Patients with major depressive disorder (MDD) who require an acute course of electroconvulsive therapy (ECT) have high relapse rates. Therefore, an effective maintenance treatment strategy needs to be established. Continuation and maintenance ECT (C/M-ECT) could be an adequate treatment option, although the lack of controlled studies has led to its usefulness being questioned. This review includes a detailed description of studies on the effectiveness/efficacy of ECT in MDD. Despite their methodological limitations, the results appear to support the idea that C/M-ECT would be a safe and effective alternative, especially in patients with severe and recurrent disease. Nevertheless, more controlled studies are needed to provide new evidence and allow a more accurate assessment of the efficacy, safety and pattern of use of C/M-ECT.
La elevada tasa de recidivas en los pacientes con trastorno depresivo mayor (TDM) que han requerido un curso agudo de terapia electroconvulsiva (TEC) hace necesaria establecer una estrategia terapéutica de mantenimiento eficaz. La TEC de continuación o mantenimiento (TEC-C/M) podría constituir una opción adecuada de tratamiento a largo plazo. Sin embargo, la falta de estudios controlados ha cuestionado su utilización. En la presente revisión se ha realizado una descripción detallada de los estudios relacionados con la eficacia de la TEC-C/M en el TDM. A pesar de sus limitaciones metodológicas, estos estudios sustentan la idea de que la TEC-C/M representaría una alternativa terapéutica efectiva y segura, especialmente en los pacientes más graves y recurrentes. No obstante, son necesarios estudios controlados que aporten nuevas evidencias y permitan una evaluación más fidedigna de la eficacia, seguridad y patrón de uso óptimo del la TEC-C/M.
The efficacy of ECT in acute treatment of depressive episodes is well established and is indicated as such in the main guidelines.1–7 However, it is relevant to point out that more than 50% of the depressive patients who respond to a course of ECT, and up to 95% of patients with psychotic depression, relapse within the next 6–12 months in spite of receiving appropriate drug treatment after ECT.8–14 In this context, it has been suggested that C/M-ECT could be indicated in some of the patients who required an acute ECT course for clinical remission, just as maintenance drug treatment is indicated for the patients who have responded to drug therapy in the acute phase. In addition, some studies suggest that C/M-ECT could improve the capacity to respond to drug treatment,15,16 and even to ECT itself in later relapses,15,17 and could consequently reduce health costs.16,18,19
C/M-ECT has been used since the 1940s as a strategy to prolong the improvement obtained following an acute ECT course (“prophylactic electroshock”, “convulsion dependence”).20–25 However, the development and introduction of psychotropic drugs in the 50s brought about a drastic reduction in its use. Nevertheless, the limitations of pharmacological treatment in preventing relapses that were observed in some patients with severe MDD have helped C/M-ECT to regain force and led to a recovery of interest in its use and study in the last few years.26
Most of the studies that back the use of ECT as a continuation and maintenance treatment are based on specific cases, naturalistic studies or retrospective series and the number of controlled and randomised studies is quite small.27,28 Consequently, the indication for C/M-ECT has been discussed by some authors based on the limited data available in the literature on its long-term efficacy and safety.3 Together with the controversy as to its efficacy, the level of C/M-ECT use and the patterns of use of the technique vary widely in different countries where ECT is applied as an acute treatment.29
The American Psychiatric Association (APA)2 views ECT as a therapeutic option in its recommendations for the long-term management of patients with MDD who have responded to ECT in the acute phase and who present some of the following characteristics: (a) drug therapy has not been effective in treating the index episode or in preventing relapses, (b) drug therapy cannot be administered safely and, lastly, (c) the patient prefers ECT, agrees with receiving C/M-ECT and is capable of following the therapeutic plan with the help of others.
Our objective was to review the literature on long-term ECT efficacy and pattern of use to provide data that back the clinical professional when indicating ECT as a continuation and maintenance treatment. The APA defines continuation as treatment carried out during the 6 months following recovery from the index episode, and defines maintenance as treatment carried out after these 6 months.2 However, in the literature, we find that both terms are used indistinctly; in this article, the term C/M-ECT will be used to refer to both continuation and maintenance ECT.
MethodA review of references has been carried out in the databases PubMed, ScienceDirect and Scopus. The search terms were “continuation electroconvulsive therapy”, “maintenance electroconvulsive therapy”, “depression” and “major depressive disorder”. We took into account clinical cases, naturalistic studies, uncontrolled studies and clinical trials, as well as reviews. We also searched manually the references published in the studies reviewed. Studies with the search criteria from the 1940s up to 2011 were included. Our review has centred on obtaining data, analyses and discussions of the findings related to the efficacy and pattern of use of C/M-ECT.
