Despite of separate diagnostic criteria given by International Headache Society Beta-3 for Migraine and Cervicogenic Headache, there are chances of symptoms getting overlapped with each other. Moreover, there are chances of presence of these two types of headaches in conjunction in sufferers. The solo type treatment of headache will not be satisfactory for patients.
MethodsThirty-one participants with clinical diagnosis of migraine were enrolled in this cross-sectional study. All participants underwent physical examination for cervicogenic headache using the International Headache Society Diagnostic Criteria (IHS). The side and site of pain during headache, associated neck pain, tenderness, restricted range of motion, cervical spine posture and Flexion Rotation Test (FRT) were assessed. The data were analyzed with chi square test and expressed as mean and SD.
ResultsA statistically significant association were found between Neck Pain and FRT [X2 (3)=13.527, p=0.004] at 0.05 significance level. The results of the study have shown that cervicogenic headache features also present in migraine population. There was no association between FRT with other variables like age, gender and side of pain. But FRT and neck pain were correlated to each other.
ConclusionThe possible symptoms were present in migraine and cervicogenic headache together in patients. But focusing on one type (primary) only will lead to missed or under diagnosis of other (secondary). Appropriate diagnostic criteria should be used during assessment of patient complaining about headaches to rule out diverse type of headache; it will help to differentiate headache types and will improve the treatment strategies in patients.
A pesar de los criterios de diagnóstico separados dados por la International Headache Society Beta-3 para la migraña y el dolor de cabeza cervicogénico, existe la posibilidad de que los síntomas se superpongan entre sí. Además, puede darse la presencia de estos 2 tipos de dolores de cabeza conjuntamente en los pacientes. El tratamiento del dolor de cabeza en solitario no será satisfactorio para los pacientes.
MétodosTreinta y un participantes con diagnóstico clínico de migraña se inscribieron en este estudio transversal. Todos los participantes se sometieron a un examen físico por dolor de cabeza cervicogénico utilizando los criterios de diagnóstico de la International Headache Society. Se evaluaron el lado y el lugar del dolor durante el dolor de cabeza, el dolor de cuello asociado, la sensibilidad, el rango de movimiento restringido, la postura de la columna cervical y la prueba de rotación en flexión (FRT). Los datos se analizaron con la prueba de chi cuadrado y se expresaron como media y desviación estándar.
ResultadosSe encontró una asociación estadísticamente significativa entre el dolor de cuello y la FRT (χ2 [3]=13,527, p=0,004) a un nivel de significación de 0,05. Los resultados del estudio han demostrado que las características del dolor de cabeza cervicogénico también están presentes en la población con migraña. No hubo asociación entre FRT y otras variables como edad, sexo y lado del dolor. Pero la FRT y el dolor de cuello se correlacionaron entre sí.
ConclusiónLos posibles síntomas estuvieron presentes de forma conjunta en la migraña y la cefalea cervicogénica en los pacientes. Pero centrarse en un tipo (primario) solo conducirá a que se pierda o no se diagnostique el otro (secundario). Se deben utilizar criterios de diagnóstico apropiados durante la evaluación del paciente que se queja de dolores de cabeza para descartar los diversos tipos; esto ayudará a diferenciar los tipos de dolor de cabeza y mejorará las estrategias de tratamiento en los pacientes.
Headache is a common and most prevalent pain disorder affecting a large proportion of society these days. As per an International Headache Society (IHS) classified headache as primary; where no causative factor is found and secondary where other factors contribute to the headache; apart from original cause or disorder. The term ‘migraine’ originally comes from Greek word hemicrania which means ‘half of the head’ that represents one of the most important clinical features of migraine. In most of these cases headache affects unilaterally. But also in some cases it's been observed as bilateral pain either back of the head or front of head.1 Neck pain is frequently been reported by migraineurs preceding or during their attacks. Neck stiffness, forward head posture, trigger points in cervical musculature have been identified in patients with migraine.2–4 In current time period migraine is most common disability seems as an inconvenience to the sufferers.
Cervicogenic headache, a secondary headache disorder, have been characterized by presence of unilateral cranial pain that is dispersed/referred to the head from musculoskeletal disorders of cervical spine.5 Cervicogenic headache have been associated with neck pain, epsilateral arm pain or discomfort and reduced cervical range of motion.6 The symptoms of cervicogenic headache sometimes may mimic as those of primary headaches like tension type headache, migraine such as dizziness, neck pain. Therefore, a proper diagnostic criterion is of utmost importance to differentiate cervicogenic headache from other primary forms of headache.
