The use of psychoactive drugs to facilitate sexual assault has acquired great relevance in recent years. The objective of this work is to help make this type of situation visible, establishing diagnostic criteria and thus being able to determine the real incidence of this type of crime.
Materials and methodsIn order to determine the frequency and characteristics of victims of sexual assault with suspected chemical submission (SSQ), a retrospective descriptive study of sexual assaults facilitated by psychoactive substances has been carried out at the Institute of Legal Medicine and Forensic Sciences of Alicante (IMLCFA) in the years 2016-2020.
ResultsAmong 702 cases studied, 95 (13,5%) met the criteria for inclusion in the probable DFSA (drug-facilitated sexual assault) group.
The profile of the victim was a woman (95,4%) around 24 years old. In most cases, the sexual violence was committed by a single male aggressor, recently met or known by the victim, and generally these events happen on weekends. The victim had voluntarily consumed alcohol, drugs or psychotropic drugs immediately before the events in most cases (88,5%). This vulnerable state of the victim was used by the aggressor to sexually assault her (opportunistic DFSA). The toxicological analyses performed on blood and/or urine were positive in 85,3%. In almost half of them (46,3%), there was more than one substance found in the toxicological analyses. The most frequent substance found were: alcohol (54,7%), cannabinoids (37,9%), benzodiazepines (22,1%), cocaine (15,8%) and ecstasy or MDMA (8,4%).
In half of the cases (50,5%), unexpected positive toxicological findings were obtained for psychoactive substances that the victim did not admit to having consumed voluntarily.
El empleo de drogas psicoactivas para facilitar una agresión sexual ha adquirido gran relevancia en estos últimos años. El objetivo del presente trabajo es ayudar a visibilizar este tipo de situaciones, estableciendo los criterios diagnósticos y así poder determinar la incidencia real de este tipo de delitos.
Material y métodosSe ha realizado un estudio descriptivo retrospectivo de las víctimas de violencia sexual mediante el empleo de sustancias psicoactivas, atendidas por los médicos forenses del Instituto de Medicina Legal y Ciencias Forenses de Alicante (IMLCFA), en los años 2016 a 2020.
ResultadosDe los 702 casos estudiados de víctimas de violencia sexual, en 95 casos (13,5%) se cumplían los criterios de sospecha de Sumisión Química (SSQ) o delitos facilitados por sustancias psicoactivas.
El perfil de la víctima es una mujer (94,7%), de edad media 24,7 años. En la mayoría de los casos la violencia sexual fue cometida por un único agresor (80,6%), varón, conocido, o recién conocido por la víctima y generalmente los hechos ocurrieron en fin de semana (54,8%).
La víctima había consumido voluntariamente alcohol solo, o en combinación con drogas y/o medicamentos, inmediatamente antes de los hechos en la mayoría de los casos (88,5%). La situación de vulnerabilidad que genera este consumo puede ser aprovechado por el agresor para agredirla sexualmente (SQ oportunista). Los análisis químico-toxicológicos de las muestras analizadas en sangre y orina fueron positivos en un 85,3% de los casos. En casi la mitad de los casos fueron positivos a más de una sustancia (46,3%). Las más frecuentes encontradas fueron: alcohol (54,7%), cannabinoides (37,9%), benzodiacepinas (22,1%), cocaína (15,8%) y éxtasis (8,4%).
En la mitad de los casos (50,5%), se obtuvieron hallazgos toxicológicos positivos inesperados de sustancias psicoactivas, que la víctima no admitía haber consumido voluntariamente.
The use of psychoactive substances to facilitate sexual assault has become highly relevant in recent years. The term suspected chemical submission (SCS) was coined in 1982 to cover all types of crimes with reference to the administration to an individual of substances with psychoactive effects for criminal purposes.
The majority of these cases are associated with crimes against sexual freedom. The term sexual violence refers to opportunistic chemical submission (CS), in those cases when the aggressor takes advantage of the victim’s vulnerable situation due to the voluntary consumption of substances which cause sedation, amnesia and disinhibition; and premeditated or proactive CS, when the aggressor administers an incapacitating or disinhibiting substance to the victim without their knowledge or consent.1
The groups of substances associated with CS can be classified as: those which have depressive effects on the central nervous system (CNS), which cause somnolence and incapacitate the victim so that they cannot respond to sexual assault or any other type of violence, and stimulants, which bring about the disinhibition of the victim, leading to risk behaviours.