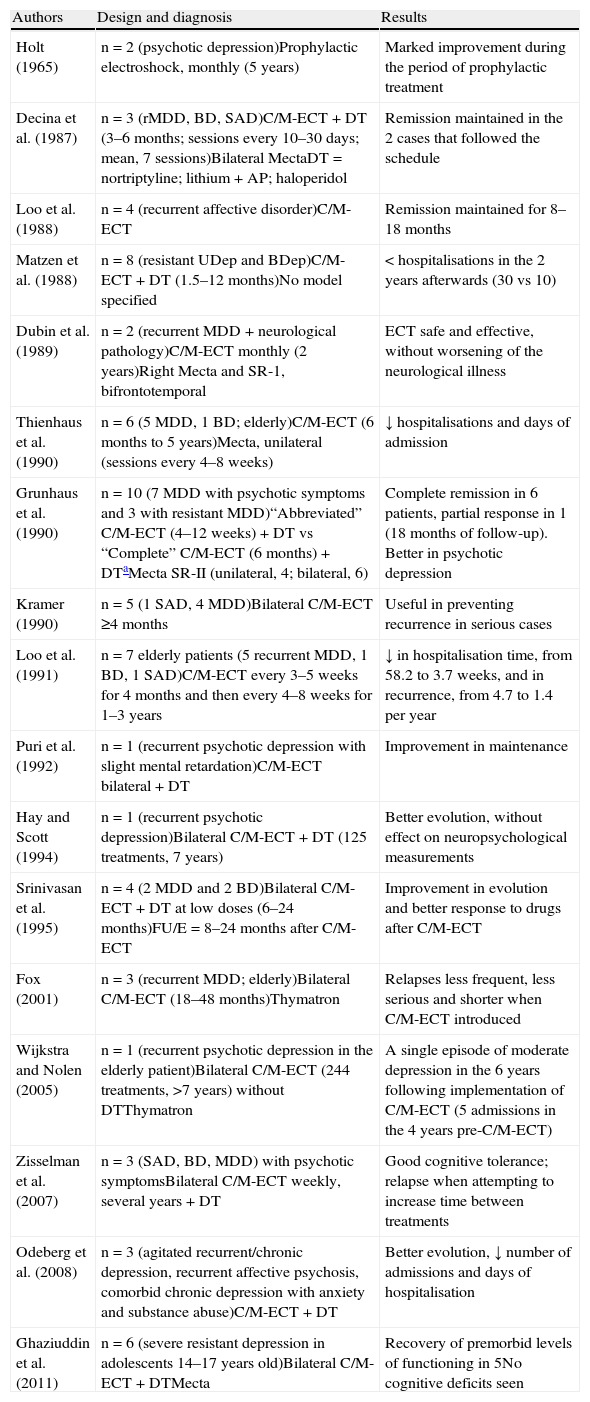
ResultsEfficacy of continuation and maintenance electroconvulsive therapy in major depressive disorderA total of 40 articles were included in the review that fulfilled the search criteria. Specifically, these were 17 cases or series of cases, 12 retrospective studies and 11 prospective studies (Tables 1–3).
Series of cases and clinical cases.
| Authors | Design and diagnosis | Results |
| Holt (1965) | n=2 (psychotic depression)Prophylactic electroshock, monthly (5 years) | Marked improvement during the period of prophylactic treatment |
| Decina et al. (1987) | n=3 (rMDD, BD, SAD)C/M-ECT+DT (3–6 months; sessions every 10–30 days; mean, 7 sessions)Bilateral MectaDT=nortriptyline; lithium+AP; haloperidol | Remission maintained in the 2 cases that followed the schedule |
| Loo et al. (1988) | n=4 (recurrent affective disorder)C/M-ECT | Remission maintained for 8–18 months |
| Matzen et al. (1988) | n=8 (resistant UDep and BDep)C/M-ECT+DT (1.5–12 months)No model specified | < hospitalisations in the 2 years afterwards (30 vs 10) |
| Dubin et al. (1989) | n=2 (recurrent MDD+neurological pathology)C/M-ECT monthly (2 years)Right Mecta and SR-1, bifrontotemporal | ECT safe and effective, without worsening of the neurological illness |
| Thienhaus et al. (1990) | n=6 (5 MDD, 1 BD; elderly)C/M-ECT (6 months to 5 years)Mecta, unilateral (sessions every 4–8 weeks) | ↓ hospitalisations and days of admission |
| Grunhaus et al. (1990) | n=10 (7 MDD with psychotic symptoms and 3 with resistant MDD)“Abbreviated” C/M-ECT (4–12 weeks)+DT vs “Complete” C/M-ECT (6 months)+DTaMecta SR-II (unilateral, 4; bilateral, 6) | Complete remission in 6 patients, partial response in 1 (18 months of follow-up). Better in psychotic depression |
| Kramer (1990) | n=5 (1 SAD, 4 MDD)Bilateral C/M-ECT ≥4 months | Useful in preventing recurrence in serious cases |
| Loo et al. (1991) | n=7 elderly patients (5 recurrent MDD, 1 BD, 1 SAD)C/M-ECT every 3–5 weeks for 4 months and then every 4–8 weeks for 1–3 years | ↓ in hospitalisation time, from 58.2 to 3.7 weeks, and in recurrence, from 4.7 to 1.4 per year |
| Puri et al. (1992) | n=1 (recurrent psychotic depression with slight mental retardation)C/M-ECT bilateral+DT | Improvement in maintenance |
| Hay and Scott (1994) | n=1 (recurrent psychotic depression)Bilateral C/M-ECT+DT (125 treatments, 7 years) | Better evolution, without effect on neuropsychological measurements |
| Srinivasan et al. (1995) | n=4 (2 MDD and 2 BD)Bilateral C/M-ECT+DT at low doses (6–24 months)FU/E=8–24 months after C/M-ECT | Improvement in evolution and better response to drugs after C/M-ECT |
| Fox (2001) | n=3 (recurrent MDD; elderly)Bilateral C/M-ECT (18–48 months)Thymatron | Relapses less frequent, less serious and shorter when C/M-ECT introduced |
| Wijkstra and Nolen (2005) | n=1 (recurrent psychotic depression in the elderly patient)Bilateral C/M-ECT (244 treatments, >7 years) without DTThymatron | A single episode of moderate depression in the 6 years following implementation of C/M-ECT (5 admissions in the 4 years pre-C/M-ECT) |
| Zisselman et al. (2007) | n=3 (SAD, BD, MDD) with psychotic symptomsBilateral C/M-ECT weekly, several years+DT | Good cognitive tolerance; relapse when attempting to increase time between treatments |
| Odeberg et al. (2008) | n=3 (agitated recurrent/chronic depression, recurrent affective psychosis, comorbid chronic depression with anxiety and substance abuse)C/M-ECT+DT | Better evolution, ↓ number of admissions and days of hospitalisation |
| Ghaziuddin et al. (2011) | n=6 (severe resistant depression in adolescents 14–17 years old)Bilateral C/M-ECT+DTMecta | Recovery of premorbid levels of functioning in 5No cognitive deficits seen |
BD: bipolar disorder; BDep: bipolar depression; C/M-ECT: continuation/maintenance ECT; DT: drug therapy (including different types of drugs and/or strategies); MDD: major depressive disorder; rMDD: recurrent major depressive disorder; SAD: schizoaffective disorder; UDep: unipolar depression.