Features of cervicogenic headache sometimes correlate with that of migraine, such as: typical unilaterality of pain, neck pain, stiffness of neck. Therefore an apparent diagnosis as well as treatment, whether medical or physiotherapy, of either of headache become crucial in clinical practice.7–9 Despite having specific diagnostic criteria, symptoms can overlap between cervicogenic headache and migraine population. There can be presence of cervicogenic headache in conjunction with migraine headaches in sufferers. The treatment of migraine symptoms only will not be satisfactory for the patients.
This study was intended to identify the presence of cervicogenic headache features in migraine patients which allow us to understand the possibilities of missed or under diagnosis of cervicogenic headache. Careful evaluation and greater awareness of some of cervicogenic headache features as associated symptoms of migraine may improve diagnostic accuracy and have a beneficial impact on time to treatment
MethodsStudy design and setting: This study employed an Observational research design. The study was conducted at Out Patient Department of School of Physiotherapy and Paramedical Sciences, Lovely Professional University, Punjab, India. The approval from the Institutional Ethics Committee, Lovely Professional University, Punjab was obtained prior to data collection. Consent was taken beginning of the study in written format from each participant at Out-patient Physiotherapy Department, School of Physiotherapy and Paramedical Sciences, Lovely Professional University, Punjab, India.
Participants: Eligibility criteria were history of migraine and neck pain. A convenient sampling method was used for the selection of participants. Total 40 subjects were approached for this study. Out of them 31 participants meeting the inclusion/exclusion criteria i.e. provisional diagnosis of migraine, either gender, aged between (18–40yrs), no past history of whiplash injury were enrolled for the study.
