Cardiac trauma is a significant cause of death. Thoracotomy is an advanced resuscitation technique aimed at restoring cardiac output by relieving cardiac tamponade and repairing cardiac injuries.
ObjectiveA case report of a patient who suffered a penetrating precordial wound that was resolved with a resuscitative thoracotomy was conducted. A narrative review of the current state of the art is presented.
ConclusionsThoracic trauma associated with cardiac injury is a potentially lethal condition. Despite early diagnosis, overall survival is anecdotal. Medical teams familiar with advanced resuscitation techniques such as resuscitative thoracotomy are required.
El trauma cardíaco es una causa importante de muerte. La toracotomía es una técnica de reanimación avanzada que tiene como objetivo la restauración del gasto cardíaco mediante la liberación del taponamiento cardíaco y la reparación de lesiones cardíacas.
ObjetivoSe realizó un reporte de caso de un paciente que sufrió una herida precordial penetrante que resolvió con una toracotomía resucitativa. Se presenta una revisión narrativa del estado del arte.
ConclusionesEl trauma torácico asociado al trauma cardíaco es una condición potencialmente letal. Pese a un diagnóstico precoz, la supervivencia global es anecdótica. Se requiere de equipos médicos familiarizados con técnicas de reanimación avanzada como la toracotomía resucitativa.
Cardiac trauma is a potentially life-threatening condition. When penetrating cardiac injury is associated with massive hemothorax, cardiac tamponade, and cardiac arrest, the mortality rate reported in the literature is 100%. Historically, cardiac injuries have been associated with high mortality rates. For decades, they were considered untreatable. Around 90% of patients die before reaching the hospital, and different case series have reported survival rates close to 1%. The survival rate for patients in shock after an open chest injury is approximately 35%, while for closed chest traumas, this rate is around 2%. Armed conflict and urban violence in Colombia generate a high incidence of traumatic injuries, but there are few reports in the literature on experiences in their management.1 Resuscitative thoracotomy is an advanced resuscitation technique performed in patients with cardiovascular collapse secondary to cardiac tamponade. Its goal is to restore cardiac output, decompress cardiac tamponade, perform direct cardiac massage, and prevent exsanguination. The proper management of intravenous fluids, bleeding control, obstructive shock management, hemorrhage control, and the prioritized use of blood products are fundamental factors for improving the prognosis of this population. This case report exemplifies how proper and multidisciplinary trauma management can ensure the patient's survival.2
MethodologyInformed consent and approval from the institutional bioethics committee were obtained. A retrospective observational study was conducted on a patient who suffered a penetrating precordial wound leading to mixed shock. A narrative review of the current state of the art on resuscitative thoracotomy is presented.
Case descriptionA 25-year-old male patient with a history of substance abuse presented to the emergency department after sustaining a penetrating precordial wound with a sharp object in the left ninth intercostal space along the posterior axillary line. During the initial assessment, signs of circulatory insufficiency (shock index of 2.23) were observed, which progressed to a cardiac arrest secondary to pulseless electrical activity. Cardiopulmonary resuscitation (CPR) maneuvers were initiated, and the FAST-E protocol was applied, revealing cardiac tamponade and massive hemothorax. A resuscitative thoracotomy was performed using an anterolateral approach. The chest was impregnated with chlorhexidine without stopping compressions. The injured person's left arm was positioned above the head. After disinfection, a sterile surgical dressing was placed over the area and a sterile field was used for instrumentation.
We made an incision at the level of the fifth intercostal space from the parasternal edge to the mid-axillary line. We traversed the skin, subcutaneous tissue, fascia, intercostal muscles, and pleura. The intercostal muscles were opened with a scalpel. We performed blunt dissection of the tissues with fingers to enter the thoracic cavity. A Finochietto retractor was inserted between the ribs to open and adequately visualize the organs of the thoracic cavity once the pleura was sectioned. The internal mammary arteries began to bleed, so bleeding control was achieved by ligature. Subsequently, the pericardium was opened longitudinally.
