Intestinal malrotation occurs as a result of an embryologic alteration during the rotation of the midgut around the axis of the superior mesenteric artery. The incidence of this condition in adult populations is estimated at 0.2%.1 The clinical spectrum of intestinal malrotation, however, is very extensive and non-specific.
We present the case of intestinal malrotation in an adult with anatomical characteristics that have not been previously described in the literature.
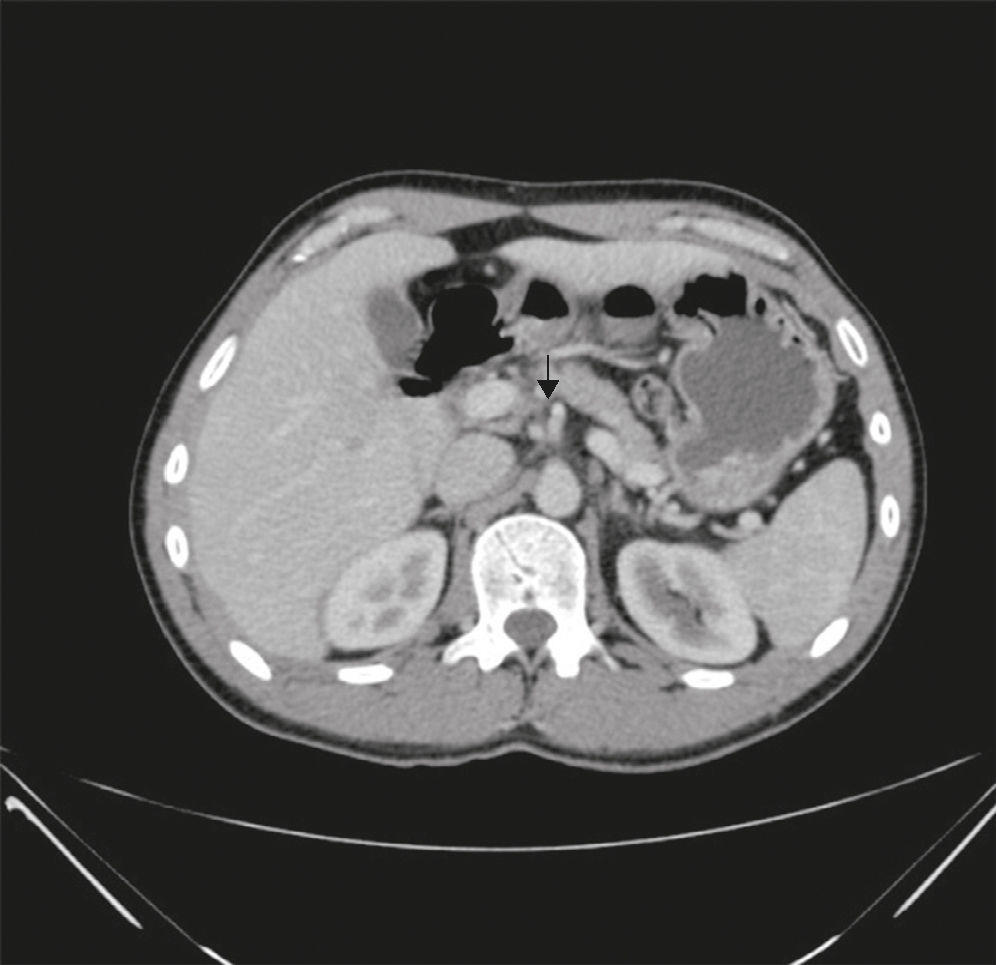
The patient is a 43-year-old male who was referred to our department due to chronic abdominal pain accompanied by recurring episodes of nausea and postprandial vomiting. He had no family or personal medical history of interest, except for dyslipidaemia that was being treated with simvastatin. Physical examination as well as an abdominal and rectal exploration were normal. Routine laboratory tests showed no alterations. Studies were also done to rule out sideroblastic anaemia and altered thyroid function, which were negative. CA 19.9 was not elevated, nor were IgA antibody or other autoimmune antibodies. After upper gastrointestinal endoscopy that showed no relevant lesions, we decided to order a gastrointestinal (GI) series and found dilatation of the second and third portions of the duodenum accompanied by a possible volvulus at the duodenum-first jejunal loop (Fig. 1), and the caecum was located high and central. Afterwards, abdominal computed tomography was conducted to complete the study, which revealed a dilated duodenum situated to the right of the vertebral axis, superior mesenteric vein situated in front and to the left of the superior mesenteric artery, and a “whirlpool sign” of the vein and mesentery around the artery (Fig. 2).