Procedure: People who have been diagnosed with migraine by general physician were eligible for the study. Participants were contacted via pamphlets for invitation of free checkup for headache and neck pain which were posted on notice boards of different departments of the university. Final sample of participants was assessed for presence of cervicogenic headache features by using International Headache Society Cervicogenic Headache Diagnostic Criteria and a statistical analysis were made.
Variables: This study was imposed to find out the important features of cervicogenic headache in migraine patients using the diagnostic criteria for the former given by ICHD-Beta 3. The potential confounder in this study could be the chronicity of the migraine. As many studies have found the direct relation of neck pain with the chronicity of the migraine. With the chronicity of migraine, the intensity of neck pain gets worse. The acute and chronic status of migraine in patients was not assessed and involved in this study.
Statistics: The statistical analysis was done using SPSS (version-16). The following are the statistical formulas and tools which were used during the analysis of data. Mean, Frequency, Mode and Standard Deviation were analyzed. Chi-square Test of association which is used to check if there is any relationship or association between two categorical variables.
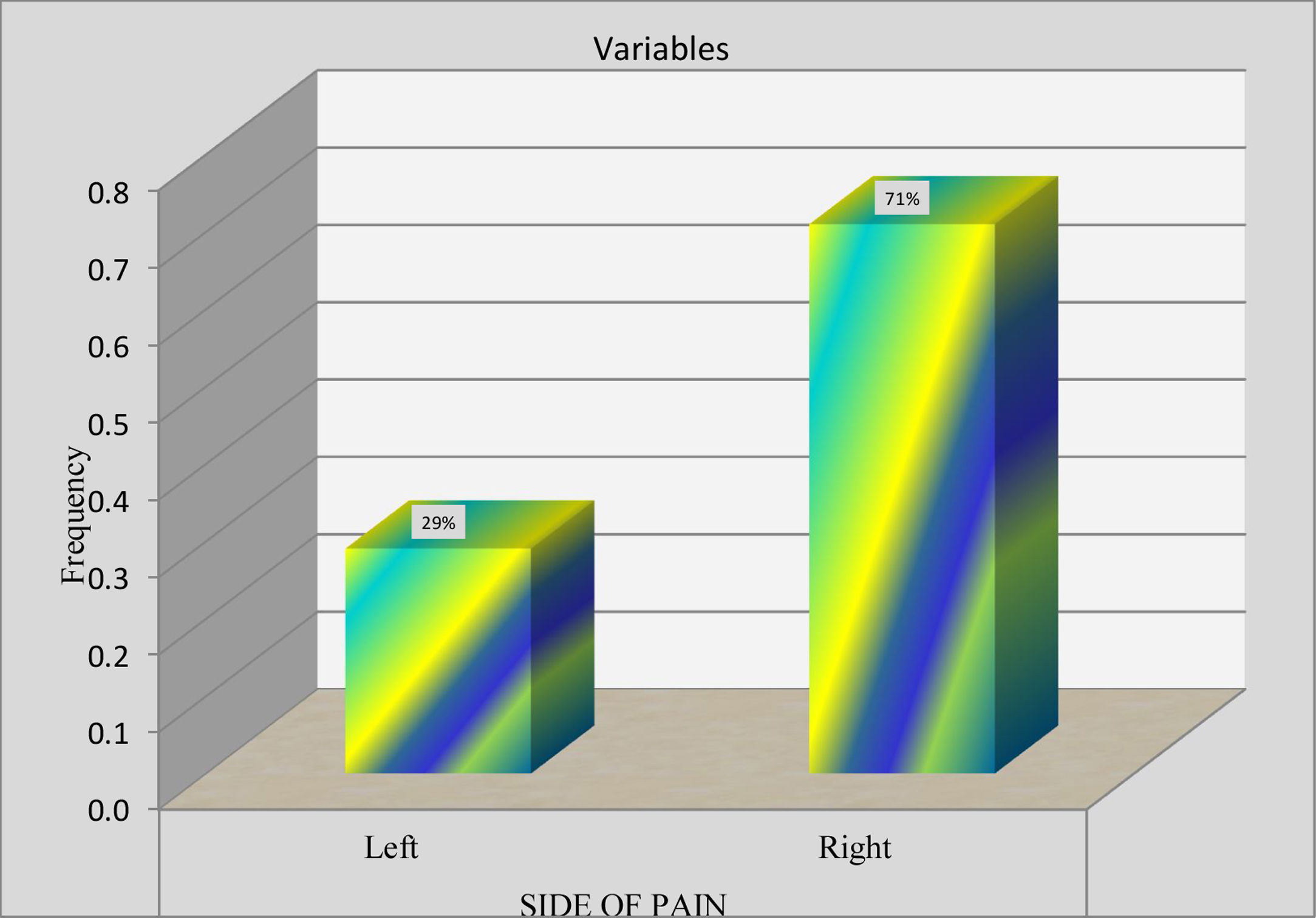
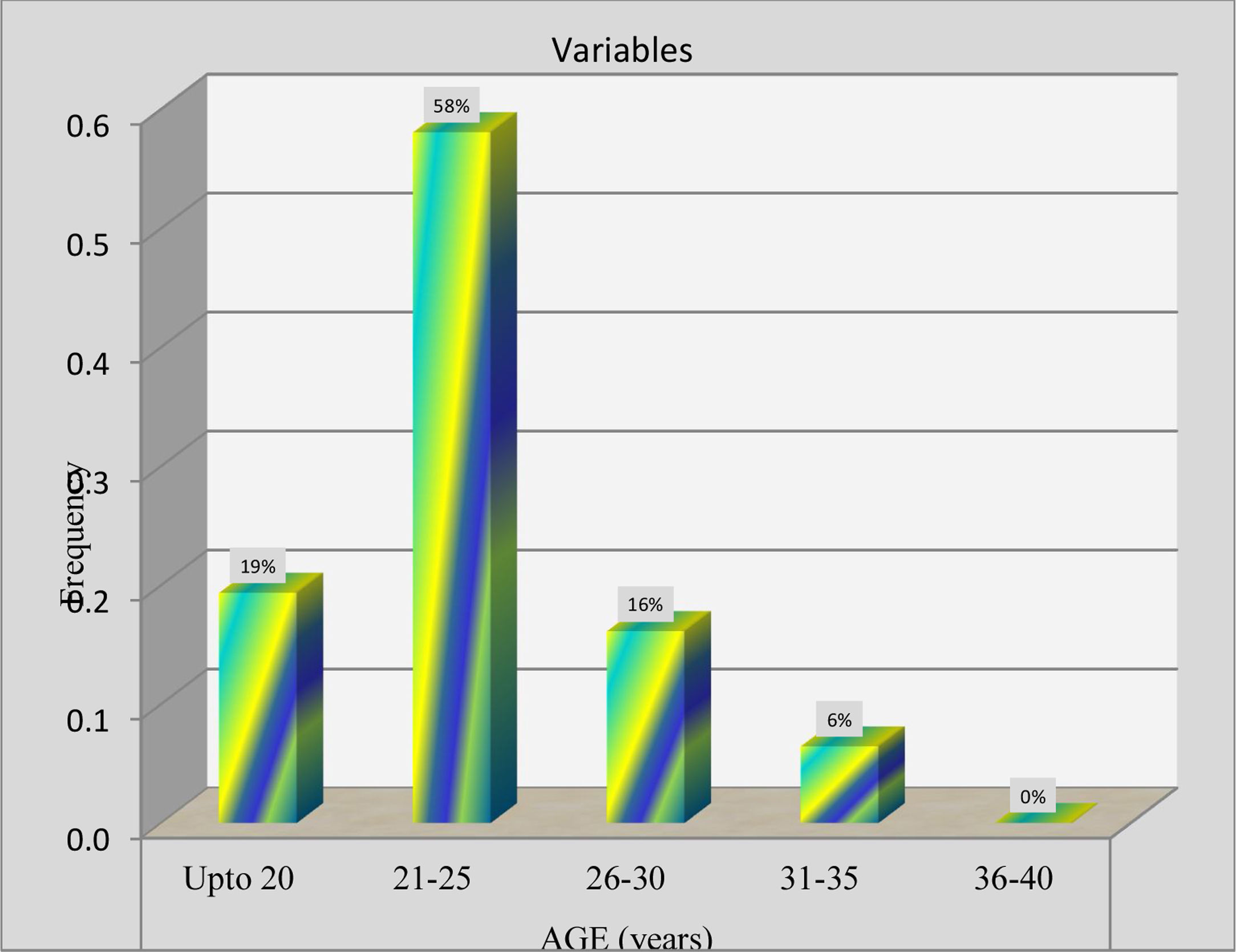
ResultsThe results of the study have been reported for total 31 subjects 18–40 years with clinical diagnosis of migraine were included in the statistical analysis. Out of total subjects 74% were Female and 26% were Male indicating that the prevalence of migraine is high in Females than