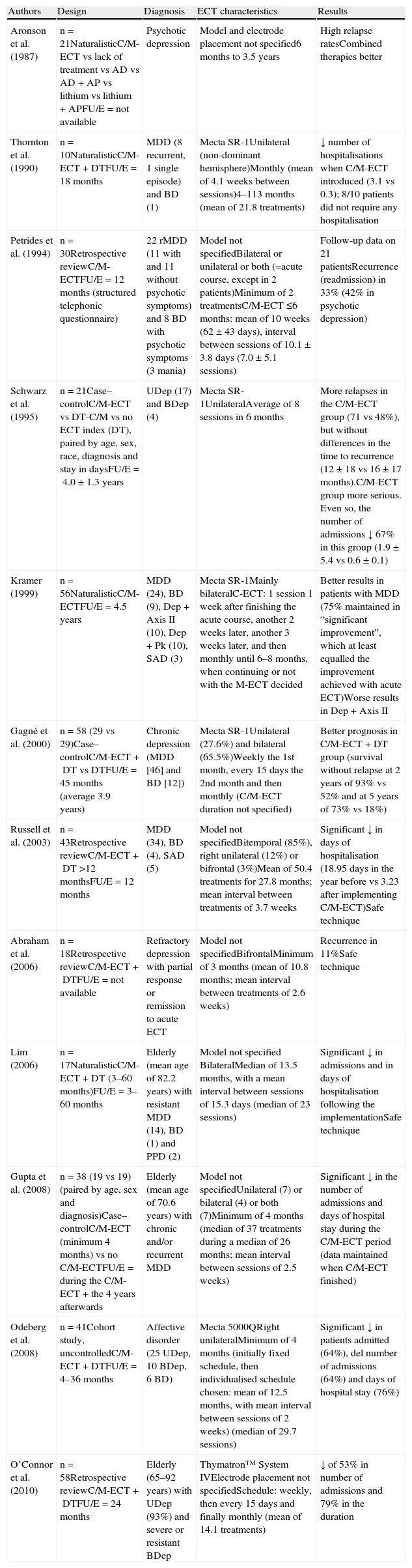
Retrospective studies.
| Authors | Design | Diagnosis | ECT characteristics | Results |
| Aronson et al. (1987) | n=21NaturalisticC/M-ECT vs lack of treatment vs AD vs AD+AP vs lithium vs lithium+APFU/E=not available | Psychotic depression | Model and electrode placement not specified6 months to 3.5 years | High relapse ratesCombined therapies better |
| Thornton et al. (1990) | n=10NaturalisticC/M-ECT+DTFU/E=18 months | MDD (8 recurrent, 1 single episode) and BD (1) | Mecta SR-1Unilateral (non-dominant hemisphere)Monthly (mean of 4.1 weeks between sessions)4–113 months (mean of 21.8 treatments) | ↓ number of hospitalisations when C/M-ECT introduced (3.1 vs 0.3); 8/10 patients did not require any hospitalisation |
| Petrides et al. (1994) | n=30Retrospective reviewC/M-ECTFU/E=12 months (structured telephonic questionnaire) | 22 rMDD (11 with and 11 without psychotic symptoms) and 8 BD with psychotic symptoms (3 mania) | Model not specifiedBilateral or unilateral or both (=acute course, except in 2 patients)Minimum of 2 treatmentsC/M-ECT ≤6 months: mean of 10 weeks (62±43 days), interval between sessions of 10.1±3.8 days (7.0±5.1 sessions) | Follow-up data on 21 patientsRecurrence (readmission) in 33% (42% in psychotic depression) |
| Schwarz et al. (1995) | n=21Case–controlC/M-ECT vs DT-C/M vs no ECT index (DT), paired by age, sex, race, diagnosis and stay in daysFU/E=4.0±1.3 years | UDep (17) and BDep (4) | Mecta SR-1UnilateralAverage of 8 sessions in 6 months | More relapses in the C/M-ECT group (71 vs 48%), but without differences in the time to recurrence (12±18 vs 16±17 months).C/M-ECT group more serious. Even so, the number of admissions ↓ 67% in this group (1.9±5.4 vs 0.6±0.1) |
| Kramer (1999) | n=56NaturalisticC/M-ECTFU/E=4.5 years | MDD (24), BD (9), Dep+Axis II (10), Dep+Pk (10), SAD (3) | Mecta SR-1Mainly bilateralC-ECT: 1 session 1 week after finishing the acute course, another 2 weeks later, another 3 weeks later, and then monthly until 6–8 months, when continuing or not with the M-ECT decided | Better results in patients with MDD (75% maintained in “significant improvement”, which at least equalled the improvement achieved with acute ECT)Worse results in Dep+Axis II |
| Gagné et al. (2000) | n=58 (29 vs 29)Case–controlC/M-ECT+DT vs DTFU/E=45 months (average 3.9 years) | Chronic depression (MDD [46] and BD [12]) | Mecta SR-1Unilateral (27.6%) and bilateral (65.5%)Weekly the 1st month, every 15 days the 2nd month and then monthly (C/M-ECT duration not specified) | Better prognosis in C/M-ECT+DT group (survival without relapse at 2 years of 93% vs 52% and at 5 years of 73% vs 18%) |
