In women with acute abdominal pain in the right lower quadrant, acute appendicitis and obstetric and gynaecological pathologies are the main disorders to be eliminated. In the literature, there are no giant ovarian cysts reports associated to acute appendicitis. Here we show the case of an 18-year-old patient with menarche history at 12, irregular menstrual periods, 0 pregnancies and without pathological history, who has symptoms of abdominal pain, leukocytosis and peritoneal irritation data. It was decided to perform surgery, and during the procedure a giant ovarian cyst and perforated appendicitis with regional peritonitis were found. Thus, appendectomy and oophorectomy were performed with posterior satisfactory progress. This is the first case reported in literature of an acute appendicitis case coexistent with a giant ovarian cyst. The possibility of appendical origin associated to palpable mass should not be discounted in women with acute abdominal pain.
En mujeres con dolor abdominal agudo de predominio en cuadrante inferior derecho los principales trastornos a descartar son apendicitis aguda y patologías ginecoobstétricas. En la literatura no se tiene reportes de quistes gigantes de ovario asociados a apendicitis aguda. Aquí presentamos el caso de una paciente de 18 años de edad con antecedentes de menarca a los 12 años, ciclos menstruales irregulares, gesta 0 y sin antecedentes patológicos, la cual presenta cuadro de dolor abdominal, leucocitosis y datos de irritación peritoneal. Se decidió manejo quirúrgico, y durante el procedimiento se encontró un quiste gigante de ovario y apendicitis perforada con peritonitis regional, por lo que se efectuó apendicectomía y ooforectomía, con posterior evolución satisfactoria. Este es el primer caso reportado en la literatura de un caso de apendicitis aguda coexistente con un quiste gigante de ovario. No hay que descartar dicha posibilidad en mujeres con abdomen agudo de origen apendicular asociado a masa palpable.
Acute abdominal pain is the primary cause of emergency surgery in hospitals in our country.1 The causes of this clinical condition are diverse; they can be produced for any abdominopelvic organ involvement. In female patients, the pathology spectrum that can cause acute abdominal pain is wider than that of male patients. It is necessary to do a differential diagnosis between digestive causes and obstetric and gynaecological ones. The presence of acute abdominal pain secondary to acute appendicitis in intermediate or advanced stages associated to haemorrhagic cysts or ovarian torsion is an uncommon condition.2–10 Even