Knowledge and the development of skills in airway management is one of the core competencies in the training of the anesthesiologist. “Know how” and “Knowing to do well and fast” are decisive under certain critical situations that may arise in the management of anesthesia. Bronchoscopy is a useful diagnostic and therapeutic procedure. Knowledge of the technique and airway anatomy is the cornerstone of bronchoscopy; however, there are anatomical variations and different airway classifications.
ObjectiveTo describe the airway anatomy by means of schematic representations, to assess anatomical variations and to learn about the characteristics of the procedure.
MethodologyA non-systematic review of databases (PUBMED/MEDLINE, Science Direct, OVID, SciElo) was undertaken using the following.
Results and conclusionsBronchoscopy is a useful surgical and diagnostic procedure for different applications. The anatomical variations of the airway are only present in a small percentage of the population. Anatomical classifications are both anatomically and numerically diverse; however, what is really relevant is to develop a spatial relationship. Bronchoscopy is a technique that evolves simultaneously with other technical biomedical breakthroughs and is a procedure that the anesthesiologist must explore further in order to accomplish better outcomes in anesthesia.
El conocimiento y desarrollo de habilidades en el manejo de la vía aérea es una de las competencias importantes en la formación del anestesiólogo; el “saber” y el “saber hacer bien y rápido” son determinantes en algunas situaciones críticas a las que se puede enfrentar durante el manejo anestésico. La broncoscopia es un procedimiento útiltanto diagnóstico como terapéutico. El conocimiento de la técnica y de la anatomía de la vía aérea constituye el pilar de la broncoscopia, encontrando diferentes variaciones anatómicas y clasificaciones de la vía aérea.
ObjetivoDescribir la anatomía de la vía aérea a través de esquemas, evaluar variaciones anatómicas y conocer características propias del procedimiento.
MetodologíaCon las palabras clave “Bronchoscopy”, “Anatomy”, “Airway” y “Anesthesia” se realizó una revisión no sistemática en bases de datos (PUBMED/MEDLINE, Science Direct, OVID, SciElo).
Resultados y conclusionesLa broncoscopia es un procedimiento útil en el plano quirúrgico y diagnóstico, siendo utilizado en distintos procedimientos. Las variaciones anatómicas de la vía aérea se presentan en un porcentaje pequeño de la población. Las clasificaciones anatómicas son diversas tanto anatómica como numéricamente; sin embargo, lo relevante es desarrollar una relación espacial. La broncoscopia es una técnica que va en desarrollo paralelo a otros avances de la tecnología biomédica, es un procedimiento del cual el anestesiólogo debe investigar más con el fin de generar mejores efectos en el campo de la anestesiología.
Bronchoscopy is a diagnostic and therapeutic procedure to visualize the airway and its pathological alterations. In the last few decades bronchoscopy has enabled complementary procedures such as biopsies that have been adopted into management protocols for specific groups of patients. Advances in this area have been led by pulmonologists, but fortunately this knowledge has been disseminated and is now part of the training of other specialties like anesthesiology and intensive care,1,2 resulting in a valuable contribution to diagnostic and therapeutic procedures. Several training programs for residents have been forced to include bronchoscopy training into their syllabus as a must-have skill. Currently, fibro-bronchoscopy in anesthesia is key for difficult airway management algorithms, as well as for pulmonary support techniques endorsed by different publications.
MethodologyNon-systematic literature review both in English and Spanish, with no time restrictions, using PUBMED/MEDLINE, Science Direct, OVID and SciElo databases, complemented with articles referenced in the above search. The following words were used in English: Bronchoscopy, Anatomy, Airway, and Anesthesia, while in Spanish the terms used were: Broncoscopia, anatomía, vía aérea and anestesia. Both the search and the selection of articles were done independently, with no restrictions as to the type of publication.