| Russell et al. (2003) | n=43Retrospective reviewC/M-ECT+DT >12 monthsFU/E=12 months | MDD (34), BD (4), SAD (5) | Model not specifiedBitemporal (85%), right unilateral (12%) or bifrontal (3%)Mean of 50.4 treatments for 27.8 months; mean interval between treatments of 3.7 weeks | Significant ↓ in days of hospitalisation (18.95 days in the year before vs 3.23 after implementing C/M-ECT)Safe technique |
| Abraham et al. (2006) | n=18Retrospective reviewC/M-ECT+DTFU/E=not available | Refractory depression with partial response or remission to acute ECT | Model not specifiedBifrontalMinimum of 3 months (mean of 10.8 months; mean interval between treatments of 2.6 weeks) | Recurrence in 11%Safe technique |
| Lim (2006) | n=17NaturalisticC/M-ECT+DT (3–60 months)FU/E=3–60 months | Elderly (mean age of 82.2 years) with resistant MDD (14), BD (1) and PPD (2) | Model not specified BilateralMedian of 13.5 months, with a mean interval between sessions of 15.3 days (median of 23 sessions) | Significant ↓ in admissions and in days of hospitalisation following the implementationSafe technique |
| Gupta et al. (2008) | n=38 (19 vs 19) (paired by age, sex and diagnosis)Case–controlC/M-ECT (minimum 4 months) vs no C/M-ECTFU/E=during the C/M-ECT+the 4 years afterwards | Elderly (mean age of 70.6 years) with chronic and/or recurrent MDD | Model not specifiedUnilateral (7) or bilateral (4) or both (7)Minimum of 4 months (median of 37 treatments during a median of 26 months; mean interval between sessions of 2.5 weeks) | Significant ↓ in the number of admissions and days of hospital stay during the C/M-ECT period (data maintained when C/M-ECT finished) |
| Odeberg et al. (2008) | n=41Cohort study, uncontrolledC/M-ECT+DTFU/E=4–36 months | Affective disorder (25 UDep, 10 BDep, 6 BD) | Mecta 5000QRight unilateralMinimum of 4 months (initially fixed schedule, then individualised schedule chosen: mean of 12.5 months, with mean interval between sessions of 2 weeks) (median of 29.7 sessions) | Significant ↓ in patients admitted (64%), del number of admissions (64%) and days of hospital stay (76%) |
| O’Connor et al. (2010) | n=58Retrospective reviewC/M-ECT+DTFU/E=24 months | Elderly (65–92 years) with UDep (93%) and severe or resistant BDep | Thymatron™ System IVElectrode placement not specifiedSchedule: weekly, then every 15 days and finally monthly (mean of 14.1 treatments) | ↓ of 53% in number of admissions and 79% in the duration |
AD: antidepressant; AP: antipsychotic; Axis II: disorder codified in Axis II of the DSM-IV-TR; BD: bipolar disorder; BDep: bipolar depression; C/M-ECT: continuation/maintenance ECT; Dep: depression; DT: drug treatment (including different types of drugs and/or strategies); FU/E: length of follow-up or data as to the evolution in that period of time; MDD: major depressive disorder; Pk: Parkinson's disease; PPD: primary psychotic disorder; rMDD: recurrent major depressive disorder; SAD: schizoaffective disorder; UDep: unipolar depression.
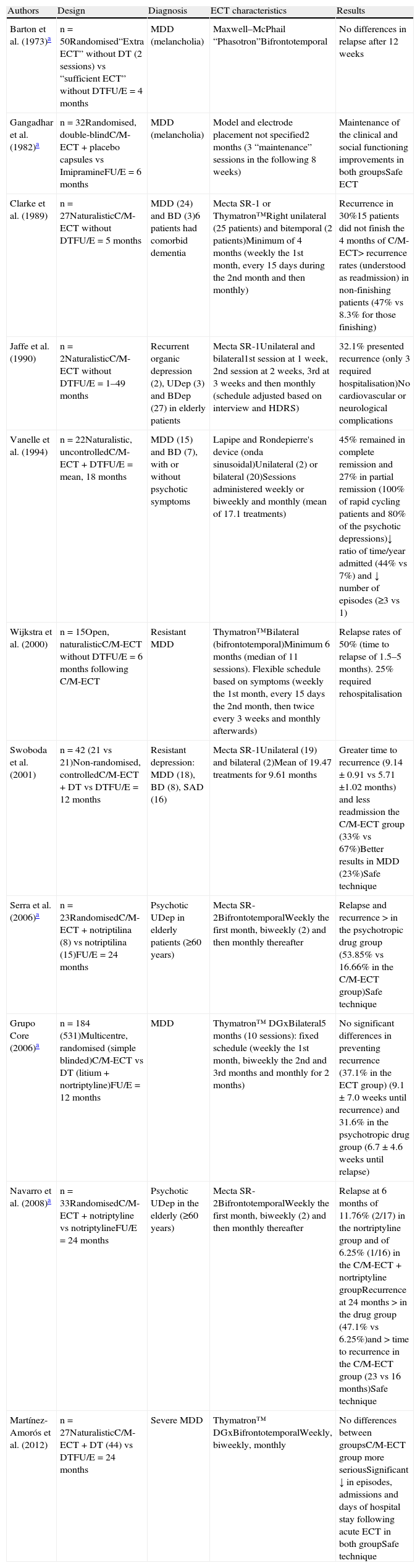
Prospective studies.