This work consists of a study of the cases of sexual assault using psychoactive substances registered in Alicante Legal Medicine and Forensic Science Institute (IMLCFA) during the years 2016 to 2020. This work aims to help make situations of this type more visible, establishing diagnostic criteria and thereby enabling determination of the real incidence of crimes of this type.
Material and methodsA descriptive retrospective study was undertaken of the victims of sexual violence using psychoactive substances and seen by IMLCFA forensic doctors, in the period from 1 January 2016 to 31 December 2020.
The sources of information used were the documentation contained in the clinical history: the forensic medical report and the standardized IMLCFA document used to record data in the forensic medicine protocol in cases of crimes against sexual freedom2 and its subsequent modifications;3 this is in accordance with the new Forensic Medicine Protocol.4
Exclusion criteriaSome cases were considered to be doubtful, due to the lack of available information about the circumstances surrounding the facts, the victim’s description, the symptoms, a lack of information in the clinical history, or the absence of toxicological studies. These factors led cases to be excluded from the group of SCS and rejected.
Inclusion criteriaThe cases were reviewed by 2 researchers who applied the SCS inclusion criteria, based on some of the signs described by Du Mont et al.5,6 (Table 1), as well as having the results of the clinical history, the victim’s description of the events and the toxicological results.
Signs of suspected chemical submission (SCS).
| Signs of suspected drug-facilitated sexual assault (DFSA) |
| Symptoms of an excessive hang-over, given the substances that the victim had consumed |
| Acts performed by the victim that fit neither with their personality nor with their previous consumption |
| Disinhibition |
| Reduced judgement |
| Total or partial amnesia |
| Loss of consciousness |
| Delirium or hallucinatory state |
| Dizziness |
| Slurred speech |
| Confusion |
| Somnolence |
| Nausea or vomiting |
| Blurred vision |
Adapted from Du Mont et al.5
The sociodemographic data were analysed, together with the medical history, the circumstances of the events, the type of sexual assault and the previous voluntary consumption of substances. A study of biological samples was also requested to search for semen in the swabs and/or the victim’s clothing, as well as the toxicological blood, urine and hair analysis. The results are shown comparing both groups in terms of the use of psychoactive substances (SCS) and the non-use of drugs (Non-SCS).
Studies of the samples were performed in the National Institute of Toxicology and Forensic Science (INTCF), Barcelona, by gas chromatography with head space and flame ionization detector (FID) to determine ethyl alcohol. The general investigation into drugs of abuse and psychoactive drugs was performed using homogeneous enzyme immunoassay and processing by solid-phase extraction, mass gas-spectrometry for the study of drugs of abuse and psychoactive drugs. Moreover, since 2018 highly sensitive liquid chromatography apparatus has been available, coupled to a high resolution mass detector that is able to detect concentration of the order of ug/l. This thereby corresponds to the assay detection limits proposed by the international standards for cases of DFSA.7 The analysis included alcohol, drugs of abuse and pharmaceuticals.
The biological studies consisted of the determination of the prostatic specific antigen (PSA) using immunochromatographic analysis, and the presence of sperm was determined by microscopic observation. Cases were considered positive when PSA and/or sperm was present.
The resulting information was analysed using version 15-0 of the SPSS statistical programme for Windows. A descriptive analysis was undertaken of all the variables.
ResultsSample selectionOf the 702 cases studied, 95 (13.5%) fulfilled the criteria for inclusion in the SCS group. 24 other cases (3.4%) did not meet all of the inclusion criteria, so that they were considered to be doubtful CS and were ruled out.
Victim profileThe majority of the victims were women, and only 5 cases were men. The majority of victims were Spanish (60.2%). They were aged from 10 to 51 years old. In our study, and significantly (P <.01), psychoactive substances (SCS) were used the most in the 18-27 year-old age group (52.6%), followed by the group of those under the age of 18 years (20%).
Personal historySome of the victims with SCS (16.5%) had a history of mental illness, drug addiction (1.8%) or both (3.4%), although these results were not significant. At the moment the events occurred 8 cases were taking prescribed psychoactive medication (benzodiazepine and antidepressants), although these were not found to be statistically significant.
