The aim of this study was to determine the incidence of central venous catheter-related bloodstream infection (CRBSI) in a general hospital, using two different assessment methods.
MethodsMethod A: One observer prospectively followed up all patients with central venous catheters (CVCs) placed in our hospital over a period of 1 year, recording all CRBSI episodes. Incidence was calculated in two ways, in relation to the total number of catheter days, and in relation to the total number of hospital days of all patients hospitalized during this period. Method B: Another observer recorded all CRBSI episodes diagnosed during the same time period using microbiology data in which blood culture and catheter culture were positive for the same microorganism. Incidence was calculated in relation to the total number of hospital days of all hospitalized patients.
The patient's demographic characteristics and the catheter-related variables were recorded and analysed. Based on clinical and microbiological criteria, catheters were classified as uninfected, colonized, or CRBSI.
ResultsOver the study period, 878 central venous catheters were placed in 704 patients. The total number of catheter days was 7357, and the mean duration of catheter use was 8.15 days (1–86). The total number of hospital stays in this period was 92,167.
Method A: 15 episodes of CRBSI were detected, yielding an overall incidence of 2.03 episodes/1000 catheter days or 0.16 episodes/1000 hospital days. Method B: 11 episodes of CRBSI, with an incidence of 0.12 episodes/1000 hospital days.
ConclusionThe two methods studied yielded different CRBSI rates, with a higher incidence reported by prospective follow-up (Method A). In addition, this method enabled a better assessment to be made of CRBSI risk as the calculation could be performed in relation to the days patients were catheterized.
El objetivo de nuestro estudio es medir la incidencia de bacteriemia por catéter venoso central (BRC) en un hospital general mediante dos métodos de valoración diferentes.
MétodosMétodo A: seguimiento prospectivo de todos los pacientes con catéteres venosos centrales (CVC) insertados en nuestro hospital durante 1 año, registrando los episodios de BRC. Datos referidos al total de días de catéter y al total de estancias hospitalarias en este período.
Método B: registro de los episodios de BRC por otro observador a partir de hemocultivos y de cultivo de catéter positivos al mismo microorganismo durante el mismo periodo de tiempo, datos proporcionados por microbiología y referidos al total de estancias hospitalarias.
Se registraron las características demográficas de los pacientes y las características de los catéteres. Según criterios clínicos y microbiológicos, los catéteres se clasificaban en: no infectado, colonizado, o bacteriemia por catéter (BRC).
Resultados878 CVC se colocaron a 704 pacientes. Total de días de cateterización de 7.357, y duración media de la inserción de 8,15 días (1–86). El total del número de estancias hospitalarias fue 92.167.
Método A: se detectaron un total de 15 episodios de BRC. Incidencia global de BRC de 2,03 episodios/1.000 días de catéter o 0,16/1.000 estancias hospitalarias.
Método B: 11 episodios de BRC, tasa de 0,12/1.000 estancias hospitalarias.
ConclusiónObservamos diferencias relevantes en las tasas de BRC obtenidas según el método de valoración empleado, siendo superior el método A. Además, el seguimiento prospectivo de los pacientes cateterizados permite una mejor valoración del riesgo de BRC al referir el resultado a días de cateterización.
Central venous catheter-related bloodstream infection (CRBSI) is an important cause of nosocomial infection, with significant associated morbidity and mortality.1–3 In the prevalence study of nosocomial infection in Spain (EPINE), the CRBSI rate in our country ranged from 2.5 to 3.4 episodes per 1000 hospitalized patients, and was the most common cause of nosocomial bacteremia.1 These infections increase the mean length of hospital stay by approximately 6–12 days, and have an attributable mortality of 20–24%.3,4
Prevention of CRBSI is an essential objective when these devices are required. The type of catheter, reason for its use, and manner in which it is used, as well as the specific characteristics of the patient in whom it is placed, are all factors affecting the risk of infection. Therefore, it is not surprising that CRBSI rates differ according to the institution and healthcare unit under study.6 Knowledge of the CRBSI rate in a particular center is the first step toward assessing the success of existing measures to prevent these infections and the need for further corrective measures.
A large number of studies8,13,15–17 have calculated CRBSI incidence rates in relation to the duration of catheterization. However, various registries in our country calculate incidence in relation to the total number of days all patients are hospitalized in a center and not the days of catheter use, which actually corresponds to the true period when a patient is at risk of acquiring an infection related to the device.1,5 This practice can underestimate the true incidence of CRBSI and make comparisons between different patient series difficult. Furthermore, in many hospitals, it is common practice to assess CRBSI rates from daily follow-up of all bacteremic episodes by an expert physician.
