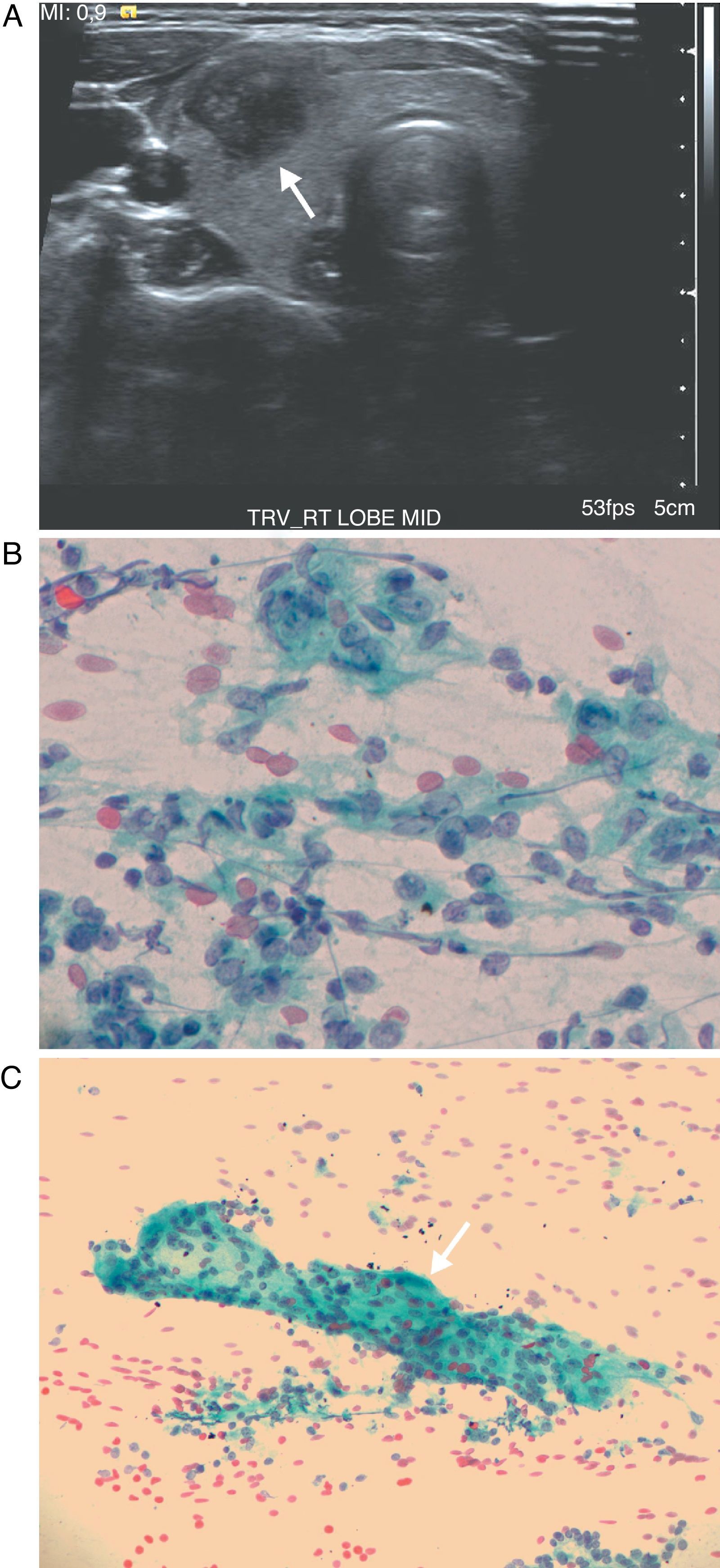
We recently encountered two very similar patients with atypical de Quervain's (also known as giant cell, granulomatous, or subacute) thyroiditis presenting as solitary painless thyroid nodules suspicious for papillary thyroid cancer. Patient 1 was an otherwise healthy 34-year-old female who presented with a painless right thyroid nodule. Initial thyroid functional test results were normal. Thyroid ultrasound identified a 2.2-cm, hypoechoic right thyroid nodule with ill-defined margins and microcalcifications (Fig. 1). The radiological report commented that the nodule was “highly suspicious for papillary thyroid cancer” and recommended fine needle aspiration (FNA). At the endocrine clinic, she appeared to be clinically euthyroid and physical examination confirmed an irregular, firm, 2-cm nodule in the right thyroid without tenderness or cervical lymphadenopathy. Adjusted total thyroxine levels were normal at 4.7μg/dL (normal 1.8–5.0), TSH undetectable (normal 0.39–4.60μU/mL), erythrocyte sedimentation rate 49, and thyroperoxidase antibody negative. During an ultrasound-guided FNA with a 25-gauge needle, the nodule was very hard and difficult to penetrate; insufficient number of cells were obtained. Repeat biopsy with a 27-gauge needle resulted in sufficient number of cells and cytology report described “clusters of atypical follicular epithelial cells with nuclear enlargement, overlap, elongated, ovoid nuclei and open chromatin pattern” which were “suspicious for papillary thyroid carcinoma.” The presence of ill-formed granuloma was not apparent to the cytopathologist then. The patient was diagnosed with papillary thyroid carcinoma and total thyroidectomy planned. At the operating table, the right thyroid appeared red-brownish in color, firm, and nodular, and loosely attached to the strap muscles. The surgeon suspected thyroiditis which was supported by frozen section and thus only performed right thyroidectomy. Surgical pathology confirmed de Quervain's thyroiditis.
