Recalcitrant hip infection after arthroplasty presents a reconstructive challenge to orthopedic surgeons. The aim of this study is to evaluate the results with a vastus lateralis muscle flap used to treat these recalcitrant hip infections in our Department.
Material and methodsA retrospective descriptive study was conducted on five patients with deep hip infections by transposition of the vastus lateralis muscle flap. Average age: 70.5years. Mean follow-up: 30months (range, 25–34months). All patients had previously undergone other major surgical procedures (mean of 3.7 previous procedures). All had multiple microbial infections before surgery. The pathogens involved using cultures of the fistula, the outcome of the wound and laboratory results, including C-reactive protein (CRP), were analysed.
ResultsHealing was achieved in the five patients who underwent surgery without requiring any further procedures or inflammatory signs of infection. CRP returned to normal one month after surgery, and there was no morbidity or mortality related to surgical technique.
ConclusionIn our experience, the vastus lateralis muscle flap as a treatment for recalcitrant deep infection after arthroplasty has presented good results, provided there are appropriate antibiotic therapy and surgical debridement, thus achieving wound healing and a return to normal of the CRP.
La infección recalcitrante de cadera tras artroplastia es una complicación de difícil tratamiento para el cirujano ortopédico. El objetivo de este estudio es evaluar los resultados de estas infecciones de cadera recalcitrantes que hemos tenido en nuestro Servicio tratadas con el colgajo de vasto externo.
Material y métodosEstudio descriptivo retrospectivo de 5 pacientes con infecciones profundas de cadera mediante trasposición de colgajo del músculo vasto lateral. Edad media: 70,5 años. Tiempo medio de seguimiento: 30 meses (rango, 25–34 meses). Previamente todos los pacientes habían sido sometidos a distintos procedimientos quirúrgicos mayores (media de 3,7 procedimientos previos). Todos presentaban infecciones polimicrobianas previas a la cirugía. Se estudió los agentes patógenos involucrados mediante cultivo de la fístula, la evolución de la herida, así como controles analíticos, incluidos la proteína C-reactiva (PCR).
ResultadosSe consiguió la curación de la herida en los 5 pacientes intervenidos, sin necesidad de realizar ningún otro procedimiento posterior ni aparición de fístula ni otros signos flogóticos de infección. La PCR se normalizó al mes de la intervención y no hubo morbi-mortalidad relacionada con la técnica quirúrgica.
ConclusiónEn nuestra experiencia, el colgajo de músculo vasto lateral como tratamiento para la infección profunda recalcitrante tras artroplastia de cadera ha presentado buenos resultados, siempre enmarcado dentro de un adecuado tratamiento antibiótico y desbridamiento quirúrgico, consiguiendo la curación de la herida y normalización de la PCR.
Recalcitrant hip infection after arthroplasty is probably one of the most intractable complications for orthopaedic surgeons. Conventional treatment consists of adequate debridement and antibiotics. However, a certain percentage of these infections is not resolved by these methods. The Girdlestone resection arthroplasty technique is the most popular option in patients with deep, recurrent infections,1,2 but even with this technique 20% of infections are not cured,3,4 even raising the possibility of disarticulation. In these recalcitrant cases, large dead spaces remain in the acetabular cavity and in the previous femoral neck and greater trochanter areas after the Girdlestone technique. These dead spaces represent an excellent breeding ground for the perpetuation of infection. The purpose of a vascularised vastus lateralis muscle flap is to fill these dead spaces with healthy and well-vascularised muscle tissue, enabling an adequate local supply of blood and, therefore, of antibiotic therapy.5
Materials and methodsWe performed a retrospective study of 5 patients (3 females and 2 males) who suffered deep and recalcitrant hip infections after total hip arthroplasty or review thereof, and who were operated between July 2008 and March 2009 by radical debridement and transposition of a vastus lateralis muscle flap.
The mean age of patients was 71.6years (range: 61–78years).
All patients had undergone prior and different surgical procedures (mean figure of 3.7 prior procedures) before transposition, including extensive debridement and surgical cures, vacuum assisted closure (VAC), withdrawal of prosthetic components and placement of antibiotic cement spacers, without satisfactory results.
We studied comorbidities and local factors of poor prognosis in the surgical wound (Table 1), elevation of C-reactive protein (present in all cases), microbial agents involved, evolution of the surgical wound, presence of phlogotic signs and fistulas, and the comorbidity caused. The surgical histories were as follows:
Case 1: patient with intertrochanteric femoral fracture synthesised with an intramedullary trochanteric nail. He was reintervened by total hip arthroplasty (THA) due to necrosis and cutting phenomenon. He presented deep infection requiring a Girldestone-type resection arthroplasty with cement spacer, which did not resolve the infection.
Case 2: patient with coxarthrosis treated primarily with total hip arthroplasty. She required several replacements due to periprosthetic fracture and dislocation. She presented deep infection requiring a Girldestone-type resection arthroplasty with cement spacer, which did not resolve the infection.
Case 3: patient with subcapital femur fracture who underwent total hip arthroplasty. She suffered deep infection which was treated by a Girldestone technique. At 6months, she underwent Girldestone salvage, presenting a new deep infection which was not resolved.