Considering this background, a comparative study was designed to determine the performance of two methods for establishing CRBSI rates in patients hospitalized during the same time period: prospective follow-up from catheter placement to removal, with daily clinical evaluation and recording of the situations in which infection occurred, and recording of CRBSI episodes using information provided by the microbiology laboratory, in which a patient's blood culture and catheter tip culture tested positive to the same microorganism.
MethodsThe study was conducted in a 348-bed general hospital, attending a catchment population 220,000 inhabitants in a peripheral area of Barcelona, and equipped with hospitalization units for all major medical specialties except nephrology and dialysis, and all major surgical specialties except cardiac, thoracic, and neurological surgeries. Our hospital has a general intensive care unit with 14 beds.
The hospital protocol for insertion, management, and removal of central venous catheters is based on the recommendations of the Healthcare Infection Control Practices Advisory Committee of the Centers for Disease Control and Prevention (HICPAC-CDC, 2002).7 A surveillance team for nosocomial infection periodically disseminates these guidelines to the staff and supervises the manipulation and maintenance of catheters. In the ICU, inserted catheters are closed with a disinfectable, needle-free mechanical valve connector, and a trained nursing team is responsible for assuring proper manipulation of the devices.8 Catheters used on the hospital wards are closed with a three-way valve.
Between February 2007 and February 2008, all patients in whom a central venous catheter (CVC) was placed during hospitalization were included in the study. We excluded pediatric patients (age<14 years), adults who already had a CVC at hospital admission, and psychiatric patients. The days hospitalized corresponding to these patients were excluded from the total days of hospitalization in the calculation of incidence density.
The incidence density of CRBSI was evaluated using two different methods for detecting this infection. The first consisted of prospective daily follow-up of each patient using a CVC, with recording of data on when the device was removed and for what reason (method A). The second involved evaluation of CRBSI according to data from the microbiology laboratory documenting blood- and catheter tip-positive status to the same microorganism in a hospitalized patient (method B) in an interval of 48h. All cases of bloodstream infection were evaluated jointly by a nurse involved in nosocomial infection control and an expert physician, in order to determine whether the infection was related to the catheter.
During the study period, bacteremia episodes detected by each method were analyzed by a single investigator, who was different for each method.
Furthermore, within the follow-up used in method A, the main demographic characteristics of patients were recorded, including age, sex, reason for admission, comorbidities, immunosuppressive treatment (corticoids persistently used over the previous 3 months or current immunosuppressive therapy in a patient with malignancy), as well as the characteristics of the catheters, including type, date of insertion and removal, anatomic site of insertion, use, placement location, number of lumen, and reason for removal. The patient's local and general infection-related clinical manifestations were also collected.
The following situations prompted catheter removal: completion of treatment, hospital discharge, poor functioning, or suspected infection. Suspicion of infection was based on the presence of one or more of the following criteria: fever of unknown origin, phlebitis, inflammation or pus at the insertion site, clinical signs of sepsis, and/or positive blood culture to a compatible microorganism.
When a patient with a CVC presented fever or a clinical process of sepsis of unknown origin, blood culture was performed, the catheter was removed, and the tip cultured. When a patient had a positive blood culture for a microorganism that commonly causes CRBSI and no other cause was identified, the catheter was also removed and cultured.
Among the cases of catheter removal due to suspected infection, we noted what cultures had been performed: semiquantitative culture of the catheter tip (Maki technque9), culture of any suppuration, and/or blood culture. Catheter tip culture was considered positive when the colony forming unit (cfu) count was greater than 15. As established in the guidelines of the Infectious Diseases Society of America (IDSA), catheters were classified according to clinical and microbiologic criteria as follows: uninfected, when there was no evidence of infection and/or cultures were negative; colonized, when culture was positive, but there was no evidence of infection; and catheter-related bloodstream infection (CRBSI), when catheter culture and blood culture were tested positive for the same microorganism.10–12 In addition, when catheter culture was available in a patient with fever that resolved after catheter removal, there were no other known causes of infection, and blood culture was negative or not performed, the catheter was classified as infected catheter (IC).
