To analyze the Wakabayashi & Daimon (2015) equation, as a predictive indicator of cardiometabolic diseases and its comparison with other indices.
DesignA systematic review was carried out between January and March 2023, according to the PRISMA statement.
Data sourceScopus, Web of Science, and PubMed databases were reviewed using “cardiometabolic index” (CMI) as the search term.
Study selectionThe following inclusion criteria were determined: studies in adults with cardiometabolic diseases using the Wakabayashi & Daimon (2015) CMI formula in different populations; studies that validate or compare the equation or that demonstrate the effects of the intervention.
Data extractionOf the 11 selected articles, the characteristics of the population, type of study, indicators for the validation of the CMI, the reported statistics and the conclusions that were recorded in a comparative table were obtained.
Results and conclusionsOdds ratio, hazard ratio, sensitivity, and specificity were used to assess associations, risk, effectiveness, and validity of the tests, indicating favorable relationships between the factors analyzed and the results obtained. Validation and probabilistic analysis of the CMI were performed against diverse diseases such as obesity [Man >60y=AUC=0.90 (0.75–1.00) (p=0.01), Se=100, Sp=81.8, YI=0.82 and OR 4.66 and Women >60y=AUC=0.95 (0.88–1.00), p=0.001, Se=90.0, Sp=100, YI=0.90 and OR=36.27]; cardiovascular diseases [AUC=0.617, Se=0.675, Sp=0.509; HR=1.48 (1.33, 1.65), p=<0.001], among others. In conclusion CMI is a new utility index that broadly identifies the presence of risk that leads to cardiometabolic diseases in adults.
Analizar la ecuación de Wakabayashi et al. del 2015 como indicador de predicción de enfermedades cardiometabólicas y su comparación con otros índices.
DiseñoSe realizó una revisión sistemática entre enero y marzo del 2023, de acuerdo con la declaración PRISMA.
Fuente de datosSe revisaron las bases de datos Scopus, Web of Science y PubMed utilizando «índice cardiometabólico» (ICM) como término de búsqueda.
Selección de los estudiosSe determinaron los siguientes criterios de inclusión: estudios en adultos con enfermedades cardiometabólicas que utilizaron la fórmula ICM de Wakabayashi et al. en diferentes poblaciones; que validaran o compararan la ecuación o que demostraran los efectos de la intervención.
Extracción de datosDe los 11 artículos seleccionados, se obtuvieron las características de la población, tipo de estudio, indicadores para la validación del ICM, la estadística reportada y las conclusiones que se registraron en una tabla comparativa.
Resultados y conclusionesPara evaluar las asociaciones, el riesgo, la efectividad y la validez de las pruebas se utilizaron odds ratio (OR), hazard ratio (HR), sensibilidad y especificidad, indicando relaciones favorables entre los factores analizados y los resultados obtenidos. La validación y el análisis probabilístico del ICM se realizaron frente a diversas enfermedades como obesidad (hombres >60 años=AUC=0,90 [0,75-1,00], [p=0,01], Se=100, Sp=81,8, YI=0,82 y OR 4,66; y mujeres >60 años=AUC=0,95 [0,88-1,00], p=0,001, Se=90,0, Sp=100, YI=0,90 y OR=36,27); enfermedades cardiovasculares (AUC=0,617, Se=0,675, Sp=0,509; HR=1,48 [1,33, 1,65] p≤0,001), entre otros. En conclusión, el ICM es un nuevo índice de utilidad que identifica ampliamente la presencia de riesgo para conducir a enfermedades cardiometabólicas en adultos.