more, in the literature there are no reports of giant ovarian cysts associated to acute appendicitis. In the present paper, we show the case of a patient with acute appendicitis coexistent with a giant ovarian cyst.
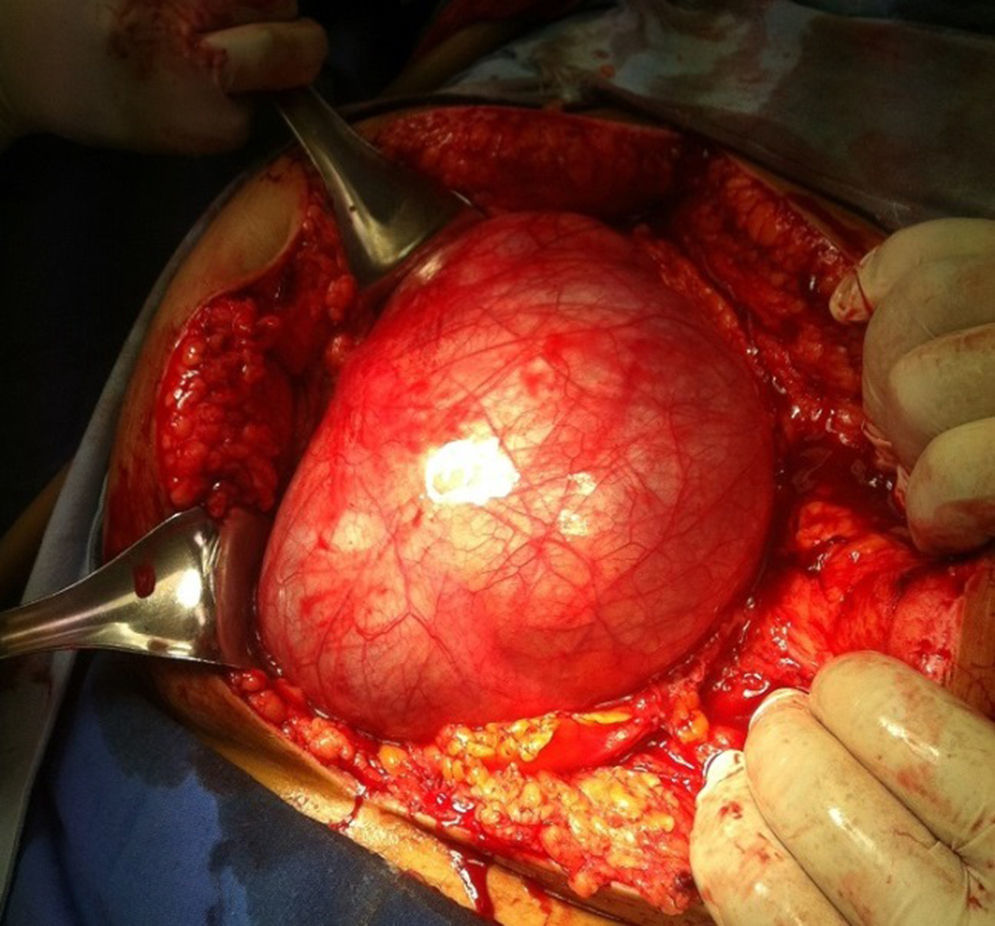
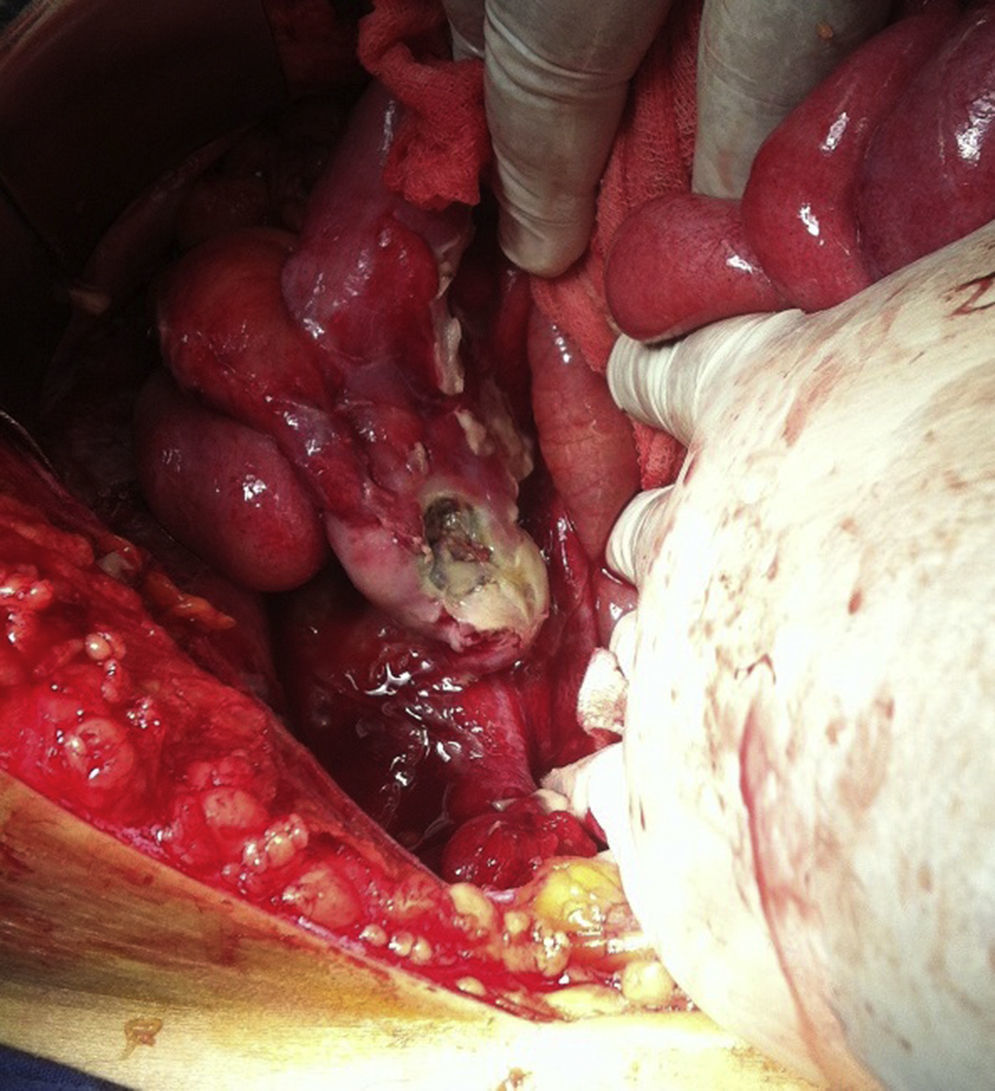
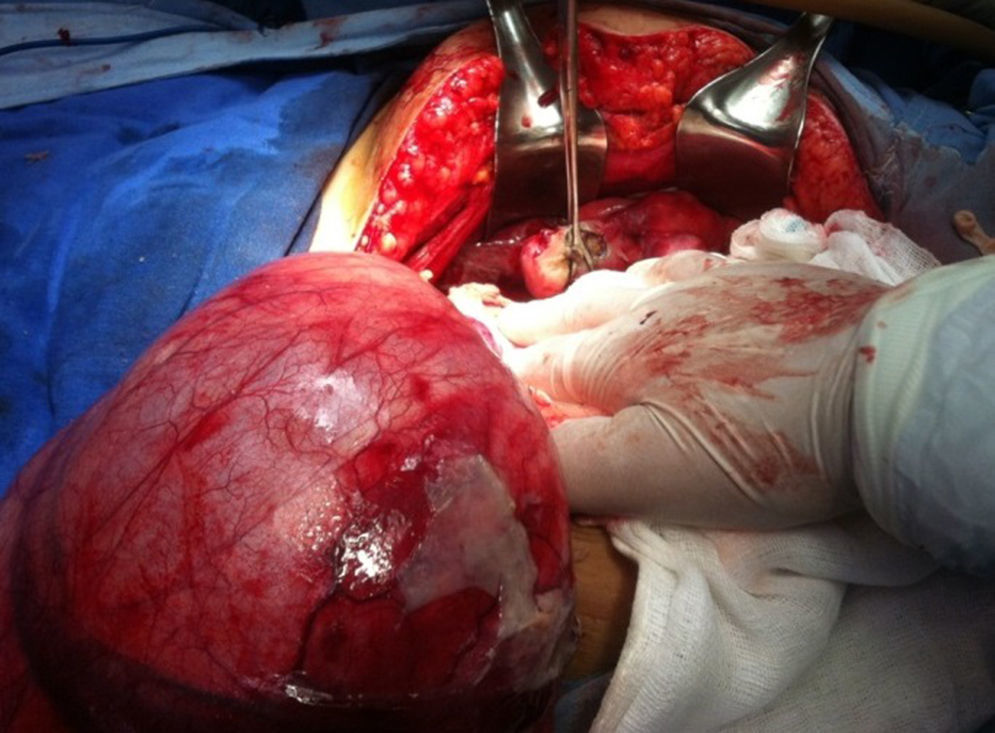
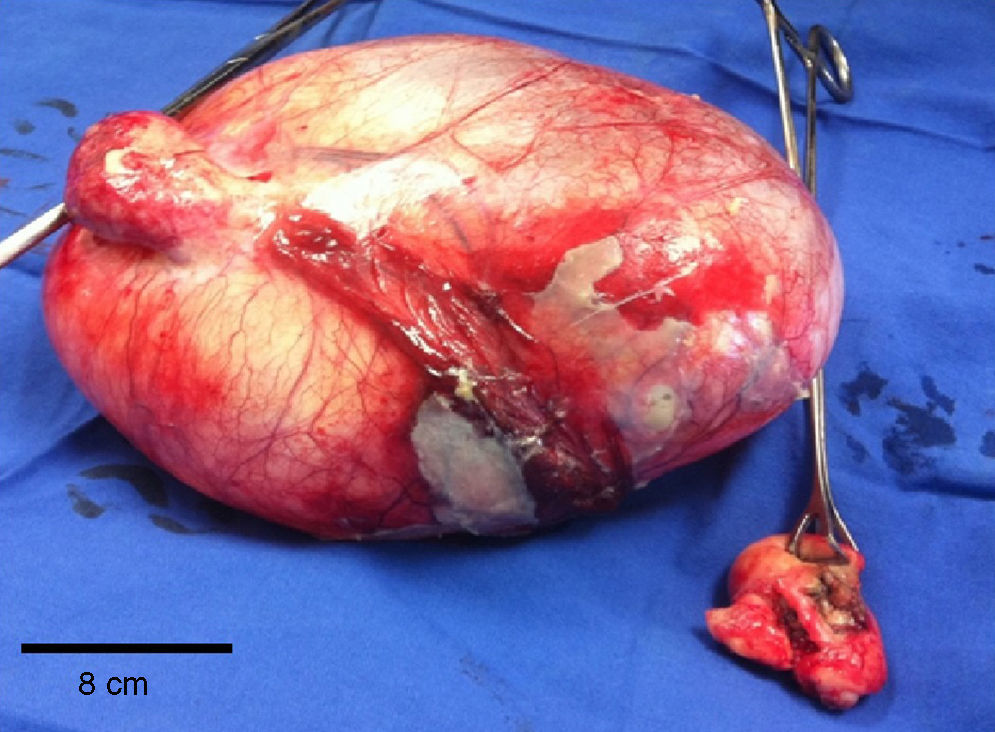
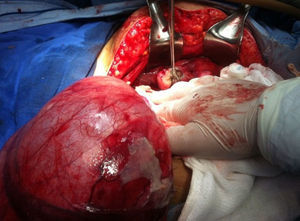
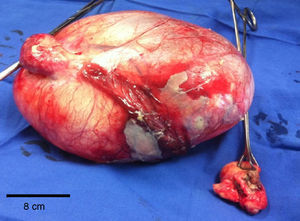
Clinical casePatient: an 18-year-old female with menarche, pubarche and thelarche history at 12 years, irregular menstrual periods, 0 pregnancies, without pathological history. Start of the ailment: seven days before her admission with 3/10 abdominal pain on an analogue scale of pain intensity, moderate intensity colic-type in mesogastrium, hypogastrium and right iliac fossa, accompanied by nausea, vomiting and decreased evacuation consistency. During the following two days, she showed an increase in the pain intensity to 8/10 on the analogue scale, hyporexia and unquantified fever. During the physical examination, she was a conscious and co-operative patient. Her weight was 61kg, height 157cm, with pain facies, integument paleness, normal state of hydration, without cardiopulmonary involvement but with tachycardia, distended abdomen preponderantly in the lower hemiabdomen, involuntary muscle resistance, superficial and deep palpation pain with prevalence in right lower quadrant and increase in significant volume of badly defined edges, McBurney and Von Blumber positive signs, tympanitic on percussion and absent peristalsis. On her admission, leukocytes of 20,800/mm3, neutrophils of 91.9% and Hb 9.3mg/dl stood out from the laboratory studies. Because of the clinical findings, the acute abdomen diagnosis was integrated due to probable complicated acute appendicitis, and surgery with a middle-line approach was decided. During surgery, a left ovarian cyst of 20cm×25cm×25cm was found (Fig. 1), caecal appendix of 12cm×3cm with middle third perforation (Figs. 2–4) and 300ml of free purulent material in cavity. Left oophorectomy and appendectomy were performed (Fig. 4), cavity lavage and drying with drainage placement. The patient had improvement at the postoperative stage and she was discharged from hospital 3 days after surgery. After the discharge, the patient made good progress and she is currently healthy. The pathological study reported an irregular vermiform appendix with perforation in the middle third and light occluded by faecaliths. It also reported follicular cyst ovary and serous cystadenoma with serous liquid inside it.