Blood cultures were processed using the BactAlert 3D system (Siemens®). Microorganism identification and sensitivity testing were performed with the Microscan WalkAway instrument (Siemens®). When the characteristics of the microorganisms found on blood culture and catheter culture coincided in morphology, biochemical findings, and antibiotype, they were considered to be the same microorganism.
In method A, the incidence density of CRBSI and of overall catheter infection (CRBSI+IC) with 95% confidence intervals was calculated it two ways: in relation to the total number of catheter days and in relation to the total number of hospital days of all patients hospitalized during the study period. In method B, the incidence density of CRBSI was calculated in relation to the total number of hospital days of all patients hospitalized during the same period.
Statistical analysis was performed with the Student t-test for continuous variables and 2×2 contingency tables (chi-square method) for discontinuous variables. A difference was considered statistically significant at p≤0.05. Confidence intervals were compared to evaluate differences between incidence densities.
The study was examined and approved by the Ethics Committee of our institution.
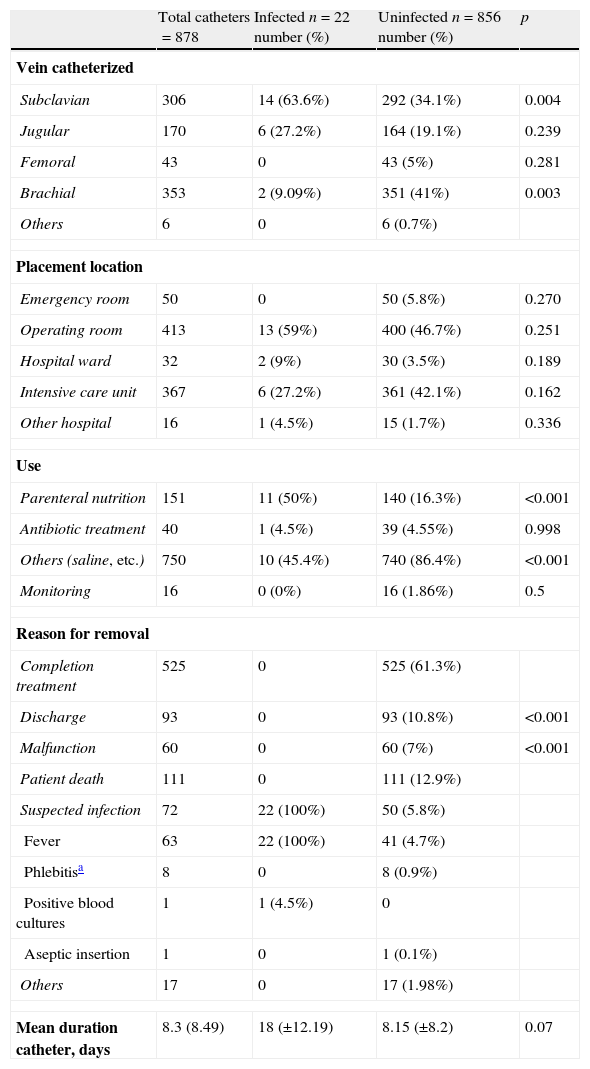
ResultsOver the 12-month study period, 878 catheters were placed in 704 patients (403 men, 57.2%), with a mean age of 65.8 years and a total of 7357 catheter days. More than half the patients (401, 56.9%) were hospitalized for surgery-related reasons. The most relevant comorbid conditions included diabetes mellitus en 148 patients (21.02%), neoplastic disease in 115 (16.33%), and chronic obstructive pulmonary disease (COPD) in 95 (13.49%). Twenty-two episodes of catheter infection occurred in 20 patients. There were no differences in sex, age, or comorbidities between patients with and without catheter infection. The only factor showing significant differences was immunosuppressive treatment, which was more commonly used in patients who developed catheter infection (p=0.013).
The catheter insertion site, the hospital care unit where it was placed, the reason for its use, the reason why it was removed, and the duration of catheterization, are shown in Table 1, which summarizes the differences between infected and uninfected catheters. The mean duration of uninfected catheters was 8.15 days (±8.2 days), and the duration of infected catheters was 18 days (±12.19 days) (p=0.07). Of note, 41 uninfected catheters were removed because of fever, and only 30% of catheters removed for suspected infection were actually infected (22/72).