Cardiometabolic risk factors (CMRF) constitute a set of conditions and behaviors that increase the probability of developing cardiovascular diseases (CVD) and metabolic disorders. These components have acquired significant relevance in the field of public health, since they represent a significant burden for population health and contribute to increased morbidity and mortality worldwide. The World Health Organization (WHO) has identified and defined arterial hypertension, dyslipidemia, smoking, obesity, lack of physical activity, unhealthy diet, and genetic predisposition as CMRF. The presence of one or more of these conditions increases the risk of developing CVD, such as coronary artery disease (CAD), myocardial infarction, and stroke, as well as metabolic disorders, such as diabetes mellitus (DM) and insulin resistance.1
Wakabayashi & Daimon proposed in 2015 a new index to identify the presence of CMRF that could lead to cardiometabolic diseases. The cardiometabolic index (CMI) is calculated as the product of the triglycerides to high density lipoprotein cholesterol (TG/HDL-C) and waist to height ratio (WHtR) to predict cardiometabolic risk (CMR) in adults. TG/HDL-C has been reported to be a good predictor of CVD risk, and that interventions against high TG and low HDL-C levels should be included to prevent heart disease.2,3 Meanwhile WHtR is a central component of metabolic syndrome (MS), it is also a better indicator than waist circumference (WC) alone and body mass index (BMI) for detecting abdominal obesity.4 Authors proved that taking an indicator of CVD and combining it with the WHtR the CMI is also a useful marker to discriminate against hyperglycemia and DM.
Study was conducted on 10,196 Japanese men and women at ages between 35 and 40 years, who had undergone medical health checkups and were not taking any dyslipidemia medication. Blood hemoglobin A1c was used to assess for hyperglycemia. Authors found significant correlations between CMI and hemoglobin in both women (r=0.234, p<0.01) and in men (r=0.216, p<0.01). The area under the receiver operating characteristic (ROC) curve (AUC-ROC) was 0.761 for hyperglycemia and 0.831 for DM in women, and 0.724 and 0.745 for men respectively. Specificity (Sp) and sensitivity (Se) for hyperglycemia was 79.3% and 64.5% in women and 73.4% and 61.6% in men, respectively; for DM, Sp was 78.5% and Se 80.0% in women and 74.5% and 65.5% in men, respectively. Odds ratio (OR) were 6.98 for hyperglycemia and 14.61 for DM in women, and 4.42 and 5.38 in men, respectively. Blood hemoglobin A1c values were distributed in ascending quartiles.
Results considered the CMI as a new index, which reflects both adiposity and blood lipids and is also useful to differentiate hyperglycemia and DM.4
Wakabayashi & Daimon's CMI has been frequently validated by the same authors from 2015 to date and themselves have analyzed their index in different populations and diseases, as well as other researchers, who have also compared it with other indices reported in the scientific literature.
It is interesting to identify how the studies where the CMI has been considered the best indicator to predict diseases associated with CMRF, and this review focused on studies where this relationship has been proved.
The objective is to analyze the Wakabayashi & Daimon equation (2015), as an indicator for cardiometabolic diseases prediction and its comparison with other indexes.
MethodA systematic review was carried out according to the parameters and guidelines of the PRISMA declaration,5 from January 30 to March 19, 2023, in Scopus, Web of Science and PubMed databases with “cardiometabolic index” as the search chain.
Inclusion criteria were: articles from studies conducted in adults with cardiometabolic diseases; that Wakabayashi & Daimon CMI formula (2015) had been used in different populations; that the equation had been validated and/or compared, correlated, or used to demonstrate the effects of an intervention.