| Authors | Design | Diagnosis | ECT characteristics | Results |
| Barton et al. (1973)a | n=50Randomised“Extra ECT” without DT (2 sessions) vs “sufficient ECT” without DTFU/E=4 months | MDD (melancholia) | Maxwell–McPhail “Phasotron”Bifrontotemporal | No differences in relapse after 12 weeks |
| Gangadhar et al. (1982)a | n=32Randomised, double-blindC/M-ECT+placebo capsules vs ImipramineFU/E=6 months | MDD (melancholia) | Model and electrode placement not specified2 months (3 “maintenance” sessions in the following 8 weeks) | Maintenance of the clinical and social functioning improvements in both groupsSafe ECT |
| Clarke et al. (1989) | n=27NaturalisticC/M-ECT without DTFU/E=5 months | MDD (24) and BD (3)6 patients had comorbid dementia | Mecta SR-1 or Thymatron™Right unilateral (25 patients) and bitemporal (2 patients)Minimum of 4 months (weekly the 1st month, every 15 days during the 2nd month and then monthly) | Recurrence in 30%15 patients did not finish the 4 months of C/M-ECT> recurrence rates (understood as readmission) in non-finishing patients (47% vs 8.3% for those finishing) |
| Jaffe et al. (1990) | n=2NaturalisticC/M-ECT without DTFU/E=1–49 months | Recurrent organic depression (2), UDep (3) and BDep (27) in elderly patients | Mecta SR-1Unilateral and bilateral1st session at 1 week, 2nd session at 2 weeks, 3rd at 3 weeks and then monthly (schedule adjusted based on interview and HDRS) | 32.1% presented recurrence (only 3 required hospitalisation)No cardiovascular or neurological complications |
| Vanelle et al. (1994) | n=22Naturalistic, uncontrolledC/M-ECT+DTFU/E=mean, 18 months | MDD (15) and BD (7), with or without psychotic symptoms | Lapipe and Rondepierre's device (onda sinusoidal)Unilateral (2) or bilateral (20)Sessions administered weekly or biweekly and monthly (mean of 17.1 treatments) | 45% remained in complete remission and 27% in partial remission (100% of rapid cycling patients and 80% of the psychotic depressions)↓ ratio of time/year admitted (44% vs 7%) and ↓ number of episodes (≥3 vs 1) |
| Wijkstra et al. (2000) | n=15Open, naturalisticC/M-ECT without DTFU/E=6 months following C/M-ECT | Resistant MDD | Thymatron™Bilateral (bifrontotemporal)Minimum 6 months (median of 11 sessions). Flexible schedule based on symptoms (weekly the 1st month, every 15 days the 2nd month, then twice every 3 weeks and monthly afterwards) | Relapse rates of 50% (time to relapse of 1.5–5 months). 25% required rehospitalisation |
| Swoboda et al. (2001) | n=42 (21 vs 21)Non-randomised, controlledC/M-ECT+DT vs DTFU/E=12 months | Resistant depression: MDD (18), BD (8), SAD (16) | Mecta SR-1Unilateral (19) and bilateral (2)Mean of 19.47 treatments for 9.61 months | Greater time to recurrence (9.14±0.91 vs 5.71±1.02 months) and less readmission the C/M-ECT group (33% vs 67%)Better results in MDD (23%)Safe technique |
| Serra et al. (2006)a | n=23RandomisedC/M-ECT+notriptilina (8) vs notriptilina (15)FU/E=24 months | Psychotic UDep in elderly patients (≥60 years) | Mecta SR-2BifrontotemporalWeekly the first month, biweekly (2) and then monthly thereafter | Relapse and recurrence > in the psychotropic drug group (53.85% vs 16.66% in the C/M-ECT group)Safe technique |
| Grupo Core (2006)a | n=184 (531)Multicentre, randomised (simple blinded)C/M-ECT vs DT (litium+nortriptyline)FU/E=12 months | MDD | Thymatron™ DGxBilateral5 months (10 sessions): fixed schedule (weekly the 1st month, biweekly the 2nd and 3rd months and monthly for 2 months) | No significant differences in preventing recurrence (37.1% in the ECT group) (9.1±7.0 weeks until recurrence) and 31.6% in the psychotropic drug group (6.7±4.6 weeks until relapse) |
| Navarro et al. (2008)a | n=33RandomisedC/M-ECT+notriptyline vs notriptylineFU/E=24 months | Psychotic UDep in the elderly (≥60 years) | Mecta SR-2BifrontotemporalWeekly the first month, biweekly (2) and then monthly thereafter | Relapse at 6 months of 11.76% (2/17) in the nortriptyline group and of 6.25% (1/16) in the C/M-ECT+nortriptyline groupRecurrence at 24 months > in the drug group (47.1% vs 6.25%)and > time to recurrence in the C/M-ECT group (23 vs 16 months)Safe technique |
| Martínez-Amorós et al. (2012) | n=27NaturalisticC/M-ECT+DT (44) vs DTFU/E=24 months | Severe MDD | Thymatron™ DGxBifrontotemporalWeekly, biweekly, monthly | No differences between groupsC/M-ECT group more seriousSignificant ↓ in episodes, admissions and days of hospital stay following acute ECT in both groupSafe technique |
BD: bipolar disorder; C/M-ECT: continuation/maintenance ECT; DT: drug therapy (including different types of drugs and/or strategies); FU/E: length of follow-up or data as to the evolution in that time period; MDD: major depressive disorder; SAD: schizoaffective disorder.
In the literature we found 17 articles that included clinical cases and series of cases (Table 1) that back the efficacy and safety of C/M-ECT at the clinical level as a therapeutic tool for preventing relapse in MDD,16,17,30–43 even in adolescents.44
Retrospective studiesWe reviewed 12 retrospective studies. The specifications of each of them and the data as to the sample characteristics and ECT application can be found in Table 2.
Of these 12 retrospective studies, C/M-ECT was combined with psychotropic drugs in 7,39,45–50 while in 5, either it was not combined or this aspect was not specified.8,9,29,51,52 In 8 of the studies, only the evolution of a group of patients who received C/M-ECT after the acute episode was assessed.9,39,45,47–51 In the 4 other retrospective studies, in spite of the methodological limitations inherent in this type of studies, the assessment was of C/M-ECT efficacy with respect to other continuation/maintenance treatment strategies,8,29,46,52 including lack of treatment,8,52 antidepressant alone,8,46 antidepressant plus antipsychotic,8,46 lithium alone,8,46 antidepressant plus mood stabiliser46 and lithium plus antipsychotic,8 or unspecified drug therapy.29
The potential efficacy of C/M-ECT as a maintenance treatment was presented in the 12 retrospective studies, some of which indicated recurrence rates between 11% and 33%.9,45,51 It should be pointed out that these are rates lower than those described for patients not treated with C/M-ECT after an acute course of ECT.8–14 The efficacy of C/M-ECT was also seen in the reduction of patients admitted,39,50 the number of admissions29,39,47,48,50,52 and the days of hospitalisation after the establishment of C/M-ECT.39,47–49,52
The efficacy of the technique was subject to different considerations in 3 of the studies reviewed.9,29,46 Aronson et al.8 found a very high recurrence rate in the C/M-ECT group (95.2%) and suggested that C/M-ECT without being combined with drugs did not show any special efficacy in preventing relapse. However, these same authors suggested that the relapse rate was lowered when a combined therapeutic strategy was used and, in this sense, they emphasised the need to perform further studies with combined treatments, especially with ECT. Schwarz et al.29 found higher relapse rates in the C/M-ECT group (71 vs 48%); however, they concluded that the group treated with C/M-ECT was more severe. Perhaps the results that were most clearly favourable to C/M-ECT combined with psychotropic drugs, with respect to long-term drug therapy, were those indicated by Gagné et al.46 They found a probability for survival without recurrence at 2 years of 93% against 52%, and without recurrence at 5 years of 73% against 18%, always in favour of C/M-ECT associated with psychotropic drugs.