Catheter-related variables: differences between infected and uninfected catheters.
| Total catheters=878 | Infected n=22 number (%) | Uninfected n=856 number (%) | p | |
| Vein catheterized | ||||
| Subclavian | 306 | 14 (63.6%) | 292 (34.1%) | 0.004 |
| Jugular | 170 | 6 (27.2%) | 164 (19.1%) | 0.239 |
| Femoral | 43 | 0 | 43 (5%) | 0.281 |
| Brachial | 353 | 2 (9.09%) | 351 (41%) | 0.003 |
| Others | 6 | 0 | 6 (0.7%) | |
| Placement location | ||||
| Emergency room | 50 | 0 | 50 (5.8%) | 0.270 |
| Operating room | 413 | 13 (59%) | 400 (46.7%) | 0.251 |
| Hospital ward | 32 | 2 (9%) | 30 (3.5%) | 0.189 |
| Intensive care unit | 367 | 6 (27.2%) | 361 (42.1%) | 0.162 |
| Other hospital | 16 | 1 (4.5%) | 15 (1.7%) | 0.336 |
| Use | ||||
| Parenteral nutrition | 151 | 11 (50%) | 140 (16.3%) | <0.001 |
| Antibiotic treatment | 40 | 1 (4.5%) | 39 (4.55%) | 0.998 |
| Others (saline, etc.) | 750 | 10 (45.4%) | 740 (86.4%) | <0.001 |
| Monitoring | 16 | 0 (0%) | 16 (1.86%) | 0.5 |
| Reason for removal | ||||
| Completion treatment | 525 | 0 | 525 (61.3%) | |
| Discharge | 93 | 0 | 93 (10.8%) | <0.001 |
| Malfunction | 60 | 0 | 60 (7%) | <0.001 |
| Patient death | 111 | 0 | 111 (12.9%) | |
| Suspected infection | 72 | 22 (100%) | 50 (5.8%) | |
| Fever | 63 | 22 (100%) | 41 (4.7%) | |
| Phlebitisa | 8 | 0 | 8 (0.9%) | |
| Positive blood cultures | 1 | 1 (4.5%) | 0 | |
| Aseptic insertion | 1 | 0 | 1 (0.1%) | |
| Others | 17 | 0 | 17 (1.98%) | |
| Mean duration catheter, days | 8.3 (8.49) | 18 (±12.19) | 8.15 (±8.2) | 0.07 |
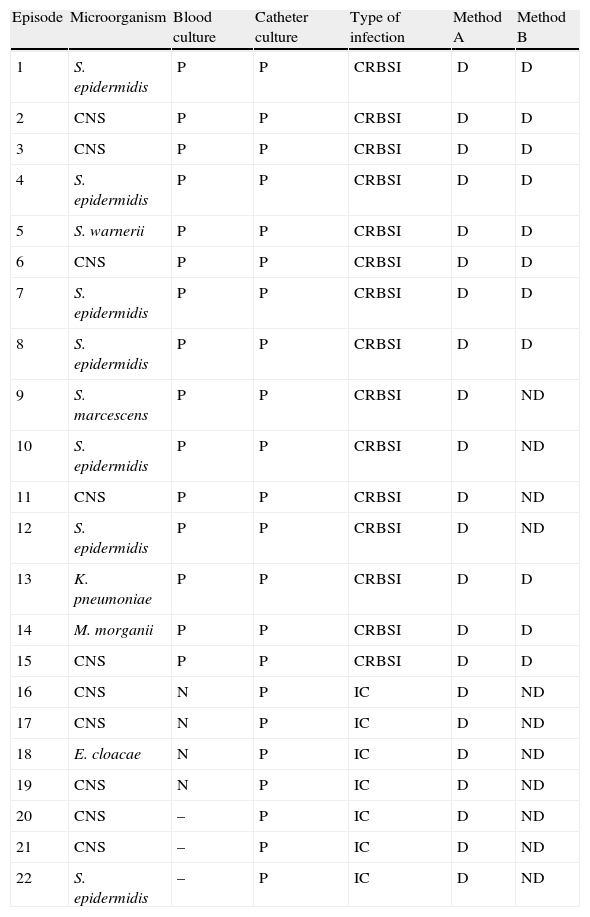
Using prospective daily follow-up (method A), 22 cases of catheter infection were detected, including 15 cases of CRBSI and 7 cases of IC. The most common causal agent was coagulase-negative staphylococcus (Table 2). Using method B, only 11 cases of CRBSI were detected. The details regarding each infection episode and the method by which it was detected are shown in Table 2.
