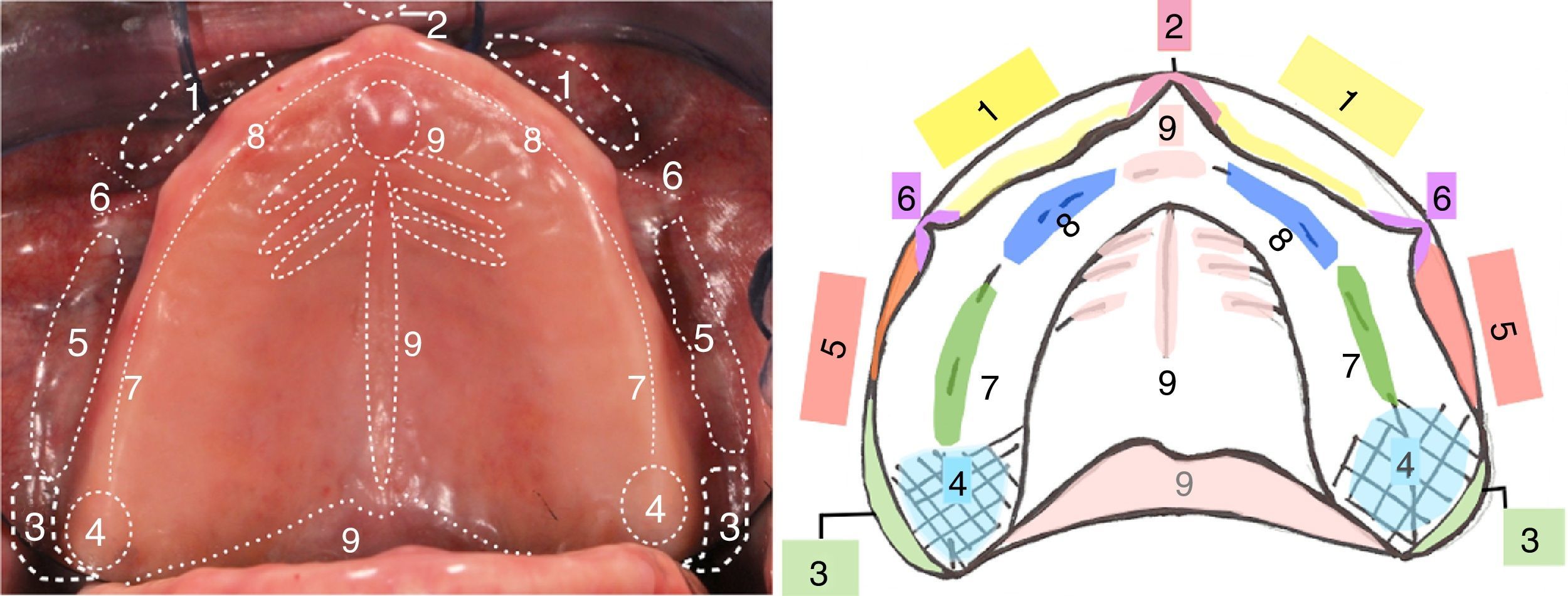
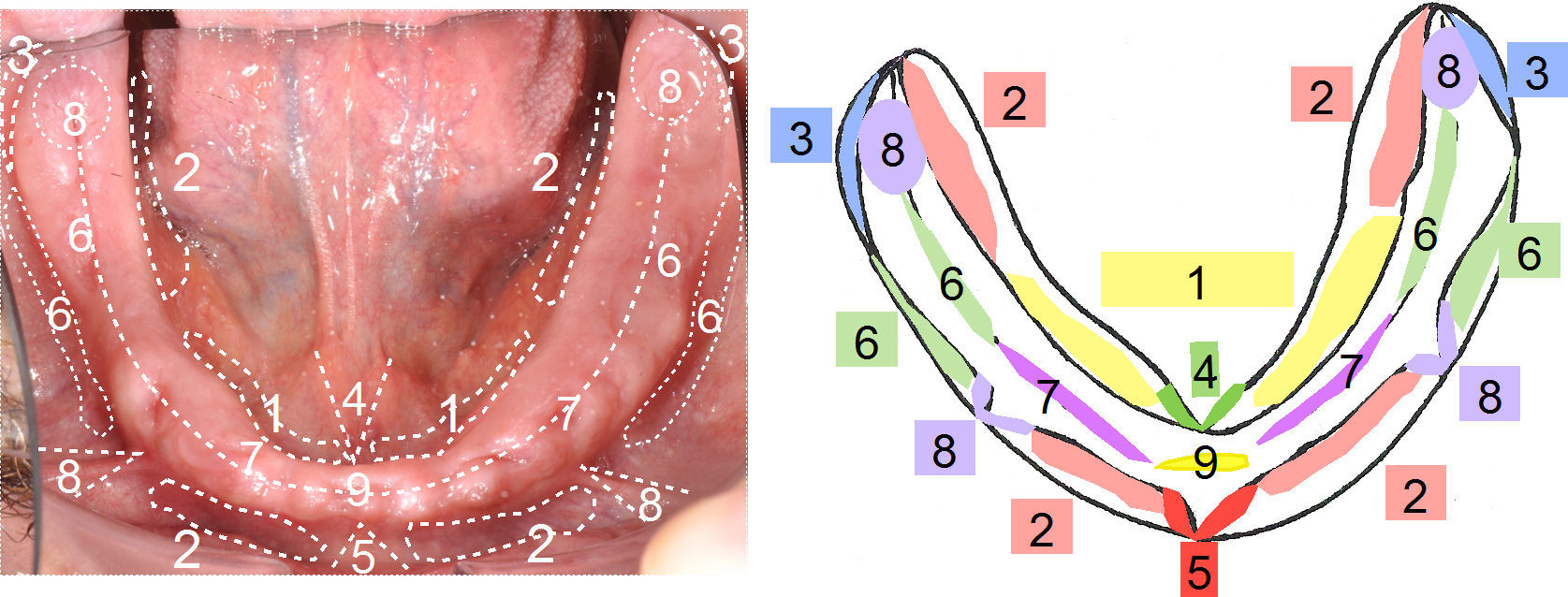
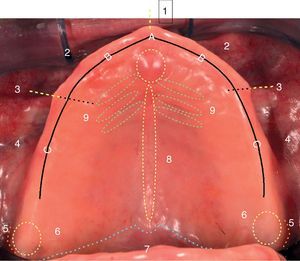
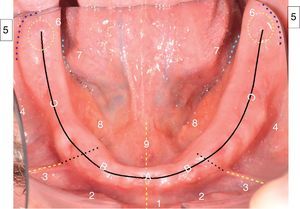
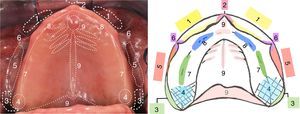
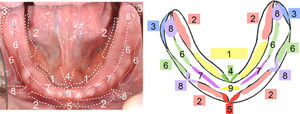
After the installation, the patients studied were cited in 3 opportunities (7, 14 and 21 days – in case of persistence ulcers, were added all necessary recalls) to assess the presence of traumatic lesions of the oral mucosa and the adaptation process. Most of the controls were performed on subjects who during the third control still presented areas of ulceration and/or erythema of the oral mucosa. In order to register the localization of traumatic injuries, the jaws were divided into anatomical sites according as shown below:
After the definition of the anatomical sites, two diagrams were made, one for the maxilla and one for the mandible (Figs. 1 and 2). The students were asked to register the presence or absence of lesions during each control. In the case of the presence of lesions, students had to color with yellow erythematous lesions and mark with red ulceration areas. Along with this, the perception of pain of the patient at the time of the control was recorded using the numerical verbal scale (EVN), in which patients qualify pain with a number between 0 and 10, 0 being “no pain” and 10 “worst pain imaginable”.
