To evaluate factors associated with non identification of the sentinel lymph node (SLN) in lymphoscintigraphy of breast cancer patients and analyze the relationship with SLN metastases.
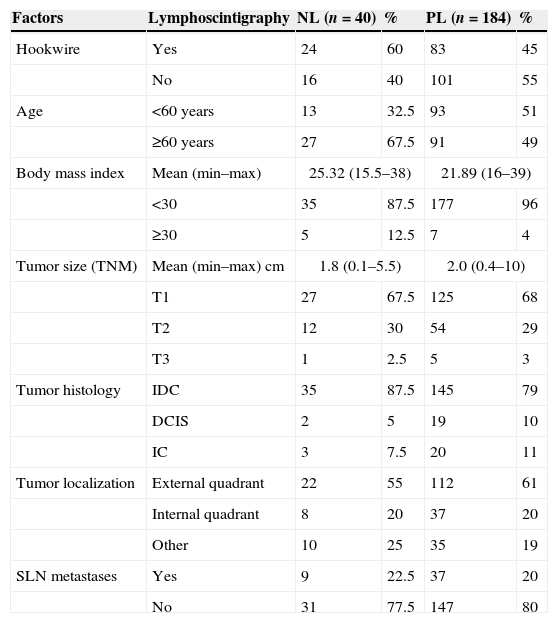
Material and methodsA single-center, cross-sectional and retrospective study was performed. Forty patients with lymphoscintigraphy without sentinel lymph node identification (negative lymphoscintigraphy – NL) were enrolled. The control group included 184 patients with SLN identification (positive lymphoscintigraphy – PL).
Evaluated factors were age, body mass index (BMI), tumor size, histology, localization, preoperative breast lesion hookwire (harpoon) marking and SLN metastases.
The statistical analysis was performed with uni- and multivariate logistic regression models and matched-pairs analysis.
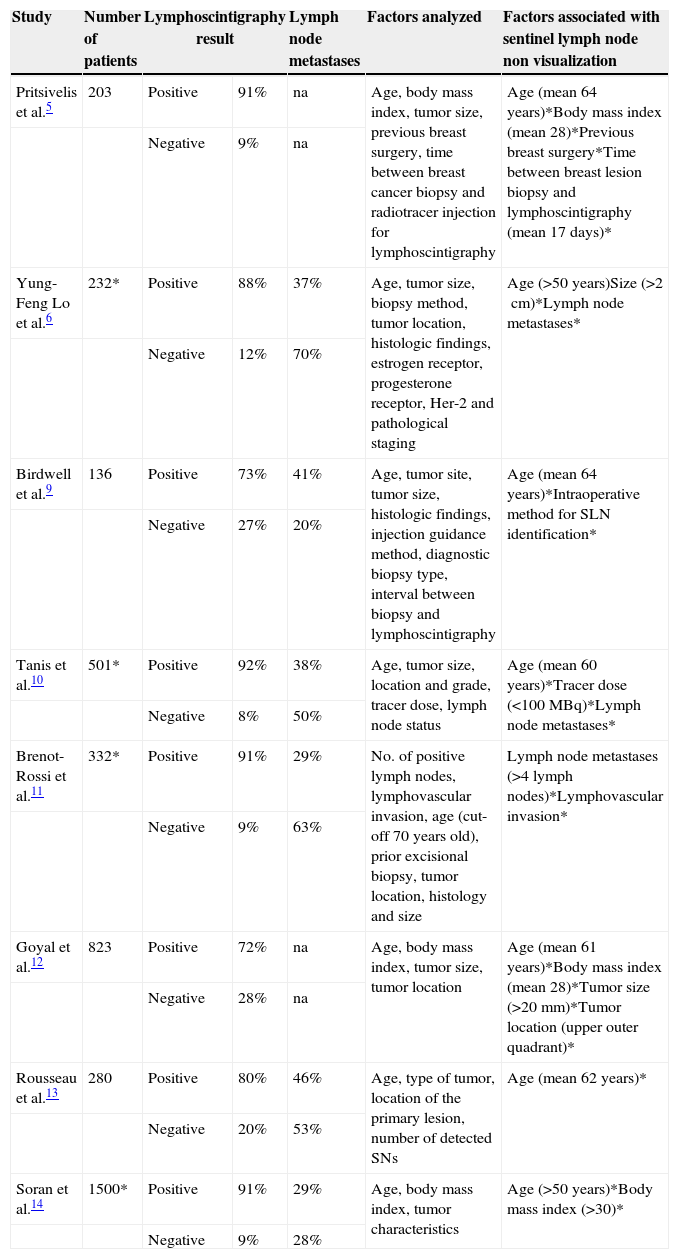
ResultsAge (p=0.036) or having BMI (p=0.047) were the only factors significantly associated with NL. Being ≥60 years with a BMI ≥30 increased the odds of having a NL 2 and 3.8 times, respectively.
Marking with hookwire seems to increase the likelihood of NL, but demonstrated statistical significance is lacking (p=0.087). The other tested variables did not affect the examination result. When controlling for age, BMI and marking with the harpoon, a significant association between lymph node metastization and NL was not found (p=0.565).
ConclusionsThe most important factors related with non identification of SLN in the patients were age, BMI and marking with hook wire. However, only the first two had statistical importance. When these variables were controlled, no association was found between NL and axillary metastases.
Evaluar los factores relacionados con la no identificación del ganglio centinela (GC) en la linfogammagrafía de pacientes con cáncer de mama y su relación con metástasis en el GC.
Material y metodosSe realizó un estudio unicéntrico, transversal y retrospectivo. Se seleccionaron 40 pacientes con linfogammagrafías sin identificación de GC (linfogammagrafía negativa - LN). El grupo control incluyó 184 pacientes con identificación del GC (linfogammagrafía positiva - LP).
Los factores evaluados fueron: edad, índice de masa corporal (IMC), tamaño, histología, localización, marcación preoperatoria del tumor con arpón e metástasis en el GC. El análisis estadístico se realizó mediante modelos de regresión logística univariante y multivariante y análisis pareado.
ResultadosLa edad (p=0.036) y el IMC (p=0.047) fueron los únicos factores asociados significativamente con LN. Tener edad ≥ 60 años o IMC ≥ 30 elevaron la probabilidad de tener una LN 2 y 3.8 veces, respectivamente.
La marcación con arpón parece aumentar la probabilidad de LN, pero sin significación estadística (p=0.087). Las otras variables no influyeron el examen. Al controlar edad, IMC y marcación con arpón, no se encontró una asociación significativa entre metástasis de ganglios linfáticos y LN (p=0.565).
ConclusiónLos factores más importantes relacionados con la no identificación del GC en las pacientes fueron edad, IMC y marcación con arpón, pero, sólo los dos primeros tuvieron relevancia estadística. Cuando se controló estas variables, no se encontró asociación entre LN y metástasis axilares.
Article
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)