Episodes of catheter-related bloodstream infection, causal microorganism, blood culture, catheter culture, type of infection and results according to detection method.
| Episode | Microorganism | Blood culture | Catheter culture | Type of infection | Method A | Method B |
| 1 | S. epidermidis | P | P | CRBSI | D | D |
| 2 | CNS | P | P | CRBSI | D | D |
| 3 | CNS | P | P | CRBSI | D | D |
| 4 | S. epidermidis | P | P | CRBSI | D | D |
| 5 | S. warnerii | P | P | CRBSI | D | D |
| 6 | CNS | P | P | CRBSI | D | D |
| 7 | S. epidermidis | P | P | CRBSI | D | D |
| 8 | S. epidermidis | P | P | CRBSI | D | D |
| 9 | S. marcescens | P | P | CRBSI | D | ND |
| 10 | S. epidermidis | P | P | CRBSI | D | ND |
| 11 | CNS | P | P | CRBSI | D | ND |
| 12 | S. epidermidis | P | P | CRBSI | D | ND |
| 13 | K. pneumoniae | P | P | CRBSI | D | D |
| 14 | M. morganii | P | P | CRBSI | D | D |
| 15 | CNS | P | P | CRBSI | D | D |
| 16 | CNS | N | P | IC | D | ND |
| 17 | CNS | N | P | IC | D | ND |
| 18 | E. cloacae | N | P | IC | D | ND |
| 19 | CNS | N | P | IC | D | ND |
| 20 | CNS | – | P | IC | D | ND |
| 21 | CNS | – | P | IC | D | ND |
| 22 | S. epidermidis | – | P | IC | D | ND |
Abbreviations. CRBSI: catheter-related bloodstream infection; IC: infected catheter; P: culture positive; N: culture negative; –: not done; D: detected; ND: not detected; CNS: coagulase-negative staphylococcus.
Microorganisms: E. cloacae, Enterobacter cloacae; K. pneumoniae, Klebsiella pneumoniae; M. morganii, Morganella morganii; S. marcescens, Serratia marcescens; S. epidermidis, Staphylococcus epidermidis; S. warnerii, Staphylococcus warnerii.
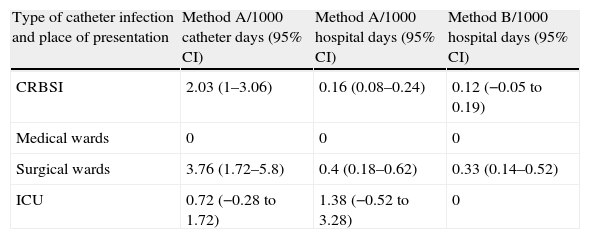
These data yielded an incidence density of catheter infection (IC+CRBSI) of 2.99/1000 catheter days or 0.24/1000 hospital days. Focusing only on CRBSI episodes, the incidence density of CRBSI was 2.03 episodes/1000 catheter days or 0.16 episodes/1000 hospital days using method A, and 0.12 episodes/1000 hospital days using method B. The rates of catheter infection and CRBSI according to the detection method used and the hospital department where infection was acquired are shown in Table 3.
CRBSI rates and 95% confidence intervals according to hospital area of presentation, and detection method used.
| Type of catheter infection and place of presentation | Method A/1000 catheter days (95% CI) | Method A/1000 hospital days (95% CI) | Method B/1000 hospital days (95% CI) |
| CRBSI | 2.03 (1–3.06) | 0.16 (0.08–0.24) | 0.12 (−0.05 to 0.19) |
| Medical wards | 0 | 0 | 0 |
| Surgical wards | 3.76 (1.72–5.8) | 0.4 (0.18–0.62) | 0.33 (0.14–0.52) |
| ICU | 0.72 (−0.28 to 1.72) | 1.38 (−0.52 to 3.28) | 0 |
CRBSI: catheter-related bloodstream infection; ICU: intensive care unit.
The results of this study demonstrate the higher sensitivity of method A than method B for the detection of bloodstream infection in patients with central venous catheters. Prospective daily follow-up of patients using these devices resulted in detection of 27% more episodes of CRBSI than retrospective assessment using microbiology data on positive cultures. Furthermore, prospective follow-up enabled detection of infected catheters in patients without bloodstream infection, and analysis of the risk of such infections in relation to the days of catheterization.