Zones of distribution of ulcers in maxila: 1: Middle bottom bridle, 2: Anterior vestibular, 3: Side bridle, 4: Posterior vestibular flank, 5: Distovestibular area, 6: Piriformis papilla, 7: Posterior lingual flank, 8: Anterior lingual flank, 9: Lingual frenum, A: Corresponds to the high area of the flanges, located in relation to the insertion of the middle bottom bridle. B: Corresponds to the Upper flanges, located between the insertion of the middle bottom bridle and side bridle. C: Corresponds to the upper flanges, located distal to the insertion of the middle bottom bridle.
Zones of distribution of ulcers in mandible: 1: Medial lower frenulum, 2: Anterior vestibular flank, 3: Side bridle, 4: Posterior vestibular flank, 5: Distovestibular area, 6: Piriformis papilla, 7: Posterior lingual flank, 8: Anterior lingual flank, 9: Lingual frenulum, A: Corresponds to the high area of the flanges, located in relation to the place of insertion of the middle bottom bridle. B: Corresponds to Upper flanges, located between the insertion of the middle bottom bridle and side bridle. C: Corresponds to Upper flanges, located by distal to the insertion of the middle bottom bridle.
After the injury registration, the students proceeded to adjust the prostheses according to the areas previously marked. This information was completed in the successive controls until the patient was discharged, in absence of pain symptoms or mucosal lesions.
Statistical analysisThe categorical variables were described using frequencies and percentages, while the quantitative variables were described with measures of central tendency, dispersion and position.