Characteristics of the procedure and anesthesia considerationsKnowledge of the upper and lower airway structures, including any anatomical alterations, is critical for a sound diagnostic or therapeutic practice. Particularly when pulmonary insulation is required, proper positioning of the device has to be ensured; otherwise, the surgeon may be challenged with hypoxemia, mechanical complications and surgical technique difficulties.3,4
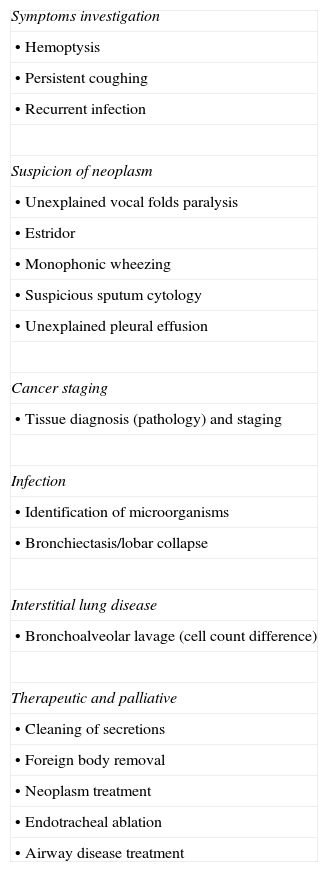
Bronchoscopy is useful as part of the training in these disciplines and is indicated under different situations (Table 1).
Indications for flexible bronchoscopy.
| Symptoms investigation |
| • Hemoptysis |
| • Persistent coughing |
| • Recurrent infection |
| Suspicion of neoplasm |
| • Unexplained vocal folds paralysis |
| • Estridor |
| • Monophonic wheezing |
| • Suspicious sputum cytology |
| • Unexplained pleural effusion |
| Cancer staging |
| • Tissue diagnosis (pathology) and staging |
| Infection |
| • Identification of microorganisms |
| • Bronchiectasis/lobar collapse |
| Interstitial lung disease |
| • Bronchoalveolar lavage (cell count difference) |
| Therapeutic and palliative |
| • Cleaning of secretions |
| • Foreign body removal |
| • Neoplasm treatment |
| • Endotracheal ablation |
| • Airway disease treatment |
In order to undertake bronchoscopy procedures, a complete work team and instrumentation are needed, including as a minimum monitoring devices and crash cart with all the pharmacological tools. The bronchoscope must be carefully operated to prevent breakage of the optical fiber. The recommendation is to lubricate with distilled water and avoid using any gels.
Bronchoscopy may be done orally or nasally5; however, the decision to use a nasal approach depends on the associated comorbidities and any potential structural alterations the patient may have. It is critical to identify upper airway hemoptysis to determine the right approach. Several work groups are still debating about the need to administer sedation prior to the procedure.6,7 The purpose of sedation is to provide patient comfort and to facilitate the job of the bronchoscopist.8–10 However, a bronchoscopy procedure may be done without sedation.11,12 However, according to some publications, most bronchoscopies are performed under sedation.13–16 Indeed, bronchoscopy is a procedure that causes discomfort in most patients.
Basic on-going monitoring is recommended for any anesthetic procedure including sedation. There is no ideal formula to sedate a patient and sedation regimes should be tailored to the individual patient, his/her comorbidities and the specific type of procedure. Various pharmacological options or combinations of anesthetic agents have been described. One of them is the combination of a short-acting benzodiazepine such as midazolam with opiates.17,18
Nerve blocks are seldom performed, unless the anesthesiologist feels it is appropriate. These blocks use local anesthetics such as lidocaine spray, preferably at 2–4% concentrations.19,20 Atropine or glycopyrrolate may be administered prior to the procedure in order to reduce the amount of secretions and to mitigate vagal hyperactivity.21,22
Recent advances in various cardiac, thoracic and GI tract surgical techniques have led to the widespread practice of double lumen intubation and the use of the fiber bronchoscope in the OR.23–25 Regardless of the route it is convenient to always follow the same approach and to return to an identifiable structure to avoid confusion.