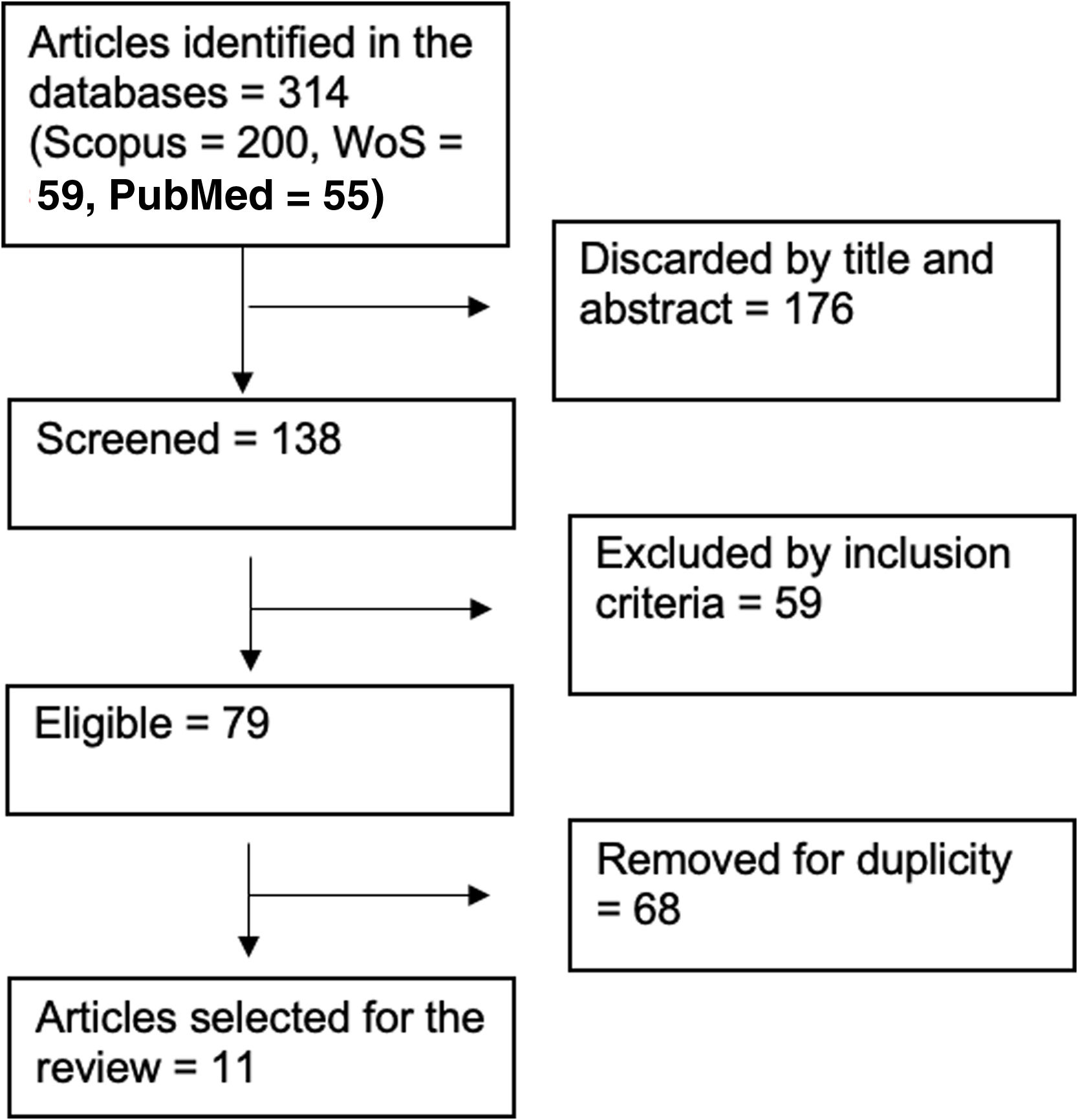
Selection process began by reading the title and abstract of each article identified by the terms of searching, discarding those that did not match the criteria search. After reading the full text, those that did not meet the inclusion criteria were excluded; then duplicated articles were eliminated. Finally, a total of 11 articles were selected for the review.
ResultsStudies provided data from 2017 to 2023 in adult individuals. 314 articles were identified in databases of which 11 studies were considered for the review. Most of the included studies were conducted in Asiatic population from China (66.66%) and Japan (16.66%). Other studies were performed in Mexican (8.33%) and Iranian (8.33%) people. Diagram of the selection process is shown in Fig. 1.