Alcohol was the substance consumed voluntarily the most often by the victim, in 84 cases (88.5%), alone in 62 cases, or in combination with drugs of abuse in 22 cases. These results were found to be statistically significant (P < .01) (Table 2).
Characteristics of the victims and circumstances of the sexual assault in connection with the suspicion of chemical submission (SCS) and with no suspicion of chemical submission (Non-SCS).
| Variables | Total | SCS | Non-SCS | P |
|---|---|---|---|---|
| N (%) | 702 (100) | 95 (13.5) | 607 (86.5) | |
| Victim profile | ||||
| Sex: female, n (%) | 702 (100) | 90 (94.7) | 562 (92.6) | .45 |
| Nationality: Spanish, n (%) | 690 (98.3) | 56 (60.2) | 333 (55.8) | .42 |
| Age in years: average: 24.7 | 699 (99.6) | |||
| 18-27 years, n (%) | 50 (52.6) | 142 (23.5) | <.01 | |
| Personal history | 618 (88) | .80 | ||
| Mental illness, n (%) | 12(14) | 90 (16.9) | ||
| Empty Cell | ||||
| Previous voluntary consumption of alcohol or substances | 654 (92.2) | <.01 | ||
| Alcohol n (%) | 62 (65.3) | 183 (32.7) | ||
| Drugs of abuse n (%) | 2 (2.1) | 13 (2.3) | ||
| Combination of substances n (%) | 22 (23.2) | 43 (7.7) | ||
| Temporal-spatial context | ||||
| Months of the year: January and December n (%) | 697 (99.3) | 23 (24.2) | 80 (13.3) | .45 |
| Day of the week: Saturday and Sunday n (%) | 693 (98.7) | 52 (54.8) | 218 (36.4) | .017 |
| Time of events: 0-6h, n (%) | 491 (69.9) | 66 (77.6) | 216 (53.2) | <.01 |
| Location of assault: | 665 (94.7) | <.01 | ||
| Aggressor’s home n (%) | 35 (36.8) | 199 (34.9) | ||
| Leisure premises n (%) | 25 (26.3) | 38 (6.7) | ||
| Public highway n (%) | 22 (23.2) | 123 (21.6) | ||
| Aggressor profile | ||||
| No. of aggressors: one n (%) | 636 (90.6) | 58 (80.6) | 503(89.2) | .10 |
| Relationship with the victim | 643 (91.6) | <.01 | ||
| Known, n (%) | 33 (41.3) | 358 (63.6) | ||
| Recently met, n (%) | 24 (30) | 90 (16) | ||
| Type of sexual behaviour | 586 (83.4) | .03 | ||
| Vaginal penetration n (%) | 18 (46.2) | 233 (46.2) | ||