We explored the association between the presence of at least one traumatic injury in the maxilla and/or mandible during the first 3 postoperative controls and the systemic condition and pharmaceutical therapy, in addition to the final impression material used. Fisher's exact test was applied to evaluate the existence of association, considering a statistically significant in cases where P value was less than 0.05. Cases where the association was positive were analyzed using a logistic regression model, odds ratio (OR), with a respective 95% confidence interval.
Ethical aspects included the following:
- 1.
Informed consent of patients who entered the study and those who authorized the use of intraoral photographs in this document.
- 2.
Management of the databases in a confidential and anonymous manner.
- 3.
This study was approval of the subcommittee on ethics of the dentistry faculty of the Universidad de los Andes.
A sample of 84 edentulous patients was obtained consisting of a total of 120 edentulous arches. Of these, 82 corresponded to upper arches and 38 lower arcades. 28.6% (n=24) of the subjects belonged to the male gender and 71.4% (n=60) to the female gender. The average age of the patients was 67 years old.
In regard to the systemic conditions, 54.8% confirmed diagnosis of high blood pressure, 23.81% diabetes mellitus and 15.5% hypercholesterolemia. Regarding pharmaceutical therapy, 53.6% reported using antihypertensive drugs, 20.2% hypoglycemic drugs and 14.3% lipid-lowering drugs. An association was observed between the patients who reported suffering from hypercholesterolemia and the presence of injuries during the postoperative period with an OR of 0.25 and an IC of 0.0622845–1.00345. A statistically significant association was also found between patients who consumed lipid-lowering drugs and the presence of traumatic injuries during the first 3 postoperative controls with an OR of 0.25 and an IC of 0.0559247–0.9390921.
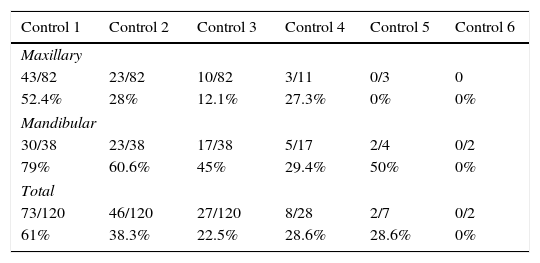
52.4% of the maxillary dentures and 79% of the mandibular dentures required at least one prosthetic fitting during the first postoperative control. The amount of adjustment necessary decreased during the 3 controls, as well as the symptoms of pain expressed by the EVN. In total, up to 5 controls were made in the upper jaw and up to 6 controls in case of mandibular dentures (Table 1).
Number of dentures that required prosthetic adjustments per control after installation.
| Control 1 | Control 2 | Control 3 | Control 4 | Control 5 | Control 6 |
|---|---|---|---|---|---|
| Maxillary | |||||
| 43/82 | 23/82 | 10/82 | 3/11 | 0/3 | 0 |
| 52.4% | 28% | 12.1% | 27.3% | 0% | 0% |
| Mandibular | |||||
| 30/38 | 23/38 | 17/38 | 5/17 | 2/4 | 0/2 |
| 79% | 60.6% | 45% | 29.4% | 50% | 0% |
| Total | |||||
| 73/120 | 46/120 | 27/120 | 8/28 | 2/7 | 0/2 |
| 61% | 38.3% | 22.5% | 28.6% | 28.6% | 0% |
A total of 134 adjustments were made in maxillary dentures, from which 56.7% were carried out during the first control, 29.1% during the second and 10.4% during the third.
With respect to the location of the traumatic lesions, 23.9% lesions were observed in the canine fossa, being the area with the highest occurrence of lesions, followed by the average bridle area (23.1%) and third in frequency the area of the flank zone of the hamular groove with 20.1% and the distovestibular area (Fig. 3). In terms of the severity of injuries, in general, ulcers showed a higher frequency of apparition (53%, n=71) versus erythematous areas (47%, n=63).
In mandibular jaws, a total of 164 adjustments were made, of which 40.9% were carried out during the first control, 32.9% during the second, and 18.9% during.
16.5% of the lesions were observed on the anterior lingual flank, being the site of highest prevalence. On the posterior lingual flank and anterior vestibular flank a 13.4% of lesions was observed. The fourth highest affected site was the distovestibular angle with an average of 12.8% (Fig. 4).
An increased frequency of erythematous lesions was observed (61 percent, n=100) in comparison with areas of ulceration (39%, n=64).
On the other hand, no statistically significant association was observed between the final impression material used, whether zinquenolic paste or silicone, and the appearance of lesions during the first postoperative controls.