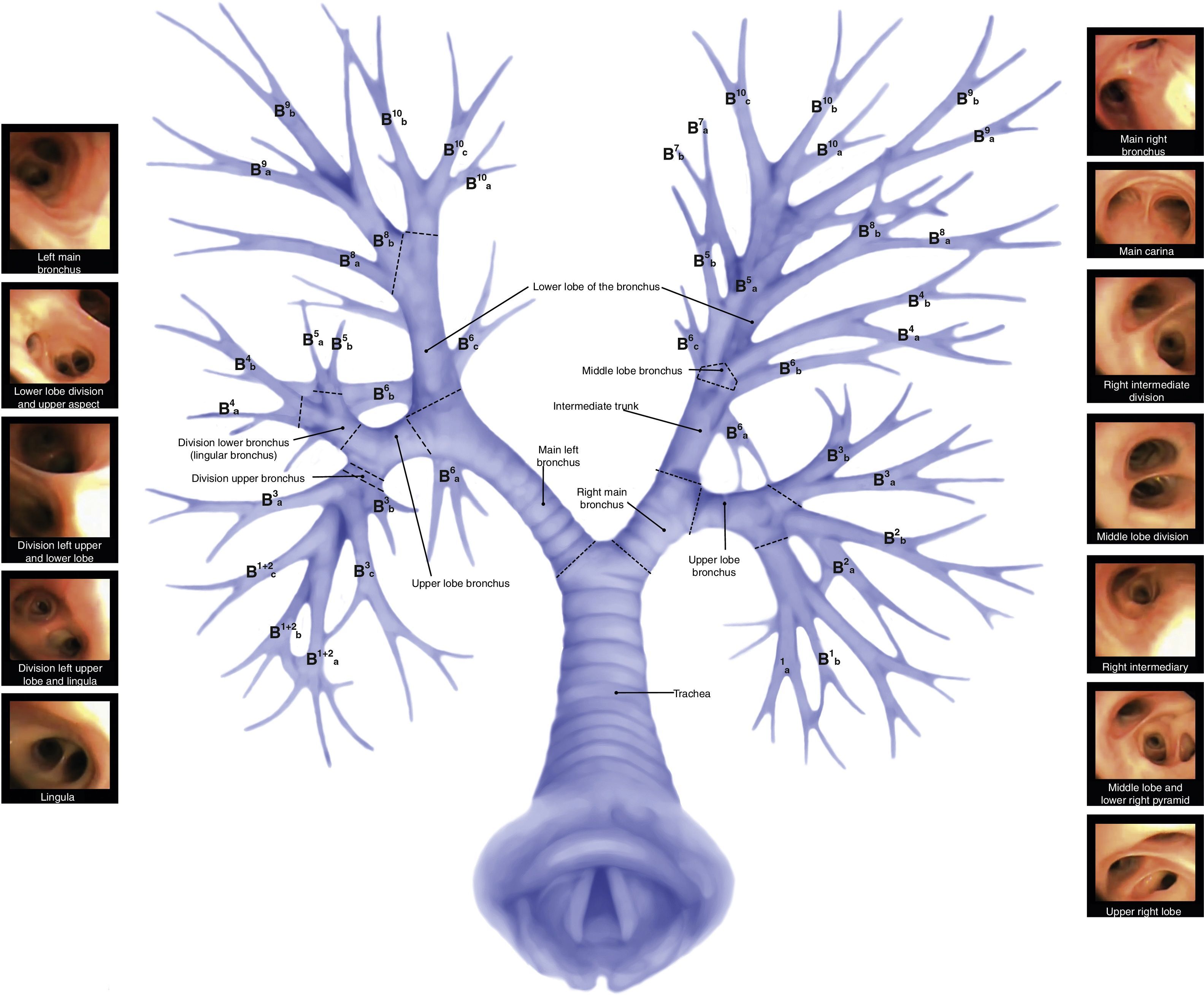
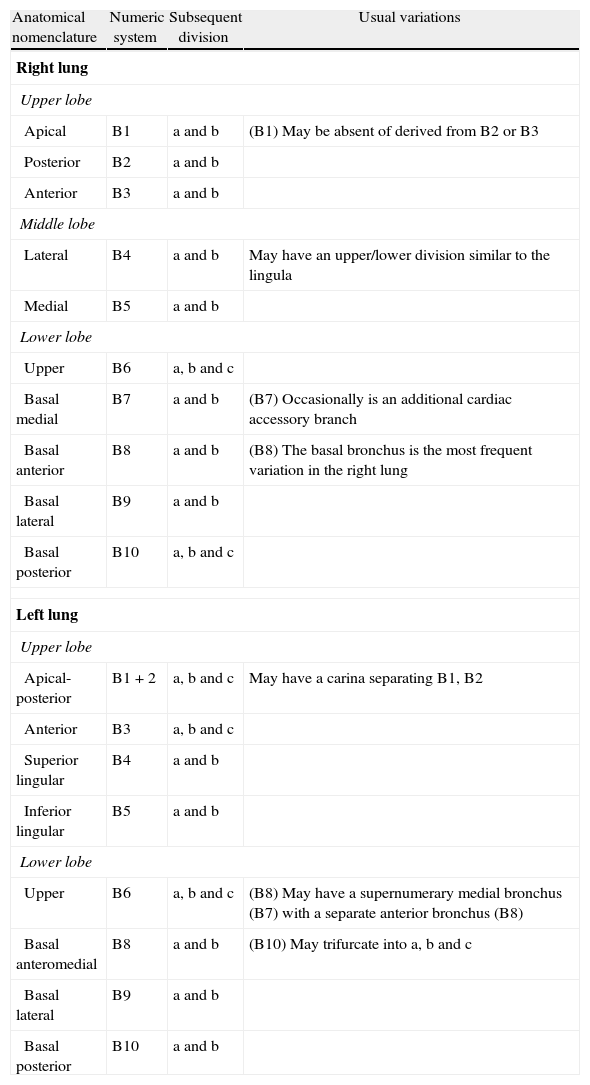
Airway anatomy and anatomical variationsTwo types of recognizable nomenclatures are used to classify the airway. The most common one being the Jackson–Huber classification that describes and names the divisions in accordance with the anatomic space orientation.26 The other popular classification is Boyden's27 for surgical purposes; this classification numerically divides each zone. Another less popular is the Yamashita Japanese classification.28 The recommendation is to use the Jackson–Huber classification because it is most widely used and less complex (Table 2).
Nomenclature and anatomical variations.
| Anatomical nomenclature | Numeric system | Subsequent division | Usual variations |
| Right lung | |||
| Upper lobe | |||
| Apical | B1 | a and b | (B1) May be absent of derived from B2 or B3 |
| Posterior | B2 | a and b | |
| Anterior | B3 | a and b | |
| Middle lobe | |||
| Lateral | B4 | a and b | May have an upper/lower division similar to the lingula |
| Medial | B5 | a and b | |
| Lower lobe | |||
| Upper | B6 | a, b and c | |
| Basal medial | B7 | a and b | (B7) Occasionally is an additional cardiac accessory branch |
| Basal anterior | B8 | a and b | (B8) The basal bronchus is the most frequent variation in the right lung |
| Basal lateral | B9 | a and b | |
| Basal posterior | B10 | a, b and c | |
| Left lung | |||
| Upper lobe | |||
| Apical-posterior | B1+2 | a, b and c | May have a carina separating B1, B2 |
| Anterior | B3 | a, b and c | |
| Superior lingular | B4 | a and b | |
| Inferior lingular | B5 | a and b | |
| Lower lobe | |||
| Upper | B6 | a, b and c | (B8) May have a supernumerary medial bronchus (B7) with a separate anterior bronchus (B8) |
| Basal anteromedial | B8 | a and b | (B10) May trifurcate into a, b and c |
| Basal lateral | B9 | a and b | |
| Basal posterior | B10 | a and b | |
A number of general anatomic concepts of the airway are important to remember. The upper airway includes the mouth, the nose, the nasopharynx, the oropharynx, the laryngopharynx and the larynx. All of them are extremely critical in the management of the airway.