Since it can be difficult for non-surgical specialties to identify the phrenic nerve in emergency situations, we made a small incision with scissors that we expanded with fingers. We evacuated clots from the pericardial sac and controlled bleeding by inserting a Foley catheter. A two-centimeter wound in the left ventricle was documented and sutured with non-absorbable 3/0 suture. A two-minute cycle of direct cardiac compressions was performed, achieving return of spontaneous circulation. To avoid overlooking posterior cardiac injuries, the heart was quickly moved anteriorly to prevent compromising venous return. The lung was medially elevated, and a massive hemothorax of 4000ml was evacuated.
After achieving return of spontaneous circulation, tranexamic acid, cefazolin, norepinephrine, and dobutamine were administered for support. After the initial stabilization, we corrected an accidental ligature of the anterior descending artery that occurred during the emergency reparation of the left ventricle wound. A massive transfusion was initiated following predictive scales (ABC≥2, CI>1, RABT≥2). Thromboelastography documented a prolonged reaction time, consistent with trauma-induced coagulopathy, so 20ml/kg of fresh frozen plasma was transfused.
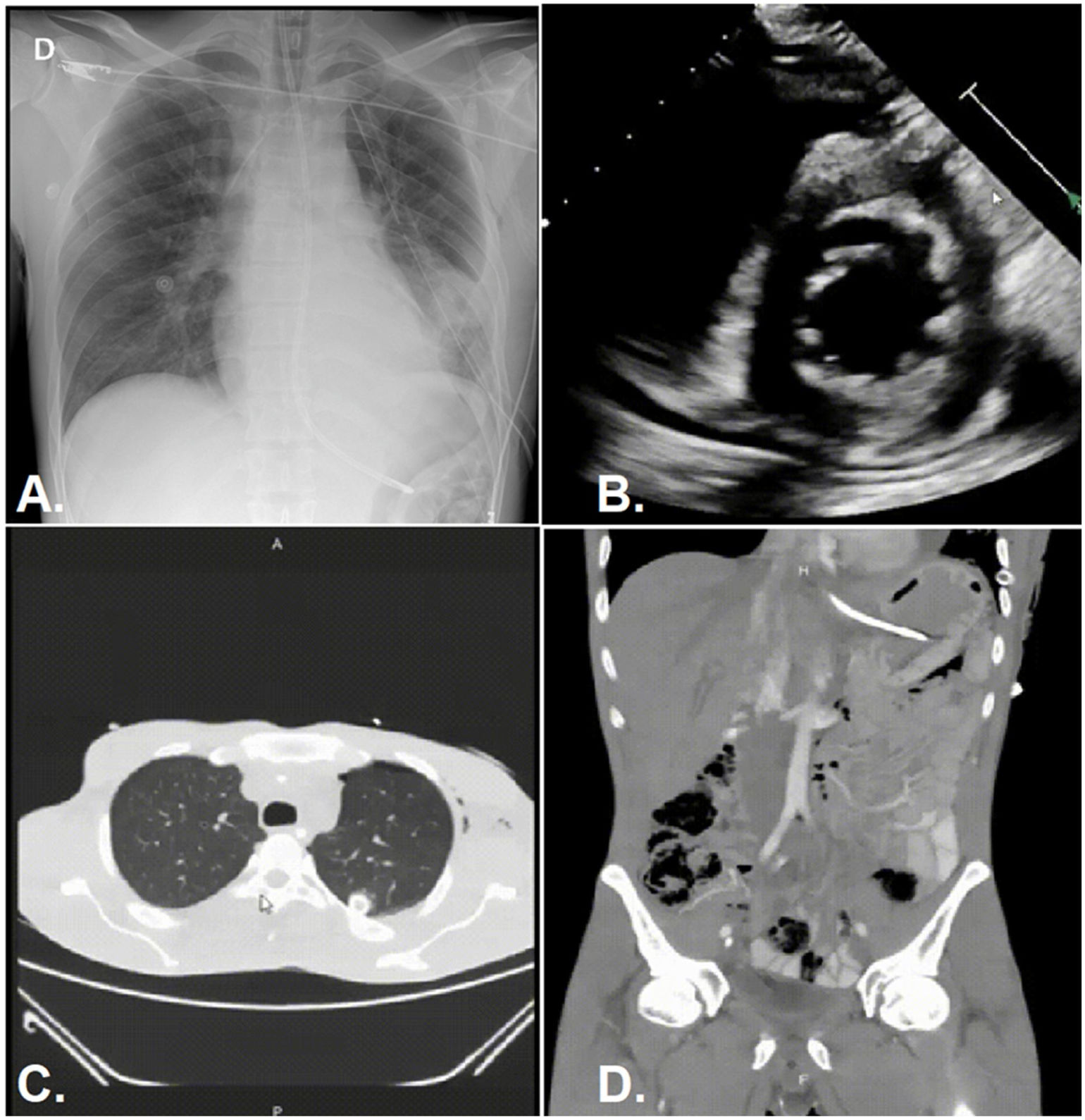
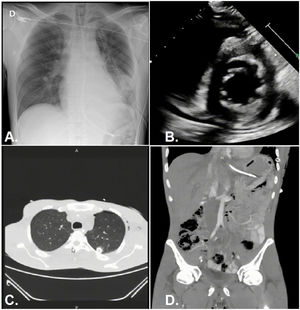
The patient was transferred to the intensive care unit (ICU), where laboratory analyses and additional imaging studies were conducted (Fig. 1). Antibiotic therapy with cefazolin was provided for five days. During the stay in the ICU, the patient experienced episodes of psychomotor agitation and episodes of heteroaggression toward healthcare personnel. Multidisciplinary management involving psychiatry was required to initiate antipsychotic therapy with olanzapine and lorazepam. Cooperative sedation with dexmedetomidine was employed. One week later, the patient underwent a surgical procedure in the operating room to drain residual pleural effusion and perform decortication of the left lung using video-assisted thoracoscopic surgery (VATS). After two weeks, the patient was referred to another institution to start a detoxification process. After discharge, it was not possible to conduct a new physical assessment with the patient as they moved to another city. A follow-up echocardiogram documented altered motility in the apical segments of the septum and the lower wall of the left ventricle with preserved ejection fraction and mild dilation of the right ventricle. However, they reported being functional and free of sequelae. Furthermore