The profile of patients for whom C/M-ECT was indicated was analysed in some of the retrospective studies review. Thornton et al.50 reported that this treatment was indicated more frequently for patients over 60 years old, for those with psychotic depression and/or depressive pseudodementia and for those with a history of poor response to or lack of tolerance to drugs. Schwarz et al.29 found that C/M-ECT was indicated in patients who were clinically more severe, in whom pharmacotherapy had failed.
Some authors assessed C/M-ECT efficacy in specific subpopulations. Petrides et al.9 reported a relapse rate in patients with psychotic depression (42%) lower than those obtained with continuation drug therapy in this subtype of depression (50–95%),8,11,53 suggesting that C/M-ECT could be a good strategy for this subtype of especially serious patients. Kramer51 analysed C/M-ECT efficacy in patients with different types of depression with comorbidity in Axis II or Axis III according to DSM-IV criteria (MDD, bipolar disorder (BD), depression associated with Axis II disorder, Parkinson's disease and schizophrenia): the best results were observed in patients with MDD and the worst results in patients with depression and comorbid Axis II disorder. Finally, in a study carried out on a very elderly population, Lim47 concluded that C/M-ECT seemed to be a safe, effective strategy, which was later replicated by other authors in later studies.48,52
With respect to the possible factors that predict recurrence following an acute course of ECT, it has been suggested8,11,53,54 that clinical aspects such as prior drug resistance, gender, seriousness of the episode and the presence of psychotic symptoms could influence posterior recurrence. However, there are very few retrospective C/M-ECT studies that analyse this question. In them, despite the examination of multiple variables, none were detected that had predictive value,9,46 with the exception of the possible protective effect of C/M-ECT itself.9
Lastly, in relation to the safety profile of C/M-ECT, from the studies reviewed,45,47,49 it could be concluded that it would constitute a relatively safe and well-tolerated strategy, even in the elderly, given that the patients did not present any serious adverse effects related with the treatment.
Prospective studiesThere were 11 prospective studies analysed. The specifications of each study and the data as to sample characteristics and ECT application are described in detail in Table 3.
Six of the prospective studies were naturalistic55–60 and the other 5 were randomised.61–65
In 3 of the naturalistic studies,55,56,60 there was an analysis of the evolution of a single group of patients for whom C/M-ECT was indicated as the only treatment, while in 1 of those studies,59 C/M-ECT was combined with psychotropic drugs. In the studies by Clarke,55 Jaffe56 and Vanelle,59 C/M-ECT efficacy was postulated as a maintenance treatment and recurrence rates of some 30% were reported. However, Wijkstra et al.60 indicated higher recurrence rates (50%), similar to those described for patients not treated with C/M-ECT following an acute course of ECT.
The remaining 2 naturalistic studies57,58 included a group of patients treated with different psychotropic drugs, and C/M-ECT was also associated with drug therapy in these studies.
The efficacy of C/M-ECT as a long-term maintenance treatment was also reflected in these studies, as lowered number of episodes,57,59 number of admissions57,58 and days of hospitalisation following C/M-ECT implementation,57,59 and improved overall patient functioning.56 Vanelle et al.59 indicated that C/M-ECT combined with psychotropic drugs was superior in reducing the number of episodes and time per admission per year. Swoboda et al.58 recorded the superiority of combined C/M-ECT over psychotropic drugs (in greater time until recurrence) and Martínez-Amorós et al.57 concluded that both psychotropic drugs and C/M-ECT combined with psychotropic drugs could be 2 strategies useful in long-term treatment for patients who required ECT in the acute episode.
Five of the 12 prospective studies were randomized61–65 and included a group of patients treated with psychotropic drugs, except for the study by Barton et al.61 It should be emphasised that the data provided by Serra et al.65 are the preliminary data from a later study.64 Only in 2 of these studies was C/M-ECT combined with drug treatment.64,65
Barton et al.61 did not find any significant differences in the number of relapses, following 12 weeks, between C/M-ECT in monotherapy and absence of treatment. However, it is important to point out that the C/M-ECT consisted of only 2 extra sessions following the recovery from the index episode. Gangadhar et al.62 did not find any differences between C/M-ECT and treatment with imipramine in 6 months of follow-up, either.
The CORE group63 carried out a randomised multicentre study on 531 patients with unipolar depression (single episode or recurrent disorder). The patients had received a course of ECT during the years 1997–2004, as treatment for the index episode. After performing a week of washing out, without any treatment, the patients who continued fulfilling remission criteria (Hamilton depression remission scale [HDRS] with 24 items [HDRS24] ≤10; n=184) were randomly assigned to a fixed C/M-ECT schedule for 5 months (total of 10 sessions) or a psychotropic drug schedule (lithium and nortriptyline at doses based on plasma levels). For the patients who finished the study (n=184), the authors found relapse rates of 37.1% in the ECT group and 31.6% in the psychotropic drug group, without finding any significant differences between the 2 treatment groups. The authors concluded that both long-term treatment strategies were, apparently, comparable in preventing relapse in severe patients with tendency to recurrence, and superior to placebo, when they compared the results with the relapse rates obtained in a previous study by Sackeim's group.14 In that study on patients who received placebo, nortriptyline, or lithium plus nortriptyline following an acute course of ECT, they found 6-month relapse rates of 84% for the placebo group, 60% for the nortriptyline group and 39% for the patients that received lithium plus nortriptyline.14 Among the limitation of the CORE group study were the loss of patients during the washing-out period, the lack of a group whose treatment was C/M-ECT associated with psychotropic drugs and the use of a fixed C/M-ECT schedule.63
Serra and Gasto65 compared the efficacy of C/M-ECT with nortriptyline with respect to a group that received only the drug. They provided initial data on 23 elderly patients with unipolar psychotic depression, and Navarro et al.64 expanded the sample assessed to 33 patients. The authors concluded that the relapse/recurrence rate, after 2 years of follow-up, was significantly greater in the group that received only nortriptyline, while the tolerability was similar in both treatment groups. Although sample size was relatively small, its homogeneity provided the results with high internal validity; this suggested that C/M-ECT could be a safe, effective alternative for this subgroup of elderly patients.