The mouth is mainly made up of the tongue and the teeth, which are relevant structures o consider for intubation. The surrounding structures of the mouth are the lips (anterior), the hard and soft palate (upper), the floor of the tongue (lower) and the oropharynx (posterior). The tongue is critical for the establishment of a patent airway.
The surrounding structures of the nose are the nostrils (anterior), the nasopharynx (posterior) and they are separated from the oral cavity by the palate. The nasal cavity has three turbinates dividing the space into meatus through which air flows to allow for a decrease in turbulent flow, humidifying and warming-up to limit the injury inflicted to the lower airway.29–31 Such approach is seldom used for intubation and accessory procedures due to internal injuries, skull base fractures or any other pathologic process that hinders the passage through this pathway. The lower turbinate and its corresponding meatus are the most important ones since this space allows for a patent airway. The sphenopalatine branch of the maxillary and facial arteries supplies irrigation both give rise to Kiesselbach's plexus, an area of frequent bleeding.
The pharynx is divided into three structures: the nasopharynx, the oropharynx and the laryngopharynx.32 Going through the nasal cavity you find the lower turbinate laterally and the nasal septum medially. When the bronchoscopist examines the nasal cavity the integrity of the mucosa may be assessed, together with potential septal deviations, turbinate hypertrophy or nasal polyposis.
When introducing the bronchoscope through the oropharynx, it is critical to identify structures such as the tonsils, the palate and the base of the tongue.33–35 Further down you find the laryngopharynx with 3 important identifiable structures: the piriform recess, the post-cricoid region and the posterior wall of the pharynx. The space between the base of the tongue and the anterior margin of the epiglottis36,37 is relevant when trying to locate a foreign body.
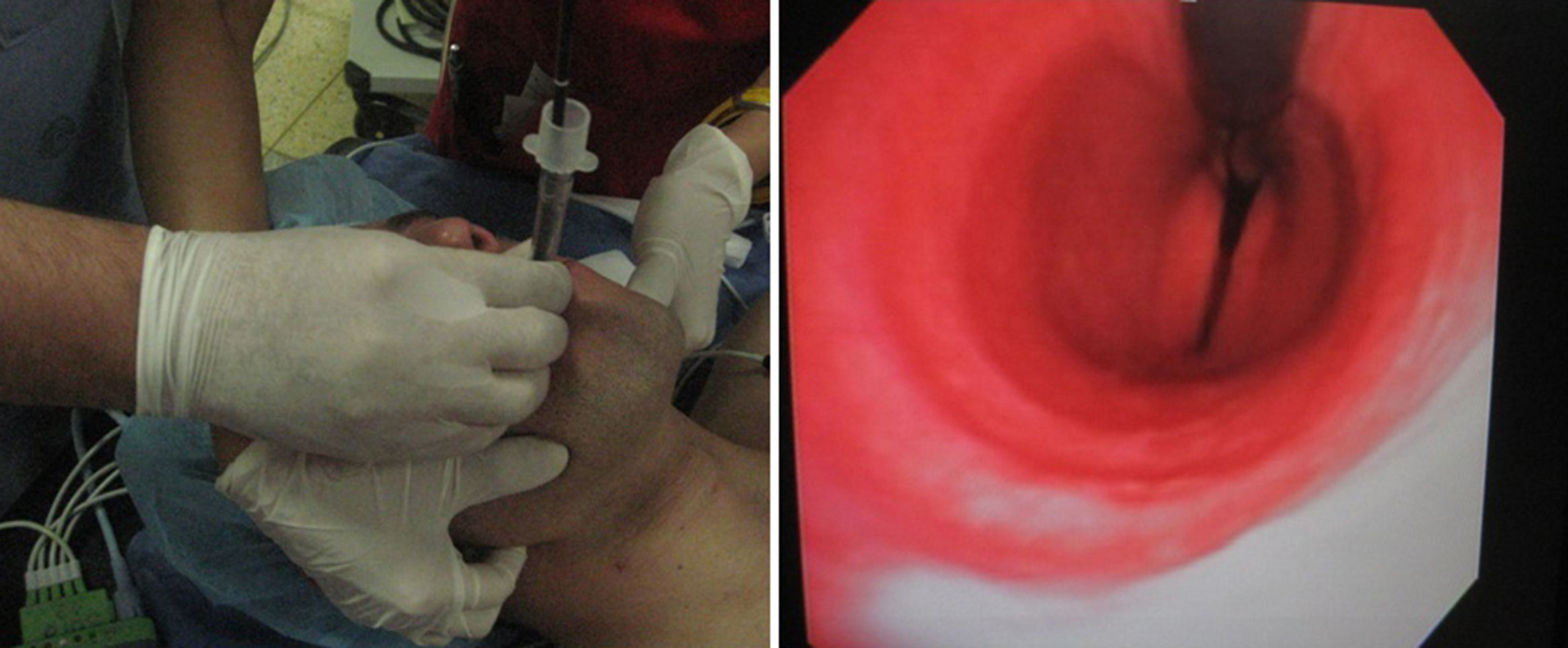