Imaging. (A) Post-thoracotomy AP chest X-ray: Left pneumothorax chamber in re-expansion with thoracostomy tube in proper position. (B) Post-cardiorrhaphy echocardiogram (report): impaired motility in the antero-septal–apical wall of the left ventricle, EF (ejection fraction) of 58%, mild dilation of the right ventricle, slight pericardial effusion. (C) Chest CT scan: coagulated hemothorax in the left lower lobe, posterior right basal pleural effusion with laminar free-flowing characteristics and passive atelectasis of underlying lung parenchyma, traumatic injury to the cardiac apex with minimal pericardial effusion, complete re-expansion of the left pneumothorax chamber with thoracostomy tube in proper position. (D) Contrast-enhanced abdominal CT scan: laceration in the lower renal pole with laminar distribution of perirenal, pararenal, left paracolic, and pelvic fluid. Extraluminal gas adjacent to the splenic–colonic angle.
The survival of trauma patients depends on proper resource management. Protocols such as Focused Assessment with Sonography in Trauma (FAST) enable the identification of potentially lethal injuries amenable to intervention. According to the Oklahoma registry, the mortality rate for penetrating cardiac injuries is 51.9%, while for blunt injuries, it is 26.3%. When injuries are associated with cardiac tamponade, hemothorax, or vascular injury, the morbidity and mortality rates are higher.3
The estimated homicide rate in Colombia per 100,000 inhabitants during 2019 was 38.28. The time limitation in prehospital care for patients with severe injuries is also an important concept to highlight, as no patient should undergo more than 10min of on-scene stabilization by the prehospital team before transportation to definitive care at a trauma center. The overall mortality rate in patients whose prehospital care exceeds 10min is approximately 84%. A ten-year retrospective study conducted in Bogotá documented 240 cases of penetrating cardiac trauma. The average age was 27 years, and the predominantly affected gender was male, with an overall mortality rate of 14.6% and signs of cardiac tamponade were found in 67% of cases. The average time interval between injury and surgical procedure/resuscitative thoracotomy was 60min.4 These data contrast with the findings described in our study.