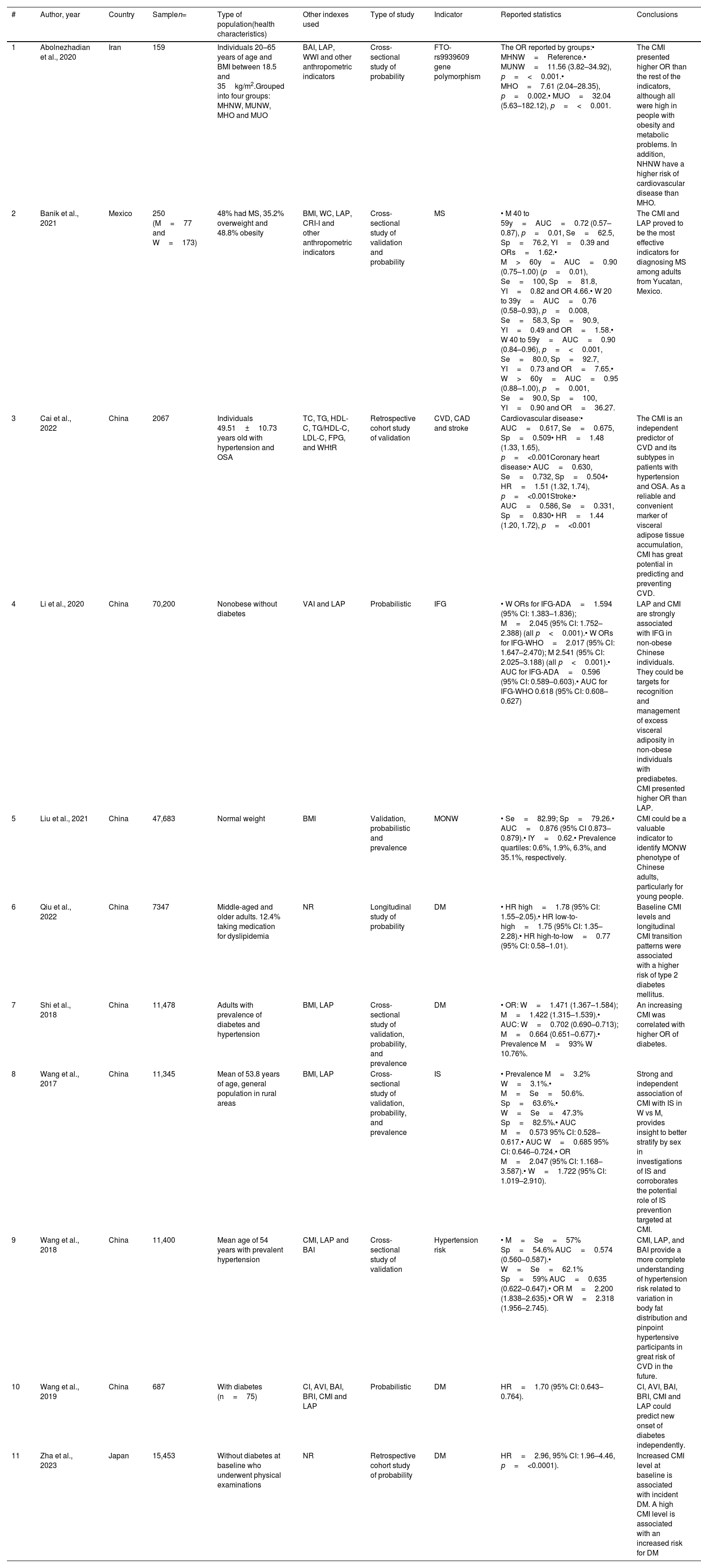
Table 1 shows the main characteristics of the analyzed articles, where validation and probabilistic studies with the CMI were performed against different indicators such as: FTO-rs9939609 gen related to obesity,6,7 MS,8,9 CVD and their subtypes,10,11 impaired fasting glucose,12 DM13,14 and hypertension risk.15 Other studies compared the CMI with indices such as: atherogenic index of plasma, lipid accumulation product index (LAP), weight-adjusted-waist index, BMI, WC, Castelli Risk Index, body adiposity index, abdominal volume index, body roundness index, total cholesterol, TG, HDL-C, TG/HDL-C ratio, low density lipoprotein cholesterol (LDL-C), fasting plasma glucose, and WHtR among other anthropometric indicators.