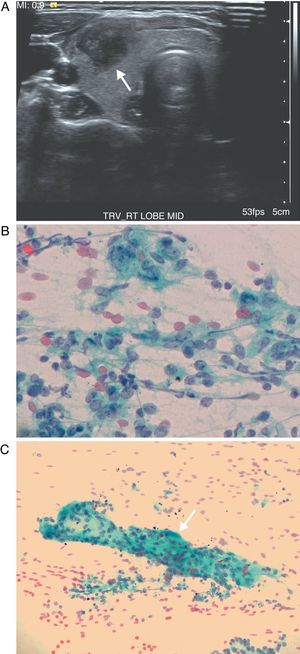
(A) Patient 1: right thyroid nodule on ultrasound. See text for details. (B and C) Patient 2: left thyroid nodule cytology. (B) Histiocytes (blue) with features mimicking atypical follicular cells seen in papillary thyroid carcinoma: slightly enlarged and overlapping nuclei, nuclear elongation, irregular nuclear membrane, open chromatin, and small and peripherally located nucleoli (Papanicolaou stain, 60×). (C) A multinucleated giant cell (arrow, 20×).
Patient 2 was also an otherwise healthy female, 38-year old, who presented with a sore throat and a left thyroid mass which was confirmed by ultrasound. Her TSH levels were 0.02, free thyroxine 2.5ng/dL (normal 0.8–1.9), and thyroperoxidase antibody negative. At the endocrine clinic, she complained of nervousness and difficulty to concentrate but her neck pain had stopped spontaneously. She was afebrile with normal heart rate. A firm, irregular, non-tender left thyroid nodule was palpated. Erythrocyte sedimentation rate was 22. Thyroid ultrasound showed a hypoechoic left thyroid nodule measuring 4.2cm×1.3cm×1.1cm, with ill-defined margins and microcalcifications. A 27-gauge needle had to be used during ultrasound-guided FNA as the lesion was very hard to penetrate. The cytology features were almost identical to those of patient 1, but the presence of well-formed granuloma and the reorganization of background histiocytes were also seen (Fig. 1). After discussion between the endocrinologist and the cytopathologist, de Quervain's thyroiditis was diagnosed and the patient was treated with propranolol with clinical improvement and resolution of the “thyroid nodule” which was confirmed by thyroid ultrasound.
Thyroid ultrasound and ultrasound-guided FNA have improved the diagnosis of thyroid nodules. The ultrasound findings and cytology features have to be interpreted in the specific clinical context. de Quervain's thyroiditis (clinically referred to as subacute thyroiditis) typically presents with painful thyroid and hyperthyroidism, but in rare cases, it can present with painless thyroid nodules.1,2 As de Quervain's thyroiditis is usually diagnosed clinically without the use of ultrasound or cytology, endocrinologists, radiologists and cytopathologists are often not familiar with its ultrasound findings or cytological features. On ultrasound, multifocal, and rarely, unifocal hypoechoic area(s) with irregular margins are seen in de Quervain's thyroiditis which can be interpreted as thyroid nodules.3 The histiocytes in de Quervain's thyroiditis mimic atypical follicular cells on cytology, and the diagnostic giant cells are only present in 10% of cases.4,5 In both of our cases, solitary, painless, and non-tender “thyroid nodules” and “suspicious” ultrasound features prompted FNA which further revealed “suspicious” cytological features, resulting in unnecessary hemithyroidectomy in 1 patient. Communication between the endocrinologist and the cytopathologist resolved the diagnostic uncertainty in the other patient. In retrospect, the suppressed TSH suggested functional nodules or thyroiditis and radioiodine uptake and scan could have helped reaching the correct diagnosis. Should FNA be done, the very hard consistency of the nodule and the unique cytology features may suggest de Quervain's thyroiditis and the communication between the clinician and the cytopathologist is critical to resolve the diagnosis. We thus conclude that atypical de Quervain's thyroiditis should be considered in the differential diagnosis of thyroid nodules. On the other hand, approximately 0.5% of patients with de Quervain's thyroiditis have true papillary thyroid carcinoma so that ultrasound follow-up is needed in those patients with suspicious hypoechoic areas; FNA is indicated in those with persistent hypoechoic areas larger than 1cm.6