Resuscitative thoracotomy is an advanced cardiopulmonary resuscitation technique that is not well known in the ICU, despite its potential life-saving effect. This technique dates back to the 19th century and was pioneered by Ludwing Rehn and Francisco Romero. With the increase in open thoracic injuries, the rise in social violence, and the occurrence of armed conflicts, there has been a renewed interest in this procedure, which could be beneficial in conflict zones like Colombia. The procedure described by Rehn and Romero continues to save lives in countries plagued by violence.5
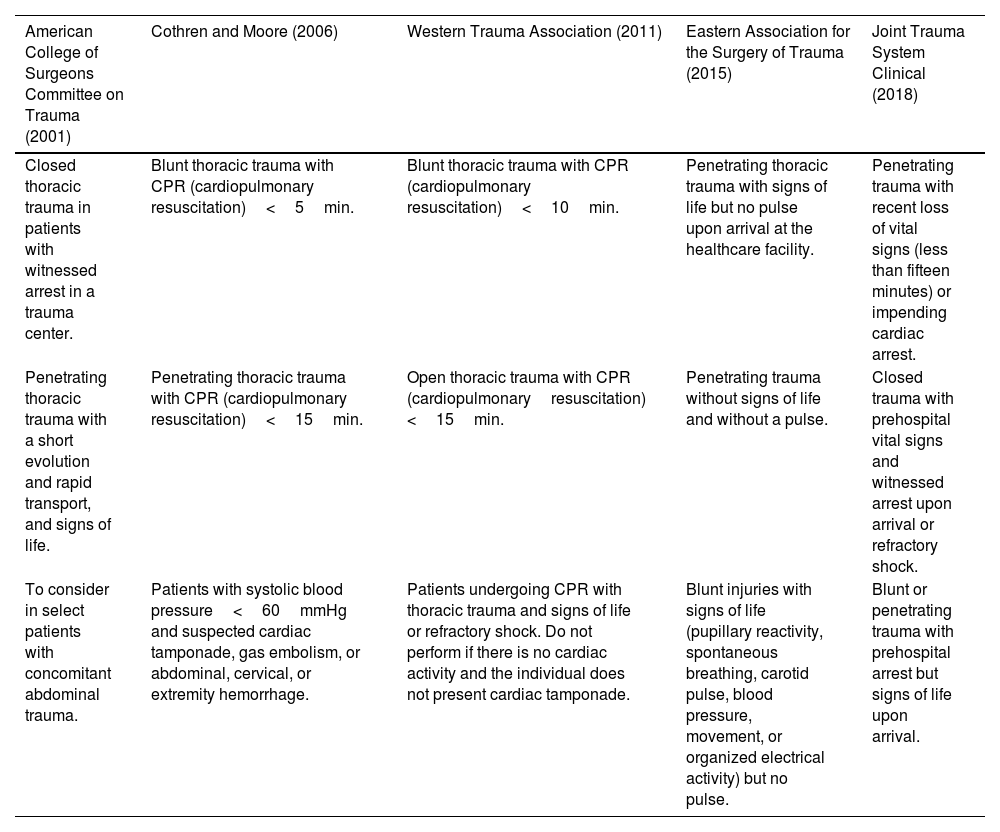
In the last two decades, multiple recommendations have been published regarding this procedure (Table 1),6–8 Cardiac tamponade is characterized by diastolic dysfunction that leads to the development of obstructive shock. Beck's triad (jugular distension, hypotension, and muffled heart sounds) occurs in less than 30% of cases, reducing its diagnostic utility. According to ATLS guidelines, resuscitative thoracotomy can be performed if there is no return of spontaneous circulation. This emergent procedure can be performed by surgeons, emergency physicians, and intensivists. The incision should be made in a single stroke, starting at the sternum and continuing along the upper border of the fifth rib until reaching the axilla. A pleurotomy should then be performed. If necessary, the sternum can be separated using a Gigli saw, and the lung can be explored for air leaks or controllable hemorrhages using a Finocchietto retractor. In cases of massive bleeding or air leaks, the pulmonary hilum can be clamped, and the aorta can be occluded. The pericardium is incised when there is doubt about injuries. The incision should be careful, parallel to the phrenic nerve. In cases of ventricular injuries, bleeding can be controlled with direct pressure, and the injury should be repaired, ensuring that the coronary vessels are not trapped. After achieving hemostasis, if necessary, direct cardiac massage or internal defibrillation should be performed. In cases of persistent hypotension, some authors recommend cross-clamping the thoracic aorta to increase coronary and cerebral perfusion (Coronary perfusion pressure=Diastolic blood pressure−Pulmonary capillary wedge pressure), (Cerebral perfusion pressure=Mean arterial pressure−Intracranial pressure) Emergency thoracotomy is a time-dependent procedure. A systematic review reported a survival rate of 12.9% for emergency thoracotomies. However, when penetrating cardiac injury is associated with massive hemothorax, as in the present report, the mortality rate is close to 100%. It is estimated that 26% of survivors of emergency thoracotomy will experience severe/moderate cognitive impairment, and 25% will suffer from post-traumatic stress disorders.8