Characteristics of the studies included in the review.
| # | Author, year | Country | Samplen= | Type of population(health characteristics) | Other indexes used | Type of study | Indicator | Reported statistics | Conclusions |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Abolnezhadian et al., 2020 | Iran | 159 | Individuals 20–65 years of age and BMI between 18.5 and 35kg/m2.Grouped into four groups: MHNW, MUNW, MHO and MUO | BAI, LAP, WWI and other anthropometric indicators | Cross-sectional study of probability | FTO-rs9939609 gene polymorphism | The OR reported by groups:• MHNW=Reference.• MUNW=11.56 (3.82–34.92), p=<0.001.• MHO=7.61 (2.04–28.35), p=0.002.• MUO=32.04 (5.63–182.12), p=<0.001. | The CMI presented higher OR than the rest of the indicators, although all were high in people with obesity and metabolic problems. In addition, NHNW have a higher risk of cardiovascular disease than MHO. |
| 2 | Banik et al., 2021 | Mexico | 250 (M=77 and W=173) | 48% had MS, 35.2% overweight and 48.8% obesity | BMI, WC, LAP, CRI-I and other anthropometric indicators | Cross-sectional study of validation and probability | MS | • M 40 to 59y=AUC=0.72 (0.57–0.87), p=0.01, Se=62.5, Sp=76.2, YI=0.39 and ORs=1.62.• M>60y=AUC=0.90 (0.75–1.00) (p=0.01), Se=100, Sp=81.8, YI=0.82 and OR 4.66.• W 20 to 39y=AUC=0.76 (0.58–0.93), p=0.008, Se=58.3, Sp=90.9, YI=0.49 and OR=1.58.• W 40 to 59y=AUC=0.90 (0.84–0.96), p=<0.001, Se=80.0, Sp=92.7, YI=0.73 and OR=7.65.• W>60y=AUC=0.95 (0.88–1.00), p=0.001, Se=90.0, Sp=100, YI=0.90 and OR=36.27. | The CMI and LAP proved to be the most effective indicators for diagnosing MS among adults from Yucatan, Mexico. |
| 3 | Cai et al., 2022 | China | 2067 | Individuals 49.51±10.73 years old with hypertension and OSA | TC, TG, HDL-C, TG/HDL-C, LDL-C, FPG, and WHtR | Retrospective cohort study of validation | CVD, CAD and stroke | Cardiovascular disease:• AUC=0.617, Se=0.675, Sp=0.509• HR=1.48 (1.33, 1.65), p=<0.001Coronary heart disease:• AUC=0.630, Se=0.732, Sp=0.504• HR=1.51 (1.32, 1.74), p=<0.001Stroke:• AUC=0.586, Se=0.331, Sp=0.830• HR=1.44 (1.20, 1.72), p=<0.001 | The CMI is an independent predictor of CVD and its subtypes in patients with hypertension and OSA. As a reliable and convenient marker of visceral adipose tissue accumulation, CMI has great potential in predicting and preventing CVD. |
| 4 | Li et al., 2020 | China | 70,200 | Nonobese without diabetes | VAI and LAP | Probabilistic | IFG | • W ORs for IFG-ADA=1.594 (95% CI: 1.383–1.836); M=2.045 (95% CI: 1.752–2.388) (all p<0.001).• W ORs for IFG-WHO=2.017 (95% CI: 1.647–2.470); M 2.541 (95% CI: 2.025–3.188) (all p<0.001).• AUC for IFG-ADA=0.596 (95% CI: 0.589–0.603).• AUC for IFG-WHO 0.618 (95% CI: 0.608–0.627) | LAP and CMI are strongly associated with IFG in non-obese Chinese individuals. They could be targets for recognition and management of excess visceral adiposity in non-obese individuals with prediabetes. CMI presented higher OR than LAP. |
| 5 | Liu et al., 2021 | China | 47,683 | Normal weight | BMI | Validation, probabilistic and prevalence | MONW | • Se=82.99; Sp=79.26.• AUC=0.876 (95% CI 0.873–0.879).• IY=0.62.• Prevalence quartiles: 0.6%, 1.9%, 6.3%, and 35.1%, respectively. | CMI could be a valuable indicator to identify MONW phenotype of Chinese adults, particularly for young people. |
| 6 | Qiu et al., 2022 | China | 7347 | Middle-aged and older adults. 12.4% taking medication for dyslipidemia | NR | Longitudinal study of probability | DM | • HR high=1.78 (95% CI: 1.55–2.05).• HR low-to-high=1.75 (95% CI: 1.35–2.28).• HR high-to-low=0.77 (95% CI: 0.58–1.01). | Baseline CMI levels and longitudinal CMI transition patterns were associated with a higher risk of type 2 diabetes mellitus. |