| Penetration in more than one way n (%) | 10 (25.6) | 101 (18.5) | ||
| Time from the events to FM examination (hrs.) | 473 (67.4) | .15 | ||
| <12 hrs. n (%) | 40 (47.6) | 202 (51.9) | ||
| 12-24 hrs. n (%) | 26 (31) | 72 (18.5) |
P: statistical significance (Chi-squared test)
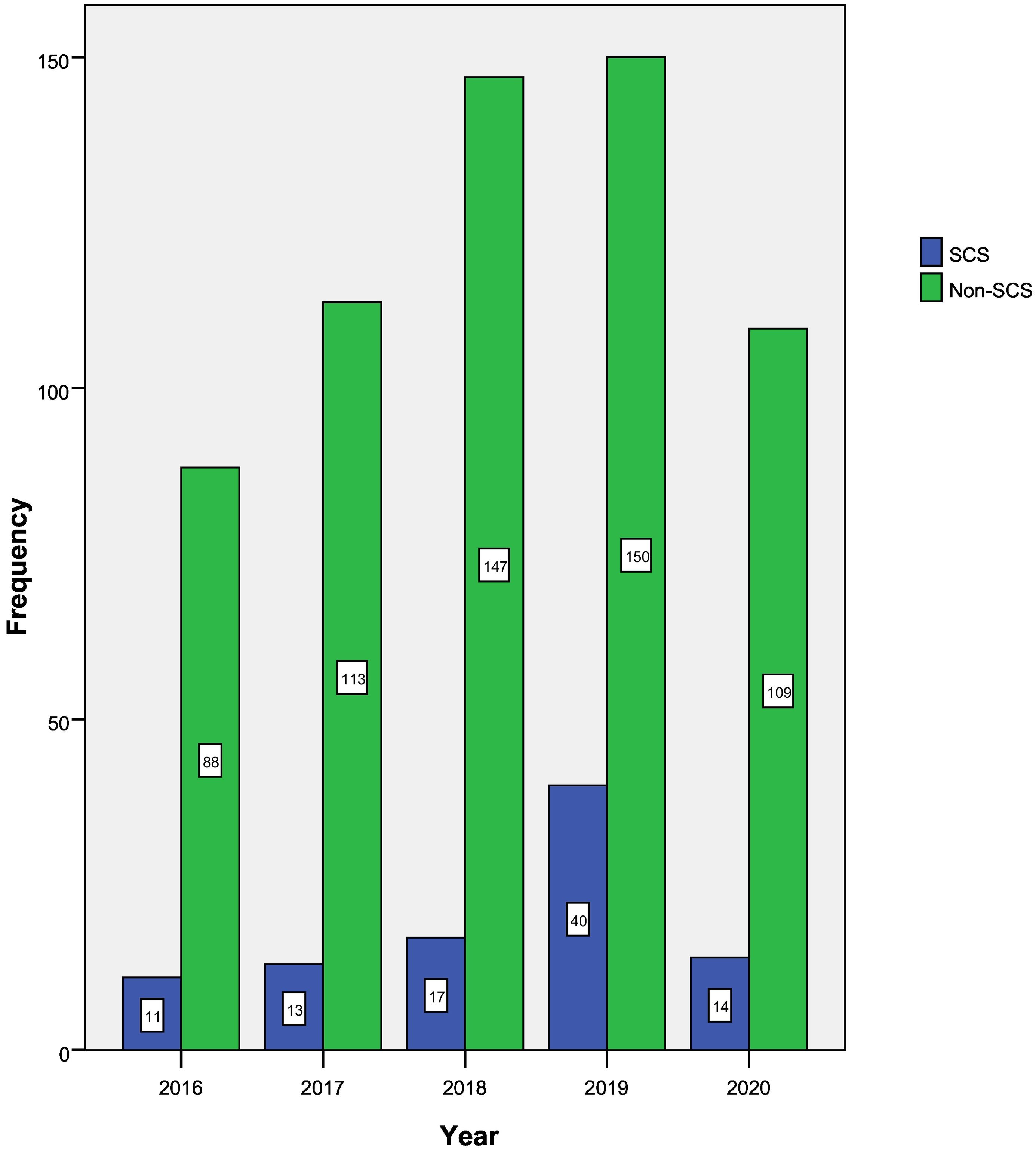
As was the case with the other crimes against sexual freedom included in our study, the number of cases of sexual assault using CS has increased over the years: 2016, 11 cases (11.6%); 2017, 13 cases (13.7%); 2018, 17 cases (17.9%); 2019 was the year with the highest incidence, with 40 cases (42.1%). The number of cases fell to 14 in 2020 (14.7%), very probably due to the COVID-19 pandemic (P = .01) (Fig. 1).
The highest frequency of sexual assault using psychoactive substances (SCS) occurred during the third quarter of the year, with 31 cases (32.6%). In terms of the months of the year, we found the 2 highest incidences in the months of December-January (24.2%), and July-August (23.2%). Sexual assault using psychoactive substances (SCS) occurred the most often, with statistical significance (P = .01) during the weekend: Saturday with 28 cases (29.5%), and Sunday with 24 cases (25.3%). They basically occurred after midnight (0-6 hrs.), with 66 cases (77.6%), followed at some distance by the evening-night (18-24 hrs.) with 14 cases (16.5%), (P < .01).
35 cases (36.8%) of the victims of SCS took place in the aggressor’s home, followed by leisure premises with 25 cases (26.3%), and the public highway, 22 cases (23.2%), showing statistical significance (P < .01).
In the majority of cases (78.6%) the time which passed after the events until the examination and sample-taking was < 24 hours (Table 2).
Aggressor profileThe majority of sexual assaults using psychoactive substances (SCS) were committed by a single aggressor (80.6%), who was known to or had recently met the victim (Table 2). When a possible family tie was analysed, in one case the aggressor was found to be the father of the victim (P = .01) (Table 2).