Indications for emergency thoracotomy according to available guidelines.
| American College of Surgeons Committee on Trauma (2001) | Cothren and Moore (2006) | Western Trauma Association (2011) | Eastern Association for the Surgery of Trauma (2015) | Joint Trauma System Clinical (2018) |
|---|---|---|---|---|
| Closed thoracic trauma in patients with witnessed arrest in a trauma center. | Blunt thoracic trauma with CPR (cardiopulmonary resuscitation)<5min. | Blunt thoracic trauma with CPR (cardiopulmonary resuscitation)<10min. | Penetrating thoracic trauma with signs of life but no pulse upon arrival at the healthcare facility. | Penetrating trauma with recent loss of vital signs (less than fifteen minutes) or impending cardiac arrest. |
| Penetrating thoracic trauma with a short evolution and rapid transport, and signs of life. | Penetrating thoracic trauma with CPR (cardiopulmonary resuscitation)<15min. | Open thoracic trauma with CPR (cardiopulmonaryresuscitation) <15min. | Penetrating trauma without signs of life and without a pulse. | Closed trauma with prehospital vital signs and witnessed arrest upon arrival or refractory shock. |
| To consider in select patients with concomitant abdominal trauma. | Patients with systolic blood pressure<60mmHg and suspected cardiac tamponade, gas embolism, or abdominal, cervical, or extremity hemorrhage. | Patients undergoing CPR with thoracic trauma and signs of life or refractory shock. Do not perform if there is no cardiac activity and the individual does not present cardiac tamponade. | Blunt injuries with signs of life (pupillary reactivity, spontaneous breathing, carotid pulse, blood pressure, movement, or organized electrical activity) but no pulse. | Blunt or penetrating trauma with prehospital arrest but signs of life upon arrival. |
After the surgical procedure, the proper management in the ICU will determine the survival outcome. Another complication associated with cardiac trauma is hemorrhagic shock (Table 2), where exsanguination leads to inadequate oxygen supply, explained by a decrease in cardiac output, cardiac index, and arterial oxygen content, along with lower PaO2, SaO2, and hemoglobin levels (DO2=CO×CaO2×10), (IDO2=CI×CaO2×10), (CaO2=Hb×1.36×SaO2)+(PaO2×0.0031). Traumatic etiology accounts for 87% of deaths associated with shock. Hypovolemia in hemorrhagic shock causes dysfunction of the nervous system. Inadequate oxygen supply leads to tissue hypoperfusion, ischemia, and the release of toxins. At the cellular level, cells shift to anaerobic metabolism due to oxygen debt. Anaerobic metabolism increases lactate levels, inorganic phosphates, and oxygen radicals. This state of stress releases damage-associated molecular patterns (DAMPs or alarmins), triggering