| 7 | Shi et al., 2018 | China | 11,478 | Adults with prevalence of diabetes and hypertension | BMI, LAP | Cross-sectional study of validation, probability, and prevalence | DM | • OR: W=1.471 (1.367–1.584); M=1.422 (1.315–1.539).• AUC: W=0.702 (0.690–0.713); M=0.664 (0.651–0.677).• Prevalence M=93% W 10.76%. | An increasing CMI was correlated with higher OR of diabetes. |
| 8 | Wang et al., 2017 | China | 11,345 | Mean of 53.8 years of age, general population in rural areas | BMI, LAP | Cross-sectional study of validation, probability, and prevalence | IS | • Prevalence M=3.2% W=3.1%.• M=Se=50.6%. Sp=63.6%.• W=Se=47.3% Sp=82.5%.• AUC M=0.573 95% CI: 0.528–0.617.• AUC W=0.685 95% CI: 0.646–0.724.• OR M=2.047 (95% CI: 1.168–3.587).• W=1.722 (95% CI: 1.019–2.910). | Strong and independent association of CMI with IS in W vs M, provides insight to better stratify by sex in investigations of IS and corroborates the potential role of IS prevention targeted at CMI. |
| 9 | Wang et al., 2018 | China | 11,400 | Mean age of 54 years with prevalent hypertension | CMI, LAP and BAI | Cross-sectional study of validation | Hypertension risk | • M=Se=57% Sp=54.6% AUC=0.574 (0.560–0.587).• W=Se=62.1% Sp=59% AUC=0.635 (0.622–0.647).• OR M=2.200 (1.838–2.635).• OR W=2.318 (1.956–2.745). | CMI, LAP, and BAI provide a more complete understanding of hypertension risk related to variation in body fat distribution and pinpoint hypertensive participants in great risk of CVD in the future. |
| 10 | Wang et al., 2019 | China | 687 | With diabetes (n=75) | CI, AVI, BAI, BRI, CMI and LAP | Probabilistic | DM | HR=1.70 (95% CI: 0.643–0.764). | CI, AVI, BAI, BRI, CMI and LAP could predict new onset of diabetes independently. |
| 11 | Zha et al., 2023 | Japan | 15,453 | Without diabetes at baseline who underwent physical examinations | NR | Retrospective cohort study of probability | DM | HR=2.96, 95% CI: 1.96–4.46, p=<0.0001). | Increased CMI level at baseline is associated with incident DM. A high CMI level is associated with an increased risk for DM |
AUC: area under the receiver operating characteristic (ROC) curve; AVI: abdominal volume index; BAI: body adiposity index; BMI: body mass index; kg/m2: kilograms per meter squared; BRI: body roundness index; CI: Conicity index; CMI: cardiometabolic index; CRI-I: Castelli Risk Index; CVD: cardiovascular disease; DM: diabetes mellitus; FPG: fasting plasma glucose; HDL-C: high density lipoprotein cholesterol; HR: the hazard ratios; IFG: impaired fasting glucose; IS: ischemic stroke; LAP: lipid accumulation product index; LDL-C: low density lipoprotein cholesterol; M: men; MHNW: metabolically healthy normal weight; MHO: metabolically healthy obese; MONW: metabolically obese normal weight; MS: metabolic syndrome; MUNW: metabolically unhealthy normal weight; MUO: metabolically unhealthy obese; NR: not reported; OR: odds ratio; OSA: obstructive sleep apnea; Se: sensitivity; Sp: specificity; TC: total cholesterol; TG: triglyceride; VAI: visceral adiposity index; W: women; WC: waist circumference; WHtR: waist to height ratio; WWI: weight-adjusted-waist index; YI: Youden index.
Included articles reported cross-sectional, cohort, and longitudinal studies where prevalence, validation, and probabilistic analysis were performed. Studies reported their results grouped by quartiles, age, and cardiometabolic indicators. OR and hazard ratio (HR) made possible to compare the relative risk between two groups exposed to different factors, the first being used in case–control studies, and the second in prospective cohort studies. On the other hand, Se and Sp were the performance measures of diagnostic tests. Se indicated the ability of a test to correctly identify positive cases, while Sp indicated the ability of a test to correctly identify negative cases.