Analytical resultsBiological results. A biological study was performed in 78 cases using swabs, and in 16 further cases the clothing worn by the victim was also studied (P < .01). The result was positive for semen and/or PSA in the victims with SCS in 56 cases (74.7%) and in the non- SCS victims in 232 cases (64.4%), although no statistically significant differences were found between both groups.
Chemical-toxicological results. A chemical-toxicological study was performed in a total of 95 cases: blood and urine samples were taken in 57 cases, with only a urine sample in 25 cases, followed by only a blood sample in 10 cases. In 3 cases a sample of hair was taken together with a blood or urine sample was taken.
The toxicological results of the victims with SCS were as follows:
Alcohol: alone or in combination, this was the substance found the most often in the blood and/or urine tests, in 52 cases (54.7%) (P = .5).
Drugs of abuse: positive results in decreasing order were found for cannabinoids in 36 cases (37.9%), cocaine and metabolites in 15 cases (15.8%), ecstasy or MDMA in 8 cases (8.4%), followed by opiates in 4 cases (4.2%).
Psychoactive pharmaceuticals: the pharmaceuticals with psychoactive effects that were found in the toxicological studies were: benzodiazepines; antidepressant drugs; antipsychotic drugs; antihistamines and antiepileptic drugs.
The 3 drugs implicated in SCS victims were, in decreasing order: benzodiazepines in 21 cases (22.1%), followed by antidepressant drugs in 6 cases (6.3%) and antihistamines in 3 cases (3.1%).
Combinations of substances: alcohol was found together with drugs of abuse or medicines in 42 cases (44.2%).
Positive results were obtained for one substance in 37 cases, 2 substances in 22 cases, 3 substances in 12 cases, and more than 3 substances in 11 cases (Table 3).
Chemical-toxicological results in blood and/or urine in the cases with SCS and non- SCS.
| Ch-T results | SCS | Non-SCS | Total |
|---|---|---|---|
| Negative | 14 (14.7%) | 11 (24.4%) | 25 (17.9%) |
| Alcohol | 21 (22.1%) | 9 (20%) | 30 (21.4%) |
| Drugs of abuse | 11 (11.6%) | 3 (6.7%) | 14 (10%) |
| Medicines | 7 (7.4%) | 5 (11.1%) | 12 (8.6%) |
| Combinations of substances | 42 (44.2%) | 17 (37.8%) | 59 (42.1%) |
| Total | 95 (100%) | 45 (100%) | 140 (100%) |
(P = .52).
The chemical-toxicological results were negative in the 3 cases in which hair was analysed.
In the cases of SCS, when more time passed between the events and the taking of samples, the percentage of positive results for alcohol, drugs of abuse and psychoactive drugs fell: the number of positive cases for alcohol after less than 12 hrs was 12 cases; after more than 48 hours there was one case; the number of positive cases for a combination of substances studied in less than 12 hrs amounted to 20 cases; after more than 48 hours there were no cases.
Unexpected toxicological results. Unexpected toxicological results were obtained for substances which the SCS victim did not admit they were taking under prescription or had consumed voluntarily in 48 cases (50.5%). These results were found to be statistically significant (P < .01), and they are shown in Table 4.
Findings of unexpected substances in the blood and urine in cases of SCS and non-SCS cases.
| Unexpected substances in blood and/or urine | SCS | Non-SCS |
|---|---|---|
| Cannabinoids | 18 | 2 |
| Benzodiazepines | 15 | 5 |
| Cocaine | 11 | 1 |
| Ecstasy | 8 | 0 |
| Opiates | 4 | 2 |
| Antidepressant drugs | 4 | 3 |
| Antihistamines | 3 | 1 |
| Alcohol | 2 | 1 |
| Antiepileptic drugs | 2 | 2 |
| Methamphetamine | 2 | 1 |
| Bufotenine | 1 | 0 |
(P < .01).
Of the 702 cases studied of sexual assault victims, 95 cases (13.5%) fulfilled the criteria for SCS. This figure is similar to those offered by many authors, such as Anderson et al., (15%),8 although it is lower than the figures given by Du Mont (21%)9 or Xifró-Collsamata et al. (30.7%).10
In the same way as in other studies11,12 the majority of the victims with SCS were women (94.7%), and their average age was 24.7 years.