Males. The 71% of subjects reported pain on right side and 29% on left Side. On other hand 61% of the subjects reported pain that was arising from frontal to occiput bone and 39% from occiput to frontal bone area. Associated neck pain was seen in 81% of subjects with their headache episodes and 19% were not reported any pain.
Seventy percentage of subjects had Sub-occipital muscle tenderness and 30% subjects had no sub-occipital muscle tenderness. The 90% of the total subjects had Upper Trapezius Tenderness and 10% of the total subjects had no upper trapezius tenderness. 65% of the total subjects showed Positive FRT results, out of them 13% had positive FRT bilaterally, 10% had positive FRT on left side, 42% had positive FRT on right side and 35%showed negative FRT results. 81% had restricted neck range of motion of (Rotation mainly) either bilateral or unilateral. 29% of the subjects had restricted neck Extension as well. 52% of the total subjects had Forward Head Posture as observed and 48% had a normal cervical spine posture.
Chi- Square Test was used to check out any association between the different variables. The results were shown that there was no statistically significant association between Age and FRT [X2 (9)=11.396, p=0.250] at 0.05 significance level. A significant association was found between Neck Pain and FRT [X2 (3)=13.527, p=0.004] at 0.05 significance level. There was no significant association between Gender and FRT [X2 (3)=5.485, p=0.140] at 0.0.5 significance level. There was no significant association found between Side of Pain and FRT [X2 (3)=4.209, p=0.240] at 0.05 significance level (Tables 1–6).
Flexion rotation test.
| Variables | Opts | Percentage | Frequency |
|---|---|---|---|
| Frt | Negative | 35% | 11 |
| Positive-BL | 13% | 4 | |
| Positive-L | 10% | 3 | |
| Positive-R | 42% | 13 |
BL, bilateral; L, left; R, right.