The use of these measures made possible to identify significant associations between variables, evaluate the risk of events or the results, and determine the effectiveness and validity of the tests used. Values obtained from these measurements indicated a favorable relationship between the factors analyzed and the results obtained.
DiscussionLipid-related indices have been proposed for some time to predict and prevent CVD. LDL-C to HDL-C ratio (LDL-C/HDL-C) and TC/HDL-C ratio are classic atherogenic indices.16 Moreover, LAP index has recently been proposed as a good predictor for CVD.17 However, LAP has limitations because WC is corrected by constants by sex to be able to calculate it.4
TG/HDL-C ratio has been proposed as a good discriminator of CVD, for this reason it is included in the CMI proposed by Wakabayashi & Daimon (2015). It also incorporates the WHtR that is a more reasonable indicator for determining abdominal obesity, linked to insulin resistance and therefore to metabolic disease; it has also been shown that can better discriminate CAD and CVRF than WC alone and BMI.18,19 Therefore, the CMI may be a more reasonable predictor of cardiovascular risk than other indices such as WC, LAP among other.4
TG and other indices associated with the incidence of CVD risk have been related and found that fasting TG is an independent predictor of ischemic CVD, nevertheless, CMI could be a better predictor since includes variables as the WHtR that can discriminate insulin resistance, hyperglycemia, and DM.18,20
Compared with different indicators and indexes, CMI has shown to be more effective as a predictor of CVD and its subtypes (CAD and stroke),10 MS, DM14 and hypertension.10,15 It is also related to the probability of the presence of FTO,6 impaired fasting glucose, and as an indicator of the phenotype of metabolically unhealthy normal weight people.7
Other researchers have found that besides to being related to cardiometabolic diseases, CMI usefulness has also been associated to non-alcoholic fatty liver disease,21,22 erectile dysfunction,23 pancreatitis,24 hyperuricemia,25 kidney cancer,26 chronic kidney disease, prostatic hyperplasia,27 and atherosclerosis,28 among other pathologies.29
Furthermore, the effectiveness of the CMI has been tested in different populations, noticing that there are factors that influence the CMI, such as moderate alcohol consumption which attenuates the association between the CMI and hyperglycemia, therefore it must be taken into consideration the habitual drinking status when using the CMI related to atherosclerotic disease and DM risk.30 WC is lower in light-to-moderate drinkers than in non-drinkers men with DM, and this is mainly due to an association between alcohol consumption and HDL-C.31 Additionally, smoking is positively associated with lipid-related indices in women regardless of alcohol consumption.32
Age is also an influencing factor of CMI differently in men and women; CMI is higher in middle-aged men than in younger and older men, and tending to be higher with increasing age in older women. Also, the association between CMI and DM weakens with increasing age in both men and women.33
There are more validation studies that were carried out in other countries, so these outcomes could be extrapolated to other populations. However, only those analyzes that met the established inclusion criteria were included in this review. Due to this, 83% of the sample comes from China or Japan, and the remaining 17% was from Mexico and Iran.
Most participants of studies in this review were patients with diabetes or glucose intolerance. This is due to the novelty of the cardiometabolic index, which, unlike other risk indicators, stands out for its validity in determining risk of type 2 diabetes mellitus without requiring measurements of glucose, glycated hemoglobin, or others in patients.
ConclusionsCMI is a new useful index that widely identifies the presence of CMRF that could lead to cardiometabolic diseases in adults. Using four variables, the index is also capable of discriminating against insulin resistance and DM.
Wakabayashi & Daimon proposed in 2015 a new index to identify the presence of cardiometabolic risk factors. It is calculated as the product of the TG/HDL-C and WHtR in adults.
What is added?Wakabayashi & Daimon's cardiometabolic index (CMI) has successfully been validated and analyzed in different populations and diseases. Other researchers have also compared it with distinct indices and pathologies revealing the usefulness of CMI.
What are the implications?CMI has shown to be effective as a predictor of cardiovascular diseases and its subtypes, metabolic syndrome, diabetes mellitus and hypertension.
This research has not received specific support from public sector agencies, commercial sector, or non-profit entities.
Conflicts of interestNone declared.