The months of the year with the highest number of cases of victims with SCS were December-January (24.2%), followed by the summer months (July-August [23.2%]), and during the weekend (Saturday and Sunday).5 In one quarter of the cases in our study the sexual assault took place in leisure premises. It is striking that a far lower proportion of cases without the suspicion of CS took place in leisure premises (6.7%). This may be explained because this type of sexual violence using psychoactive substances is strongly associated with leisure time and recreational activities, as was described by Xifró-Collsamata et al.10
Many published studies state that in cases of SCS there is a longer delay to reporting the crime than is the case with other types of sexual assault. This is explained by the fact that the substances used leave the victim unable to ask for help.5 Nevertheless, unlike these authors, our work found that a medical examination took place in 78.6% of the group with SCS within the first 24 hrs, and that there was no delay in reporting the crime, as is the case in descriptions by other authors.5,13,14 Furthermore, no significant differences were found in this respect between the groups with and without SCS.
As was the case for the report by Anderson et al.,8 the great majority of cases with SCS in our work had consumed alcohol voluntarily immediately before the events, either alone or combined with drugs of abuse and/or psychoactive drugs (88.5%). This differed from when the sexual assault had not taken place under the influence of psychoactive substances (non-SCS), in which fewer than half of the victims admitted having consumed alcohol voluntarily (39.7%). The assailant may take advantage of the increased vulnerability of the victim to sexually assault them (opportunist CS), or to surreptitiously administer other psychoactive substances (proactive CS).
We obtained positive results in 85.3% of cases in the chemical-toxicological analysis of samples from the victims with SCS. This result is similar to the one obtained by García Caballero et al. (85.5%).15 Almost half (46.3%) of the cases were positive for more than one substance.8,16 In decreasing order, the 5 substances found the most often were alcohol (54.7%), cannabinoids (37.9%), benzodiazepines (22.1%), cocaine (15.8%) and MDMA (8.4%), which is similar to the findings in other studies.17
Similarly to other authors,11,13,14,17 we found in our study that in cases with SCS, the percentage of positive results for alcohol and drugs of abuse falls with increasing periods of time between the events and sample taking.
Consuming several psychoactive substances increases their effects and exposes victims to situations in which they are defenceless, as this reduces their ability to freely react and make decisions. In the same way as other authors,12,14,18,19 we found that the most common combination of substances found consisted of alcohol and cannabinoids, with 18 cases, followed by alcohol and benzodiazepines, with 12 cases.
In half of the cases of victims with SCS (50.5%) unexpected toxicological results were obtained for psychoactive substances which the victim did not admit having taken as a medical treatment or voluntarily consumed. This result is similar to the one obtained by Du Mont et al. (48.9%).9 Although some of these cases may be included in the group of proactive CS, it is not possible to rule out the possibility that the victim either did not remember or did not wish to admit having voluntarily consumed medicines or illegal drugs. Nor can the possibility that the victim had been sold a different drug when they thought they had purchased a specific substance be ruled out. The 7 unexpected substances found the most often are, in decreasing order, cannabinoids (16 cases), benzodiazepines (14) cocaine (10), ecstasy or MDMA (8), opiates (4), antidepressant drugs (3) and antihistamines (3). These findings are similar to those of other authors.9 It is striking that alcohol was only found unexpectedly in 2 cases, combined with other drugs or psychoactive medicines.
The following substances stand out among the ones involved most often in cases of CS:
Ethyl alcoholAlcohol was the substance found the most frequently in the toxicological results of victims with SCS, alone or in combination (54.7%). This finding agrees with those of the majority of studies, which find a prevalence of 40%-70%.5,8,14 Alcohol is habitually consumed during night-time leisure, which is where these crimes occur the most often. Alcohol depresses the CNS, and in combination with other psychoactive substances such as the benzodiazepines, it may amplify their effects and increase the vulnerability of the victim to sexual assault. We found fewer positive results for alcohol in victims with SCS (54.7%) when they were compared with the frequency with which the victim admitted having voluntarily consumed alcohol prior to the events (88.5%). This may be due to the rapid metabolism of this substance (< 15 mg/dl/h) and the delay in taking samples.
CannabinoidsCannabinoids are the drugs of abuse we found the most often (37.9%). The corresponding figures for other authors vary from 0.6% to 33.7%.11,12,20 The high incidence we found may be because it is a widely used recreational drug in leisure environments, together with other substances which aid socialization and interpersonal contact, so that victims may have smoked cannabis voluntarily in a party or gathering. Nevertheless, as cannabis is available in a wide range of forms, nor can the possibility be ruled out that the assailant had administered it without the victim knowing, consuming it in a food, for example.