Acute appendicitis is the primary cause of emergency surgical intervention in the world, so much so that around 7% of the general population are subjected to appendectomy at some point in their lives.11 In second and third level hospitals in our country, 47% of acute appendicitis frequency has been reported in emergency abdominal surgeries in adults and from 3% to 21% of the total hospital admissions in paediatric patients.1,12,13 Despite the advances and greater availability of diagnostic studies, the white appendectomy percentage in the population in general has remained constant between 9% and 15% in recent years. What is more, the negative appendectomy rate in women is considerably lower in all the age ranges, reporting values from 20% to 30%.14,15 However, giant ovarian cysts are a relatively rare condition today owing to surgery performance and a greater availability of reliable diagnostic resources. These tumours are commonly asymptomatic, but when they cause symptomatology, this is related to the excessive growth that manifests as palpable abdominal mass or symptoms derived from the obstruction or irritation of the digestive or urinary tracts. Due to its commonly low and silent growth, when these conditions appear, they are often misdiagnosed after clinical and even ultrasonographic examination.16 In female patients with predominantly acute abdominal pain in the right lower quadrant, acute appendicitis and gynaecological pathologies are the main disorders to be eliminated (e.g. twisted cysts). The isolated appearance of some of these disorders is usual in these patients. And even a gynaecological pathology can simulate an acute appendicitis symptom, and vice versa; the acute adnexal pathology associated to appendicitis is a very rare situation. In fact, there are very few reports in medical literature.2–10,17–22 The first report of that association was noted in 1957 by Giorlando, who describes an acute appendicitis and paraovarian cyst case in a patient with situs inversus totalis.2 Later, Nikolaev describes a non-complicated appendicitis case associated to a twisted paraovarian cyst.3 Subsequently, in 1998 Tanaka was the first to describe three patients who showed broken ovarian cysts associated to acute appendicitis.7 More recently, in an interesting study expressly designed to study the surgical findings in girls with acute abdominal pain, it was reported that in patients from 4 to 14 years with predominant pain in the right lower quadrant, 83.7% of the cases were caused by isolated appendicitis and 13.6% were caused by appendicitis with a paratubal cyst. In that study, only 8.6% of the cysts were larger than 2cm; however, the authors do not mention the maximum dimensions found in any of the cases.9 From all the studies performed so far, the presence of a giant ovarian cyst temporarily associated to an acute appendicitis symptom was never described. In this report we describe the coexistence of the above pathologies. The report draws attention to the fact that in our case the giant cyst depended on the ovary contralateral to the appendix. Hazebroek et al. report the case of a patient with acute abdomen due to concurrent acute appendicitis with contralateral tubal pregnancy, on whom the diagnosis was performed, as in our case, during the surgical procedure but, unlike ours, laparoscopically.22 Likewise in other severe cases of acute abdomen and due to the clinical characteristics of the patient, the surgery was only chosen with a clinical suspicion that there might be complications due to acute appendicitis. In fact, we did not rely on an imaging study, i.e. pelvic ultrasound or abdominal computed tomography, in which the presence of giant ovarian cyst and concomitant appendicitis would have been observed. Before the possible incidental finding of an adnexal cyst in patients with abdominal acute pain, Vlanakis et al. recommend the systematic review of adnexes in all the patients with pain in the right lower quadrant to detect potential adnexal complications that can produce symptoms similar to appendicitis.9 Apart from agreeing with these authors, we also suggest the systematic review of the caecal appendix in every patient with adnexal pathology, even without appendicitis symptomatology, since it can coexist with evident or incipient appendical pathology associated to ovary or uterine tube complications.23
This is the first case reported in medical literature we know of in which an acute appendicitis symptom was associated to a giant ovarian cyst. Although the association of a giant ovarian cyst with acute appendicitis is unlikely, it can happen and this possibility should be eliminated in female patients with acute abdomen symptoms of appendical origin associated to palpable mass. In acute abdomen patients with a probable aetiology of acute appendicitis, it is important to conduct an intentional search for ovarian or tubal lesions which could require surgery to resolve them at the same time. Likewise, in annex pathology cases, particularly in large size lesions, it is important to eliminate the concomitant presence of appendicitis.
Conflict of interestThe authors declare that they have no conflict of interests.
To Jesús Quetzalcóatl Beltrán Mendoza, MD, PhD, for his warm and valuable contribution in the preparation of the present paper.