DiscussionThe number of prosthetic adjustments necessary depends on various factors such as quality and quantity of residual flange, health of the mucosa covering the residual flanges, capacity of adaptation of the patients, relationship in between the arches and the clinical and laboratory skills.4 In this study it was observed that 60.8% required adjustments during the first control, reducing to one third in the second visit and less than a quarter during the third visit. However, the results do not match with similar studies conducted by Sadr et al. and Kivovics et al., who observed a higher percentage of adjustments during the first control (85.8% and 87% respectively). This discrepancy can be explained because both authors examined more mandibular prostheses than the present study. In addition, both observed that mandibular dentures required significantly more settings than the maxillary; which could be the reason why a higher percentage of adjustments were observed during the first control.
The total number of controls performed are similar to that published by Sadr et al., who reported at least 5 postoperative visits in the maxilla, and 7 in the mandible.
The final impression is considered one of the most critical stages during the process of fabricating dentures. Drago et al. reported no significant differences in terms of the number of control visits that patients required comparing different impression techniques. This study did not notice either significant differences between the use of zinquenolic paste or silicone in association with the presence of lesions, suggesting that the material is not a determinant in the appearance of traumatic injuries and that studies should be designed to evaluate the type of material and the quality of impressions to confirm this affirmation.
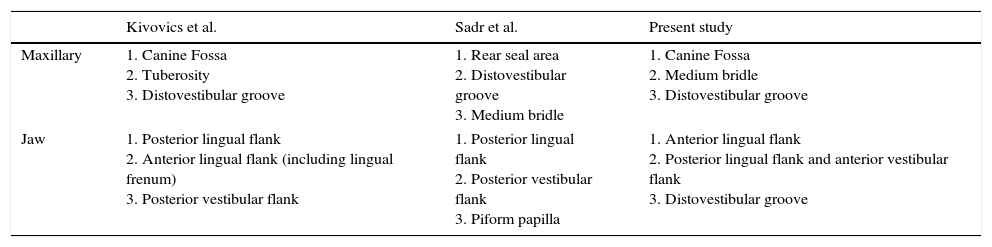
The present result of greater occurrence of traumatic injury sites disagrees with the results of previous publications. This may be due to the fact that the samples came from different countries and different ethnic groups and races (Table 2). In the mandible, when comparing with previous publications, there is a tendency of apparition of traumatic lesions on the anterior lingual zone, posterior vestibular flank and lingual rear (Table 3). Whereas in the upper jaw there is a tendency of apparition of trauma in certain areas of the maxilla, such as the fossa canine, half bridle and distovestibular groove, although the frequency of appearance is different in each article (Table 3).
Areas of increased frequency of occurrence of traumatic lesions of the oral mucosa during the immediate post-op of dentures.
| Kivovics et al. | Sadr et al. | Present study | |
|---|---|---|---|
| Maxillary | 1. Canine Fossa 2. Tuberosity 3. Distovestibular groove | 1. Rear seal area 2. Distovestibular groove 3. Medium bridle | 1. Canine Fossa 2. Medium bridle 3. Distovestibular groove |
| Jaw | 1. Posterior lingual flank 2. Anterior lingual flank (including lingual frenum) 3. Posterior vestibular flank | 1. Posterior lingual flank 2. Posterior vestibular flank 3. Piform papilla | 1. Anterior lingual flank 2. Posterior lingual flank and anterior vestibular flank 3. Distovestibular groove |
In relation to the systemic condition of the subjects studied, Zarb et al. and cols. describe that all subjects were around 75 years of age and possessed at least one chronic disease, limiting there access to dental care.6 Various systemic conditions generate a decrease in mucosal resistance to mechanical irritation, which predisposes these patients to the development of traumatic injuries.2 An example of this is diabetes mellitus, which includes a group of metabolic disturbances that also have in common the presence of hyperglycemia. An increased glucose level in the blood generates an impact in the oral cavity that predisposes to: hyposalivation, increased susceptibility to infections and difficulty of healing. Due to the alteration of the healing process, one might expect a higher prevalence of injuries of the oral mucosa after installation of dentures in diabetic patients. In the present study, no statistically significant association was observed between the presence of traumatic lesions of the oral mucosa during the first three post-installation controls and the diagnosis of diabetes.
Considering the limitations of this descriptive study, it is important to emphasize, once again that the installation of the dentures should not be the last occasion in which patient and professional encounter. Post-operative visits are essential in order to browse the areas of dissatisfaction and pain and to correct the etiological factors. After the installation, the patients should regularly be evaluated in order to be able to control the process of adaptation of the patient to the prosthetic device. Among the future prospects it would be interesting in a subsequent study evaluating bimaxillar toothless, since the presence of natural teeth “antagonistic” conditions rather the presence of injuries in the mucosa that supports the prosthesis.
The installation of complete dentures does not determine that the treatment has ended. Post-operative controls are needed to assess areas of erythema and ulceration.
Conflict of interestsThe authors declare no conflict of interest.