a systemic inflammatory response. Necrosis, apoptosis, hypovolemia, and vasoconstriction cause damage to the kidneys, liver, intestines, heart, brain, endothelium, and muscles. In the bleeding area, primary, secondary, and distal hemostasis mechanisms are activated, and fibrinolytic activity increases to prevent microvascular thrombosis. Excessive plasmin activity leads to a state of hyperfibrinolysis, resulting in disseminated intravascular coagulation. Some iatrogenic factors, such as over-resuscitation with crystalloids or the use of hydroxyethyl starch, dilute coagulation factors, worsen hypothermia, exacerbate acidosis, deplete energy reserves, and further decrease oxygen transport. The median time to death after the onset of hemorrhagic shock is two hours. Therapeutic actions should focus on rapidly controlling the bleeding, restoring blood volume, and optimizing oxygen transport. The survival chain for patients with severe hemorrhage begins in the prehospital setting, where the priorities are obtaining large peripheral vascular access, controlling bleeding through direct pressure or tourniquets, and rapid transportation to a hospital facility.8,9
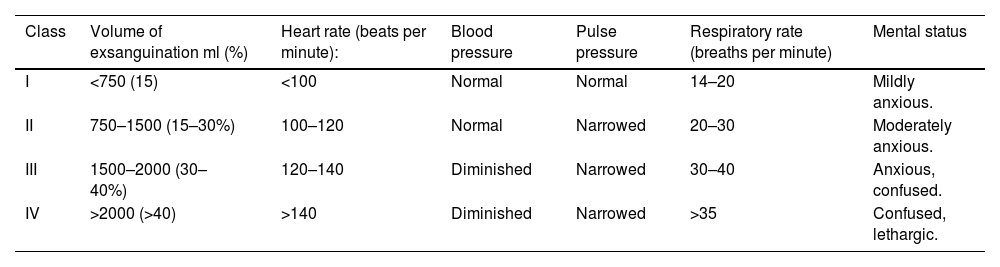
Classification of hemorrhagic shock according to the American College of Surgeons Committee on Trauma.
| Class | Volume of exsanguination ml (%) | Heart rate (beats per minute): | Blood pressure | Pulse pressure | Respiratory rate (breaths per minute) | Mental status |
|---|---|---|---|---|---|---|
| I | <750 (15) | <100 | Normal | Normal | 14–20 | Mildly anxious. |
| II | 750–1500 (15–30%) | 100–120 | Normal | Narrowed | 20–30 | Moderately anxious. |
| III | 1500–2000 (30–40%) | 120–140 | Diminished | Narrowed | 30–40 | Anxious, confused. |
| IV | >2000 (>40) | >140 | Diminished | Narrowed | >35 | Confused, lethargic. |
The blood loss and percentage correspond to a 70kg man.
Hypotension is a late indicator of shock that appears after losing more than 30% of blood volume. In traumatized patients, bleeding can come from hidden sources, and FAST (Focused Assessment with Sonography in Trauma) can help identify them. Echocardiography allows for the evaluation of cardiac filling and contractility, while base deficit, lactate levels, and capillary refill time facilitate the assessment of tissue hypoperfusion. Complete blood count, electrolyte levels, coagulation times, and fibrinogen levels are necessary to evaluate the patient's coagulation status.8 Viscoelastic tests such as thromboelastography and rotational thromboelastometry have been proposed as strategies to optimize the utilization of blood bank resources.9
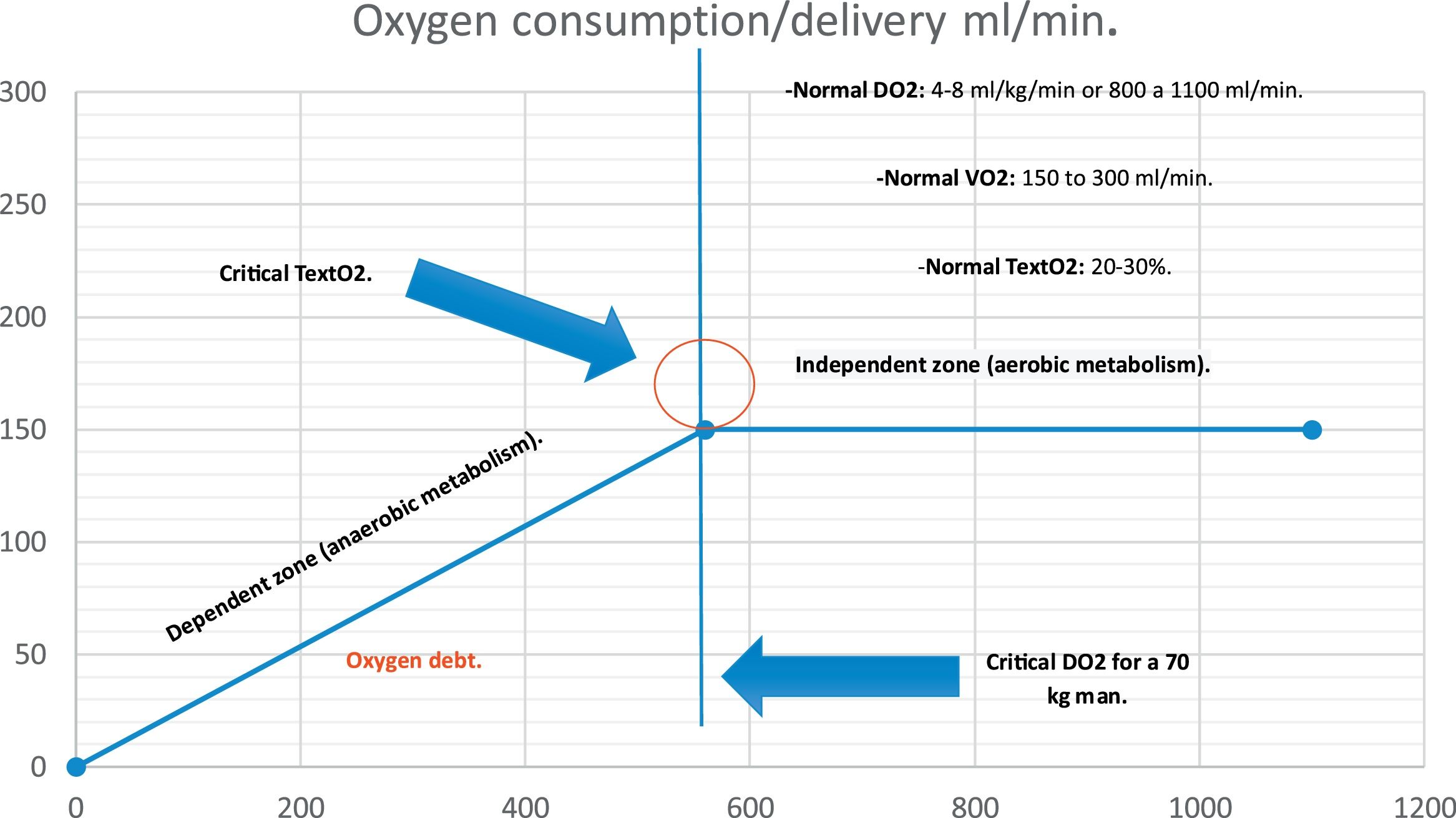
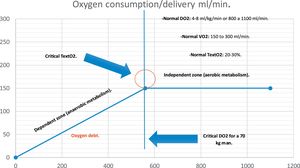