The larynx is the communicating structure between the upper and lower airway organs.38,39 The vocal folds should be briefly examined in abduction and adduction (Fig. 1). La Vocal fold dysfunction may be functional or organic. The upper laryngeal nerve and the recurrent laryngeal nerve innervate the vocal folds. Topical anesthesia helps to pass the instruments through the cavity.
Lower airwayThe trachea is the initial segment of the lower airway and starts at the level of C6.40 It is a cartilaginous tube that extends from the cricoid cartilage to the carina.41 During expiration, the trachea rises up to C4 while in total inspiration it reaches C6. The length of the trachea varies according to age. In neonates it is 3cm, in the pediatric population the range is 7–10cm42 and in adults it is approximately 15cm. The diameter is 6mm, 10mm and 13–22mm respectively. The length of the upper airway does not change with age but the height does. So a 10cm decrease in height represents a 1cm change in the length of the upper airway considering an average height of 1.70m (29cm).43 In adults, the upper airway comprises 16–20 C-shaped cartilages; the anterolateral wall is united by a tracheal membrane with no cartilage and is supported by the tracheal muscle that allows for extension in response large airflows (Ex. Asthma, COPD).44–47 The above diameters vary in accordance with the gender of the patient, as shown by studies of the average diameter, the coronal diameter and the sagittal diameter. The average in men is 22, 13–25, 13–17mm, respectively, somewhat larger as compared to women: 19, 10–21, 10–23mm.48 The average tracheal wall thickness is 3mm. The trachea is localized in the mid-line, occasionally displaced to the right because of the position of the aortic arch and in elderly patients with morbidities such as COPD that may result in a narrower antero-posterior diameter with subsequent physiological consequences. It is important to examine the integrity of the tracheal mucosa to identify any endotracheal lesions, observe probable deviations caused by masses, the distal trachea at the junction with the carina, since these are potential metastatic areas. In case any lesions are found, both lungs must be examined prior to doing a biopsy. If bleeding is present, the evaluation becomes more difficult because the quality of the fiber-bronchoscopy is compromised, in addition a longer time to complete the procedure.