BenzodiazepinesAs occurs in other published studies,15,20 we found a high prevalence of benzodiazepines in our study (22.1%), which is slightly higher than the figure obtained by Fiorentin et al. (21%).12
The benzodiazepines meet most of the criteria for the so-called “rape drugs”. They are easy to obtain, given that they are used widely everywhere, they produce sedation and reduce awareness, and they also induce anterograde amnesia.
We found the following benzodiazepines in the victims with SCS in our study: diazepam, midazolam, lorazepam, alprazolam, nordazepam, clonazepam and bromazepam. We did not find flunitrazepam (Rohipnol®) in any case, even though this drug is described in the literature as used in CS.12 Nor did we find benzodiazepine analogues such as zolpidem, which was often found in other European studies.17
StimulantsAlthough the substances associated the most often with CS are those that have a depressor effect on the CNS, such as alcohol and the benzodiazepines, other stimulant drugs associated with these crimes were also found, including cocaine10,13 and amphetamines.10 These substances are often consumed together with alcohol for recreational purposes. Cocaine and amphetamines produce euphoria, disinhibition and increased libido, so that they make the victim more receptive to having sexual relations. They may also facilitate the administration of other substances.
Other substancesOther psychoactive substances have also been associated with CS, including antidepressants,13,18 opiates,20 antipsychotic drugs,10,20,21 antihistamines18,20 and antiepileptic drugs.12,21 In our study we found antidepressants in 6.3% of cases (mirtazapine, sertraline, trazodone, citalopram and fluoxetine). In 3 cases the victim did not admit to having taken these voluntarily.
Other substances which were found, although to a lesser extent than the ones mentioned above, are opiates (morphine, tramadol), antipsychotics (risperidone, quetiapine); antihistamines (cetirizine, hydroxyzine, chlorpheniramine), and antiepileptic drugs (carbamazepine, topiramate, gabapentin).
We did not find GHB in any case, this being another drug that is considered to be a classic for CS.18
An unexpected and interesting finding consisted of one case with bufotenine. This hallucinogenic tryptamine is used in Shamanic rituals in South America. It became fashionable a few years ago in Spain to have spiritual experiences. The victim, a young woman, stated that she had been sexually assaulted by 3 men in a home during a party. Urine analysis was positive for bufotenine and benzodiazepines, which the victim stated that she had not consumed voluntarily. Unlike alcohol and benzodiazepines, bufotenine has not been associated with sexual assaults. A recently published case in Spain concerned a 54 year-old male who reported having been robbed after being given a drink which contained bufotenine.22
ConclusionsAlcohol is consumed voluntarily in contexts for leisure and enjoyment, and it was the substance found the most often in our study. It is an important factor in increasing vulnerability, as assailants may take advantage of its effects to approach a victim at a time when they are unable to freely make decisions (opportunist CS).
Unexpected positive results for psychoactive substances that the victim did not admit to having consumed voluntarily were found in half of the cases (50.5%). Some of these findings may be included within the proactive CS cases, although the possibility cannot be ruled out that the victim had forgotten or did not wish to admit consuming psychoactive substances voluntarily.
No positive results were found for GHB or other classic CS drugs such as ketamine and flunitrazepam. Apart from alcohol, the drugs found the most often in our study were cannabinoids and benzodiazepines, which are widely and easily available. Although the time that passed between the events and medical attendance was usually short, we cannot rule out the possibility that the delay in visiting a health centre and having samples taken may have prevented obtaining positive results for substances which metabolize rapidly.
It is necessary to raise the profile of this problem, to improve the response and increase the technical quality of assistance, as any delay in sample taking reduces the possibility of obtaining positive results in victims with SCS, hindering diagnosis.
We would like to thank the Chemistry Department of the National Institute of Toxicology and Forensic Science (Barcelona), for their work and professionalism.
Please cite this article as: Navarro Escayola E, Vega Vega C, Bañon González R, Sanvicens Díez N, Presencia de sustancias psicoactivas en víctimas de violencia sexual en la provincia de Alicante (España) durante los años 2016-2020. Revista Española de Medicina Legal. 2022. https://doi.org/10.1016/j.reml.2022.06.001