In 1 of the naturalistic studies,57 the profile of patients for whom C/M-ECT was indicated was analysed. These patients were those with a higher recurrence rate, lower age at disorder onset, greater resistance to pharmacological treatment and greater number of sessions of acute ECT. The treatment was also prescribed more often for male patients.
With respect to some specific subpopulations, the results provided in the review of prospective studies were congruent with those observed in the retrospective studies: in addition to being favourable to C/M-ECT in elderly patients,64,65 they also showed efficacy in psychotic depression,55,59,64,65 as well as in rapid cycling patients.59 Swoboda et al.58 analysed different diagnostic groups (MDD, BD and schizoaffective disorder (SAD)) separately, finding better results in the MDD group. Finally, C/M-ECT efficacy seemed lower in resistant patients.60
As for possible factors predictive of recurrence, in a single study57 the authors identified a greater duration of the index episode and a greater number of episodes in the previous 2 years as risk factors for presenting MDD recurrence following an acute course of ECT. However, Clarke et al.55 did not find any risk factors among the variables (sociodemographic and course) that they analysed. Having completed the course of C/M-ECT was, once again, the only protective factor.55
Some of these prospective studies provided data on the safety of the technique.56–58,62,64,65 The authors concluded that C/M-ECT would be a safe, well-tolerated strategy, given that it did not present serious side effects related with its use.
Pattern of use of continuation/maintenance electroconvulsive therapyThe technique of C/M-ECT is applied heterogeneously and with great variability.15 Some of the centres in which ECT is performed as an acute treatment do not have C/M-ECT programmes available. In addition, the proportion of patients for which C/M-ECT is indicated and the frequency with which the sessions varies according to the countries and the centres.15
The data published suggest that C/M-ECT is used less frequently than acute ECT, with utilisation rates that range between 14% and 25.5%.66–68 In a study carried out on a group of 86 psychiatrists in the USA with experience in using ECT, only 60% of them indicated C/M-ECT.69 In the 59 centres in New York when ECT was performed in 2001, 15.9% of the patients received C/M-ECT.67 In another study carried out in a New York centre, C/M-ECT was indicated, during a 6-year period, in only 19% of the patients who received ECT as acute treatment.9 In Norway, C/M-ECT was applied in 88% of the units that responded to a survey on the pattern of ECT use and it was indicated in 14% of the cases (60 patients from a total of 420).68 In Spain, the results obtained in 2006 showed that C/M-ECT was indicated in 16% of the patients treated with acute ECT.70 Likewise, the authors reported that in 26 psychiatric units, where ECT was applied as an acute treatment, C/M-ECT had not been indicated for any patient in 12 months.70 In a earlier study, in Barcelona, 60% of the hospitals that performed acute ECT (8/12) had a C/M-ECT programme available.71 On the other hand, in India, only 25.5% of the psychiatrists who replied to a survey by the Indian Psychiatric Society indicated C/M-ECT.66
How often the sessions should be during C/M-ECT and the duration of C/M-ECT are still not well established.28,51,72 In general, the time interval between sessions is increased after the acute ECT is finished, following a fixed or flexible schedule. In the flexible schedule, the time interval between sessions is modified based on patient symptoms and tolerance to C/M-ECT. In the fixed schedule, as the rate of sessions is predetermined, it is more difficult to detect early relapse signs and the patients can receive more sessions than necessary, a fact that can favour the appearance of undesirable effects.72
Fink73 proposes, as a possible approximation to a standard treatment schedule, 1 session a week for 3–4 weeks, 1 session every 15 days for 4 weeks and then monthly for 4–6 months more. Likewise, it would be recommendable for the patient to be totally free from symptoms for 16–26 weeks before considering the treatment finished.74,75 Along the same lines, the Spanish treatment schedule most recommended consists of performing weekly sessions during the first month, every 15 days during the second and third months and, finally, monthly.5
In the opinion of many authors, a flexible and individual schedule would be preferable, with the intervals recommended (weekly–biweekly–monthly) based on clinical evolution and side effects observed in each patient, administering the minimum number of treatments needed to achieve sustained remission.2,5,27,39,63,76 In C/M-ECT, each patient should be assessed before the beginning (basal state) and then before each treatment2 to evaluate both the clinical state as well as the appearance of possible adverse effects. It is important to point out that there is no maximum number of treatments in C/M-ECT.2 However, it is considered that the indication for C/M-ECT should be revised every 6 months.2,5
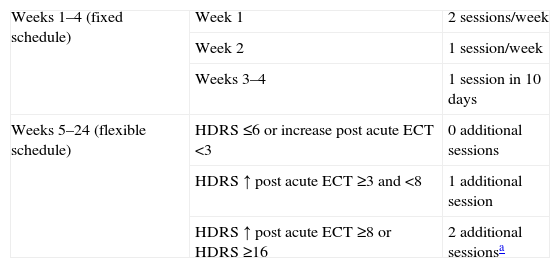
Some authors suggest using psychometric scales, especially the HDRS and mini-mental state examination (MMSE), as standardised assessment tools in these patients.56 In this sense, Lisanby et al.72 have designed an algorithm (symptom-titrated algorithm-based longitudinal ECT, STABLE) based on titrating depressive symptoms through the HDRS24 and the appearance of cognitive effects through the MMSE. The algorithm attempts to reduce the risk of relapse in the critical first month after the acute ECT and to avoid over-treatment and appearance of possible adverse effects. During the first week, the patients receive 2 sessions, 1 session in the second week and 1 session in 10 days (4 sessions in 24 days). The frequency of sessions in the following weeks (from the 5th to the 24th) is flexible (applying the algorithm): based on the weekly scores obtained in the HDRS24 and the MMSE, the patients could receive 0–2 ECT sessions in that week (Table 4). The algorithm is designed to be implemented through case management and with intensive follow-up, which includes weekly visits to detect the first symptoms of relapse and possible adverse effects (at the cognitive level), which could lead to the abandonment of the treatment. The data derived from this retrospective study suggest that this algorithm could be useful.72 However, it is an algorithm complicated to apply in standard clinical practice, given that it involves an elevated number of visits, and its usefulness should be confirmed in randomised controlled studies.