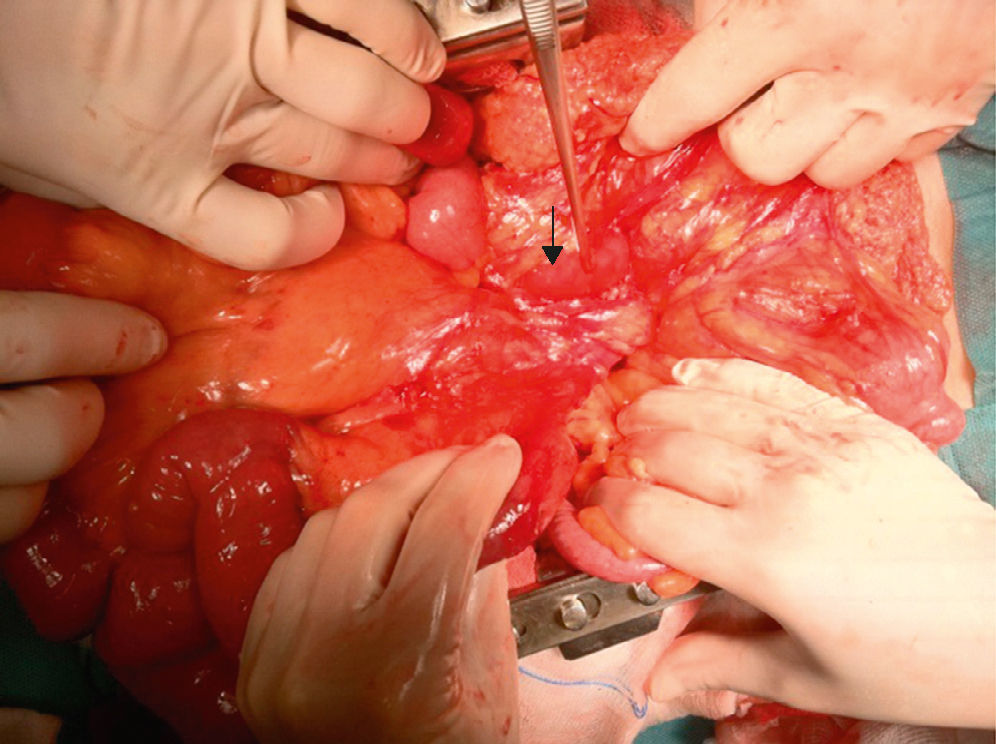
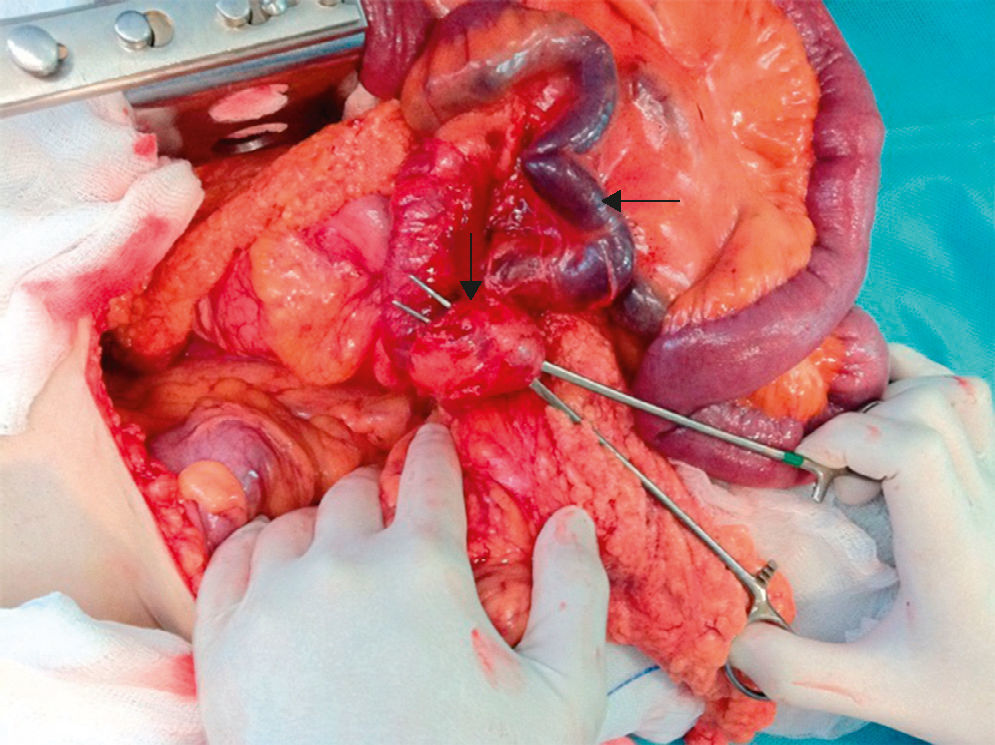
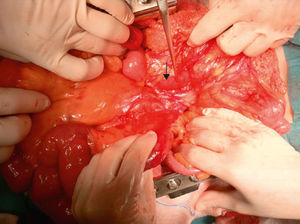
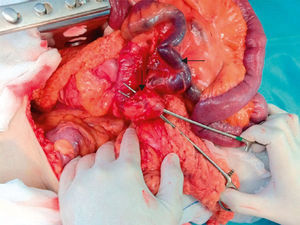
The patient was scheduled for exploratory laparotomy, which showed evidence of volvulus of the entire colon clockwise around the mesenteric axis, due to the retrovascular passage of the first jejunal loop (Fig. 3). The caecum and the appendix were situated at the right side of the theoretical angle of Treitz and held by a band (Fig. 4). We also observed 2 varices measuring approximately 1.5cm in diameter that ran along the entire mesenteric edge of the terminal ileum (Fig. 4). Adhesiolysis was performed until the theoretical angle of Treitz was located, and the band that held it to the terminal ileum-caecum was divided; an appendectomy was performed as well as anatomic fixation of the right colon to the paracolic gutter. Finally, the first intestinal loop was positioned in front of the vessels with a side-to-side suture.
In the postoperative period, the patient's condition progressed favourably, and he was discharged on the sixth day post-op with adequate intestinal transit and no abdominal pain. Currently, the patient is asymptomatic.
The term intestinal malrotation is defined as anomalous rotation and fixation of the primitive midgut. The intestinal anomalies can be classified according to the time at which the intestinal rotation around the axis of the superior mesenteric stops during embryogenesis.2,3
There are few cases in the literature that correlate mesenteric varices with intestinal malrotation due to the compromised intestinal venous return.4,5 This situation occurred in our patient with no clinical repercussions to date, and no repercussions are expected after having resolved the cause.
Approximately 50% of patients with intestinal malrotation present chronic symptoms or are asymptomatic.2 The chronic presentation is more common in adults, characterised by pain and abdominal distension, nausea and vomiting for several months or years. In contrast, acute symptoms, including severe abdominal volvulus pain, is more typical of paediatric populations.