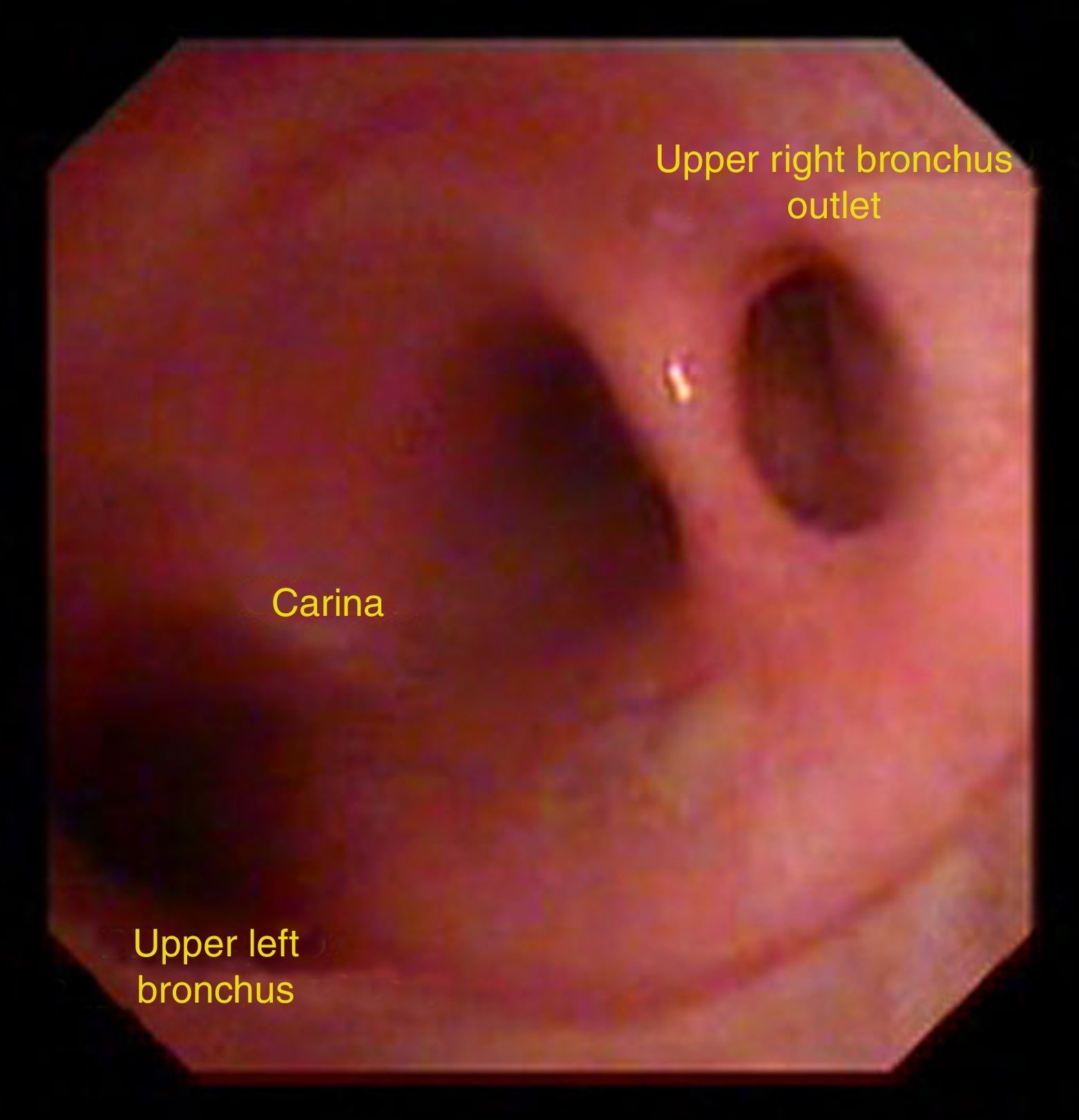
The trachea bifurcates at the level of the carina into the right and left main bronchi; as the trachea advances the lumen decreases progressively. The bifurcation is localized at the level of T5. The right bronchus is more vertically placed at a 90° angle or less with the trachea, while the left bronchus is more horizontal. In children the carina is usually more displaced to the right and with time it becomes more medial and the angulation tends to be more obtuse.