The success of resuscitation requires aggressive measures to prevent further oxygen debt accumulation (Fig. 2). In the presented case, the restrictive management of intravenous fluids, control of bleeding, management of concomitant obstructive shock, and prioritized use of blood products over crystalloids were crucial prognostic factors that prevented the development of coagulopathy. Delaying fluid resuscitation until definitive hemostasis is achieved improves survival among patients with penetrating trauma by reducing the risk of dilutional coagulopathy. On the other hand, the benefits of hypertonic solutions, dextrans, albumin, or balanced solutions compared to 0.9% saline solution are controversial in critically ill. The utility of isotonic crystalloids after the initial transient expansion is debatable, and their liberal use should be avoided. Over-resuscitation with intravenous fluids increases the risk of respiratory failure, compartment syndrome, and coagulopathy. It is recommended to limit infusions to a maximum of three liters within the first six hours after hospital arrival. Procoagulant hemostatic agents, such as recombinant activated factor VII, tranexamic acid, prothrombin complex concentrate, or fibrinogen concentrate, can be used to promote clot formation. Vasopressin supplementation has been proposed as a therapy to reduce blood product requirements and should be considered as the vasopressor of choice.9
Oxygen consumption/delivery curve. On the Y-axis, the VO2 consumption is represented, with a normal value ranging from 150 to 300 ml/kg/min. On the X-axis, there is DO2, which under physiological conditions is around 4-8 ml/kg/min or 800 to 1,100 ml/min. The critical DO2 is the point at which TextO2 and VO2 become dependent on DO2, entering the dependent zone where an oxygen debt occurs; at this moment, lactate levels can rise, and the CO2 gap can increase. Under aerobic metabolism conditions, VO2 can remain constant (4-8 ml/kg/min) even as DO2 decreases. Upon reaching the critical DO2, the cell adopts a predominantly anaerobic metabolism, leading to a decrease in both VO2 and TextO2 as DO2 falls. VO2: oxygen consumption. TextO2: oxygen extraction rate. DO2: oxygen delivery. Critical DO2: critical oxygen delivery.
Authorship: authors adapted from Cannon JW.9
Massive transfusion protocols should be activated early, as each minute of delay increases mortality by 5%. The decision to activate a massive transfusion protocol in the presented case was based on validated transfusion predictive scores in trauma patients. The recommended ratio of plasma, platelets, and red blood cells in trauma patients should be 1:1:1. This means one unit of plasma for every unit of red blood cells and one unit of platelets, usually available in apheresis, which is approximately equivalent to six platelet units. During