The above describes the distribution of flexion rotation test (FRT) results among the subjects of study. 65% (n=20) of the total population showed positive FRT, out of which 13% (n=4) had positive FRT on both sides and 52% (n=16) had positive FRT on either side. Rest 35% (n=11) of subjects had negative FRT results.
Association between age and FRT.
| Demographic data | Age (years) | Association with …. | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Opts | Up to 20 | 21–25 | 26–30 | 31–35 | 36–40 | Chi test | p value | df | Table value | Result |
| FRT | Negative | 3 | 7 | 1 | 0 | 0 | 11.396 | 0.250 | 9 | 16.919 | Not significant |
| Positive-BL | 0 | 3 | 1 | 0 | 0 | ||||||
| Positive-L | 2 | 0 | 1 | 0 | 0 | ||||||
| Positive-R | 1 | 8 | 2 | 2 | 0 | ||||||
| Normal | 1 | 10 | 3 | 1 | 0 | ||||||
The above table describes the association between age and FRT interpretation. The statistically calculated chi test value (11.396) is less than the table value (16.919) at 0.05 level of significance indicates that there is no statistically significant association between age and FRT interpretation.
Association between neck pain and FRT.
| Demographic data | Neck pain | Association with …. | ||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Opts | N | Y | Chi test | p value | df | Table value | Result |
| FRT | Negative | 6 | 5 | 13.527 | 0.004 | 3 | 7.815 | Significant |
| Positive-BL | 0 | 4 | ||||||
| Positive-L | 0 | 3 | ||||||
| Positive-R | 0 | 13 | ||||||
| Mild rotation on left side | 0 | 1 | ||||||
| Mild rotation on right side | 0 | 1 | ||||||
| None | 5 | 1 | ||||||
This table describes the association between neck pain and FRT interpretation. The statistically calculated chi test value (13.537) is more than the Table value (7.815) at 0.05 level of significance indicates that there is statistically significant association between Neck Pain and FRT.
Previous studies have discussed about these considerations that there are chances of cervicogenic headaches being missed or under diagnosed in a migraine population.8,10 This study was based upon these assumptions and the findings of this study were supporting the main hypothesis of this study. Most of the study subjects possessed cervicogenic headache symptoms as well which means both type of headaches was present in conjunction in the subjects of this study. The treatment of both types of headaches is required to relive the symptoms of patients.
The symptoms of migraine and cervicogenic headache share some common characteristics like neck pain, half side pain in cranium, pathophysiological basis sometimes. There are chances of getting one of the headaches being under diagnosed or missed from diagnosis or there are chances of presence of these two types of headaches being present in conjunction in patients. The proper diagnosis of both type of headaches is of crucial importance for differential diagnosis and for treatment purposes. The consideration of only primary headaches in patients will not get them the satisfactory results and their symptoms relief.
LimitationsThe sample size of this study was small. Duration of smart phone, laptop's usage was not considered in this study. The chronicity of migraine was not considered in this study. As these factors could also alter the findings in subjects.
Future scopesThe prevalence of both types of headache can be assessed in targeted gadgets using population. The domains of assessment of cervicogenic headache can be modified further in future like pain pressure threshold, mechanosensitivity of neural tissues, a craniocervical flexion test can be assessed and a quantitative data can be obtained and the diagnosis can be made more accurately.
ConclusionThis study showed that migraine patients possess some characteristics of cervicogenic headache like direction of pain, tenderness, positive flexion rotation test result, restricted range of motion, forward head posture which means that the migraine and cervicogenic headache symptoms can be present in conjunction. There are chances of cervicogenic headache being missed or under diagnosed in migraine population. This study will account for focusing more on accurate and keen diagnosis for both types of headache and acceptance of the presence of both types in conjunction with in migraine patients (Figs. 1 and 2).
Authors’ contributionsVandana: Contributed in data curation, formal analysis, methodology and investigation.
Durga Prathap: Contributed in conceptualization, project administration, and supervision.
Thiagarajan Subramanian: Contributed in writing review and editing.
Clinical relevanceClinical implications:
- 1.
Undiagnosed/underdiagnosed secondary type headaches.
- 2.
Overlapping symptoms of migraine and cervicogenic headache.
Institutional Ethics Committee, Lovely Professional University, Punjab, has approved this study with approval number “LPU/IEC/2018/02/01”.
FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declared that there was no potential conflict of interest.