Knowledge of the CRBSI rate in a particular center is the first step required when planning preventive strategies.13 The IDSA guidelines recommend determination of CRBSI rates according to days of catheterization, and comparison of these rates with historical data from each institution and hospital department, as well as with national rates.13 Incidence studies are more accurate and reliable than prevalence ones, although they are labor-intensive and costly, which makes them less reproducible. Furthermore, a prospective, observational study has greater capacity to detect the phenomena being investigated than a retrospective analysis based on incomplete results.
We know that catheter infection manifests within a wide spectrum of severity, from infection without microbiological documentation that can be resolved by simple catheter removal to severe infection that may require surgery for cure. Thus, for effective management and prevention of catheter infection, daily monitoring of related signs and symptoms on an individual basis with correct identification of the type of infection detected is necessary.11 Using method A, we were able to gather data on risk factors for infection that could not be obtained with method B, in which information was lacking on catheters that did not cause bloodstream infection. Hence, prospective monitoring of these patients will undoubtedly lead to better prevention policies.
In the present study, there were no cases of catheter-associated bloodstream infection; that is, episodes in which the catheter is not removed and the diagnosis is performed by evaluating bacterial growth in paired blood cultures.14 It is useful to maintain the catheter when it is needed for long-term treatment such as in dialysis and oncologic patients. This situation is not encountered in our basic general hospital, which does not have a dialysis unit or transplant patients.
To perform comparisons among hospitals, patient types, catheter types, etc., and thereby, to establish standards regarding CRBSI, we believe the best and most realistic method is to determine the number of infections in relation to the true risk of acquiring these infections, that is, based on the number of catheter days. Determination of CRBSI rates according to the total of days hospitalized in a center implies bias because certain factors are not taken into account (e.g., number of patients who are not catheterized) and this fact could underestimate the effect that a low catheterization rate would have on calculation of the incidence of bloodstream infection. The data obtained in this study support the idea that calculating CRBSI rates in relation to the days of risk provides better estimation of the true incidence.
Recently, Maki et al. reported a series of standards for CRBSI that can be used as a reference to determine whether observed hospital rates are excessive or not. For central venous catheters, a rate of 2.7 CRBSI episodes/1000 catheter days was considered acceptable.15 This rate is not greatly different from the overall rate observed in our institution (2.03 episodes/1000 catheter days), but lower rates were seen in some of our care units. The low CRBSI rate in our intensive care unit (0.72 episodes/1000 catheter days) provides evidence that the general measures for CRBSI prevention are being carried out correctly, even the controversial use of disinfectable, needle-free mechanical valve connectors.8,16,17 In the ENVIN-UCI study,18 for example, which was focused on CRBSI prevention in the ICU, the reported incidence was 2.48 episodes per 1000 catheter days. Although the situation in ICUs has received the greatest attention in the last 20 years, a considerable number of patients using CVCs are hospitalized in other care units, where there is also a clear risk of acquiring CRBSI. Our results support this notion: There was a higher risk CRBSI in hospital wards, particularly surgical units, than in the ICU, where a specialized nursing team develops active strategies for surveillance and control of these infections. Thus, our findings indicate that it is imperative to implement educational and training programs on CRBSI prevention for health personnel working in conventional care areas.
One factor that was not investigated in this study is the cost and time required for the staff to carry out prospective catheter monitoring. Although it was not an objective of the study, we estimated a daily time expenditure of 2 working hours, which is acceptable in a hospital similar to ours in size and characteristics.
Several limitations of our study should be noted. Some patients with fever did not undergo blood sampling and culture, and some catheters that were removed because of suspected infection were not cultured. Hence, the estimated incidence of CRBSI may have underestimated the true incidence and favored lower detection by method B. This occurred with 4 CRBSI cases detected by method A that were not recorded by B: in all cases catheter tip culture and blood culture were performed separately in time, in a range over 48h. It should also be mentioned that the reason for catheter removal in all patients without associated bacteremia was because of fever; hence, it is possible that some of these cases may have been undiagnosed episodes of CRBSI. Lastly, the study did not include peripheral catheters, whose control by method A would be highly laborious, considering the elevated number of devices implicated.
In conclusion, the practice of prospective monitoring of all CVCs placed during hospitalization has yielded accurate data on the true risk of these infections in our setting. This information is the necessary basis for developing pertinent corrective measures that will enable better management of these devices with regard to prevention, diagnosis, and treatment of related infections.
Conflicts of interestNone of the authors have any conflict of interest to declare.
We thank Ms. Elisabeth Palomera (Research Unit of the Consortium sanitari Maresme) for their help in the statistical study, and Celine Cavallo for his translation into English of the Spanish text.