massive transfusion in critically ill patients with multisystem trauma, key treatment principles have focused on controlling internal bleeding and mitigating the lethal triad: hypothermia, acidosis, and coagulopathy. Recently, the introduction of hypocalcemia has been proposed as part of this interaction of critical factors in trauma resuscitation, forming the “diamond of death.” Calcium is an important cofactor in hemostasis and coagulation, participating in key functions in bone structures, neural transmission, endocrine physiology, vascular tone control, and cardiac contractility. As hypocalcemia develops, the heart experiences electromechanical dysfunction, the QT interval prolongs, and the risk of arrhythmias increases. Additionally, hypocalcemia suppresses cardiac contractility, decreases cardiac output, alters afterload, and contributes to acute hemodynamic instability. An adequate level of serum calcium is required to maintain proper vascular tone, and it is known that hypocalcemia is associated with increased vasopressor requirements. Calcium is necessary for optimal platelet aggregation and proper functioning of factors II, VII, IX, X, and proteins C and S in the coagulation cascade. Similarly, calcium is required for fibrin formation. Therefore, it is recommended to administer one gram of intravenous calcium chloride after receiving the first four units of packed red blood cells to maintain ionized calcium concentrations above 0.9mmol/L. The citrate used as an anticoagulant in blood products can induce hypocalcemia by chelating serum calcium and exacerbating coagulopathy.9,10
ConclusionThoracic trauma associated with cardiac injuries and cardiac tamponade is a potentially life-threatening condition. Despite early diagnosis, overall survival remains anecdotal. Proper resource management, fluid resuscitation, early use of blood products, and optimal use of vasopressors and inotropes are crucial to provide a chance of survival for critically ill patients.
The success achieved in the presented case is attributed to the effective collaboration among various medical specialties. Teamwork and the use of non-technical skills influenced decision-making, allowing the execution of an emergency thoracotomy from the initial emergency care. Additionally, appropriate use of blood products was conducted through thromboelastography, guided by specialists in Critical Care and Intensive Medicine. Complications were managed through the coordinated intervention of thoracic and general surgery. Furthermore, the crucial role of the psychiatry team in managing withdrawal syndrome and initiating the patient's detoxification process is highlighted.
FinancingThe authors declare no funding.
Conflict of interestThe authors declare no conflict of interest.
Not declared.