GI series are the gold standard for the diagnosis of intestinal malrotation. Typical findings are altered duodenal position (ligament of Treitz to the right of the abdomen, which has the appearance of a corkscrew), signs of duodenal obstruction, or the appearance of the duodenum beak sign if there is a volvulus. Computed tomography, with its diagnostic specificity of 80% and high sensitivity to detect abnormalities in the position of the superior mesenteric artery and vein,6 provides information about possible associated complications.7,8
Symptomatic malrotation of the midgut requires surgical intervention, but the management of asymptomatic patients is more controversial.3 Surgical treatment of intestinal malrotation was described by William Ladd for the first time in 1936,9 and it is still the pillar of treatment. The classical Ladd procedure has 4 parts: division of the Ladd bands that cover the duodenum, enlargement of the root of the small-bowel mesentery by mobilising the duodenum, division of adhesions along the axis of the superior mesenteric artery to avoid volvulus and de-torsion of the midgut volvulus, if present. Variations of the surgical technique have been reported in accordance with intraoperative findings, as in the case that we describe.7
In conclusion, intestinal malrotation in adults is difficult to diagnose, fundamentally due to the limited incidence of this disorder and its nonspecific symptoms. Imaging tests confirm the diagnosis of intestinal malrotation and its possible associated complications, but its characteristics can only be determined with laparotomy. Many authors recommend the standard and modified Ladd procedures as the surgical techniques of choice.
Please cite this article as: Gallarín Salamanca IM, Espin Jaime MT, Moreno Puertas ÁE, Salas Martínez J. Malrotación intestinal inusual en paciente adulto. Cir Esp. 2016;94:e21–e23.