STABLE algorithm.
| Weeks 1–4 (fixed schedule) | Week 1 | 2sessions/week |
| Week 2 | 1session/week | |
| Weeks 3–4 | 1 session in 10 days | |
| Weeks 5–24 (flexible schedule) | HDRS ≤6 or increase post acute ECT <3 | 0 additional sessions |
| HDRS ↑ post acute ECT ≥3 and <8 | 1 additional session | |
| HDRS ↑ post acute ECT ≥8 or HDRS ≥16 | 2 additional sessionsa |
Long-term treatment of depressive patients who have remitted after acute ECT treatment still, even today, continues to be the subject of controversy. The current evidence C/M-ECT efficacy is based on publications that include clinical cases and series of cases, retrospective studies and prospective studies, of which 5 are randomised, a circumstance that would imply a level of evidence 1.77 Consequently, it cannot be forgotten that there are various factors that limit the overall interpretation of the results. In the first place, the methodological characteristics of most of these studies, which include small samples and use of administrative data or data taken from the case history, instead of data collected prospectively. In addition, these studies are difficult to compare for various reasons: (1) sample heterogeneity, because they include patients with MDD, BD and SAD; (2) the different characteristics of applying the technique (as far as wave type and electrode placement), plus the fact that most of the studies do not collect other technical factors that can affect therapy effectiveness, such as the charge applied or the pulse amplitude; (3) the lack of a control group in a significant number of studies; (4) the fact that the C/M-ECT is applied in monotherapy or associated with different psychotropic drugs, as well as the concomitant use of drugs (even though it is a standard clinical practice),78 could constitute a factor of confusion50; (5) the comparative studies include various types of strategies (absence of treatment, various drugs, in monotherapy or in combination or other strategies); likewise, introducing or modifying the drug schedule during the study would constitute factors that would make assessing the specific contribution of the C/M-ECT more difficult39; (6) the periods of follow-up and C/M-ECT application are very varied: and, lastly, (7) some retrospective studies included only those patients who had received C/M-ECT for a specific period of time (for example, 4 or 12 months) and excluded those who had not, a fact which could mean a bias in favour of those who responded to C/M-ECT.39,49
Despite all the limitations analysed, the data derived from our review suggest that C/M-ECT could constitute an effective therapeutic strategy in the prevention of depressive relapses after an acute course of ECT, with a level of recommendation B (recommendable treatment: at least moderate evidence that the measure is effective and that the benefits exceed the damages).77 Factors such as the reduction in relcurrence rates and in the number of episodes or hospitalisations and the improvement in overall patient functioning are measures that reflect the potential efficacy of treatment with C/M-ECT.
Information on C/M-ECT efficacy compared with other pharmacological strategies is very limited. The few studies that carry out some kind of comparative analysis obtain non-uniform results; while some suggest that C/M-ECT is more effective than psychotropic drugs,46,58,64,65 others do not obtain any differences57,61–63 and others indicate greater efficacy for the drugs.8,29 Likewise, it is noteworthy that, in approximately half of the studies (including the CORE group multicentre study63), C/M-ECT combined with psychotropic drugs is not used, despite it being a very normal strategy in clinical practice and one that has a well-established profile of tolerance and safety.78
Speaking generally, it has been suggested that C/M-ECT should be considered for those depressive patients who have responded to acute ECT and for whom drug therapy cannot be indicated or has shown its inefficiency,9,29,39,45,46,48–50,52,59 for those with a history of recurrent illness and frequent hospitalisations (especially if there are psychotic symptoms),9,50 and in elderly patients.47,48,64,65 Going beyond questions of efficacy, in all of the studies reviewed, there were no reports of any significant adverse effects; this is a fact that makes it possible to conclude that C/M-ECT is a technique that is well tolerated and that has a good safety profile, even in fragile patients of high somatic complexity.
The high relapse rate after an acute course of ECT has emphasised the need to identify possible risk factors for recurrence. Determining the presence of such risk factors in patients who have finished an acute course of ECT can help to select the candidates for receiving C/M-ECT and to plan it. Some authors suggest that greater drug resistance14,79–82 or the presence of psychotic symptoms10,83,84 would facilitate the appearance of recurrence. However, only a very few of the studies included in our review had assessed possible risk factors for recurrence after a course of ECT. The duration of the depressive episode and a greater number of episodes in the 2 years before the index episode could constitute risk factors.57 However, resistance to drugs or presence of psychotic signs and symptoms would not contribute to the appearance of a new recurrence. The methodological differences among the studies make interpreting the results more difficult and would explain how little reproduction there was in finding these risk factors or in their absence for recurrence following acute ECT in many other studies.46,55,58
Finally, in spite of the lack of studies that compare fixed and flexible session schedules in the use of C/M-ECT, specific clinical factors (such as the risk of performing unnecessary or less than optimum treatments, individual patterns of recurrence and the existence of residual symptoms, among others) lead us to recommend the individualisation of the initial schedule for sessions of C/M-ECT for each patient (flexible schedule). This schedule makes it possible to affect modifications based on the clinical evolution and tolerance to treatment, with the objective of making an early approach to early signs of recurrencse and the specific residual symptoms and reducing the risk of appearance of possible adverse effects.2,5
ConclusionThe data derived from the present review allow us to conclude that C/M-ECT could be considered a recommendable long-term treatment strategy in depressive patients who have needed ECT in the acute phase. The usefulness of the technique lies in data on efficacy, in the favourable impact on the course of the depressive illness and on its good tolerance profile. Even so, this usefulness should be backed by randomised prospective studies that exceed the limitations of the studies published to date and that make reliable assessment of C/M-ECT possible.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez-Amorós E, et al. Eficacia y patrón de uso de la terapia electroconvulsiva de continuación y mantenimiento en el trastorno depresivo mayor. Rev Psiquiatr Salud Ment (Barc.). 2012;5:241–53.