2cm and 1.5cm along the length of the right bronchus the right upper bronchus becomes the intermediate bronchus. One out of 300 people have anatomical variants and the upper right lobe emerges on top of the carina (Fig. 2). Some studies report a prevalence of 0.1–2% for the upper right lobe and 0.3–1% for the upper left lobe.49 In some cases you may find a bridge bronchus arising from the left bronchus but ventilates the lower right lobe. A normal variant is any variant that does not obstruct the airflow but this finding is usually incidental. The diameter of this bronchus is 17.5mm in males and 14mm in females. This bronchus divides into apical (B1), anterior (B2) and posterior (B3). The anterior and posterior segments are the most frequent sites for bronchial disease, including carcinomas. The apical is divided into posterior (B1a) and anterior (B1b). The anterior is divided into anterior (B2b) and posterior (B2a), the posterior into anterior (B3b) and posterior (B3a). The above description is based on Boyden's classification but some bronchoscopists use the Japanese Yamashita classification, wherein B2 and B3 are inverted into posterior and anterior, respectively. After generating the right upper lobe bronchus, the right bronchus lobe becomes the intermediate bronchus that extends for approximately 2–2.5cm and then splits into the middle lobe bronchus and the lower lobe bronchus. The middle lobe bronchus emerges anterolateral with a 1–2cm length before it divides into lateral (B4) that is visualized at a long distance and medial (B5), that is visualized more oblique. Both the lateral and the medial divide into anterior and posterior (B4b), (B4a), (B5b) and (B5a). The intermediate bronchus has an oblique shape and runs posterior to the right pulmonary artery and inferior to the right interlobar artery. A cardiac bronchus is a rare congenital anomaly of the intermediate bronchus where the bronchus originates in this segment before giving origin to the lower lobe bronchus that advances into the pericardium. The lower lobe bronchus is divided into upper (B6), medial basal (B7), anterior basal (B8), lateral basal (B9) and posterior (B10).
With regard to the left lung, it is important to highlight that the division of the bronchi is usually similar if compared to the right lung; however, the left lung may have 8–10 bronchi. The left source bronchus is more horizontal than the right and tends to go more toward posterior and lateral. The left bronchus is divided into the left upper lobe bronchus and the left lower lobe bronchus. The former (first ramification) is at 5 and 4.5cm from the carina in males and females, respectively (the distance from the carina to the bifurcation between the upper and lower left lobe is in average 6–8cm in males and 5–6cm in females).50 The upper left bronchus lobe is divided into the upper division bronchus and the lingular bronchus. The upper division bronchus is divided into apical-posterior (B1/B2) and anterior bronchus (B3) and advances anteriorly accompanied by the anterior segmental artery. The apical–posterior bronchus may be presented in block or divided into the apical and the posterior segment (B1 and B2). The lingular bronchus is slightly inferior–lateral 2–3cm long and divided into upper (B4) and lower (B5). The left bronchus of the lower lobe is divided into upper (B6), anteromedial (B8), lateral basal (B9), and posterior basal (B10). The medial basal segment (B7) may be present in one-third of the population and falls off leaving behind an anterior (B8) and medial (B7) bronchus.
ConclusionsThe anatomy of the upper airway is extremely important for a sound bronchoscopy technique (Fig. 3). There are different anatomical variants you should identify and these are common in a certain proportion of the world population. It is important to know the anatomical variations that result in useful physiological differences in practice. Science is constantly evolving, so physicians are required to adopt a culture of on-going education, in addition to the implementation of policies related to patient safety and quality of care.
FundingNone.
Conflict of interestThe authors declare no conflict of interest.
Dr. Gloria Gutiérrez, Javier Fabricio Guillen Olaya and Johani Pedraza Torres.
Please cite this article as: García Araque HF, Valencia Orgaz O, López Vicente R, Gutiérrez Vidal SE. Anatomía de la vía aérea para el broncoscopista. Una aproximación a la anestesia. Rev Colomb Anestesiol. 2014;42:192–198.