Case 4: patient with coxarthrosis treated by total hip arthroplasty. She required arthroplasty review due to disimplantation thereof. She presented deep infection requiring a Girldestone-type resection arthroplasty.
Case 5: patient with coxarthrosis treated by total hip replacement. He presented deep infection requiring a Girldestone-type resection arthroplasty with cement spacer, which did not resolve the infection.
Characteristics of patients.
| Patient number | Age | Gender | Diagnosis | Concomitant disease | Local factors surgical wound | Previous procedures |
| 1 | 71 | M | THA infection | Myasthenia gravisCorticosteroidsCOPDBPH | Active wound infection with purulent secretion. Multiple previous incisions and interventions | 3 |
| 2 | 70 | F | THAR infection | Repeated UTIAHTCOPD | Active wound infection with purulent secretion. Multiple previous incisions and interventions | 4 |
| 3 | 78 | F | THAR infection | Pulmonary hypertensionAtrial fibrillationMorbid obesityCOPDAHT | Active wound infection with purulent secretion. Multiple previous incisions and interventions.Chronic venous insufficiency | 4 |
| 4 | 61 | F | THAR infection | AHTPE | Active wound infection with purulent secretion. Multiple previous incisions and interventions | 3 |
| 5 | 78 | M | THA infection | AHT | Active wound infection with purulent secretion. Multiple previous incisions and interventions | 4 |
AHT: arterial hypertension; BPH: benign prostatic hyperplasia; COPD: chronic obstructive pulmonary disease; F: female; M: male; PE: pulmonary embolism; THA: total hip arthroplasty; THAR: total hip arthroplasty replacement; UTI: urinary tract infection.
All 5 patients had polymicrobial infections with very difficult antibiotic management. Throughout the natural history of each patient, we found more than 5 microorganisms in surgical wound cultures (Table 2).
Pathogenic microorganisms.
| Pathogen number | Pathogens | Time (weeks) girdlestone vastus lateralis muscle flap | Follow-up (month) | |
| 1 | ORSAEscherichia coliPseudomona aeruginosa | Morganella morgagniiKlebsiella pneumoniae | 4 | 30 |
| 2 | Proteus mirabilisEscherichia coliEnterococcus faeciumEnterobacter cloacae | Pseudomona aeruginosaStaphylococcus epidermidisStreptococcus agalactiae | 30 | 32 |
| 3 | Pseudomona aeruginosaAcinetobacter baumaniiEnterococcus faecalisProteus mirabilis | Alcaligenes faecalisCandida parapsilosisAcinetobacter lwoffiStaphylococcus hominis | 56 | 34 |
| 4 | Staphylococcus epidermidisSphingomonas paucimobilisEnterobacter cloacae (ESβL) | Enterococcus faecalisKlebsiella pneumoniaeStaphylococcus aureusPseudomona aeruginosaCandida albicans | 0 | 25 |
| 5 | Staphylococcus epidermidisLeuconostoc sppEnterobacter cloacae | Candida albicansPropionibacterium acnes | 10 | 29 |
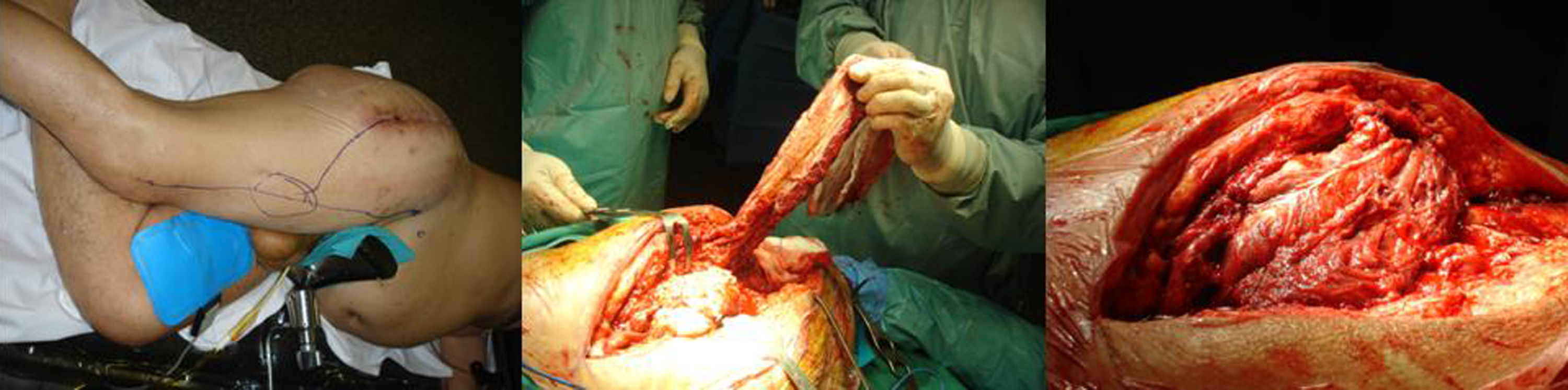
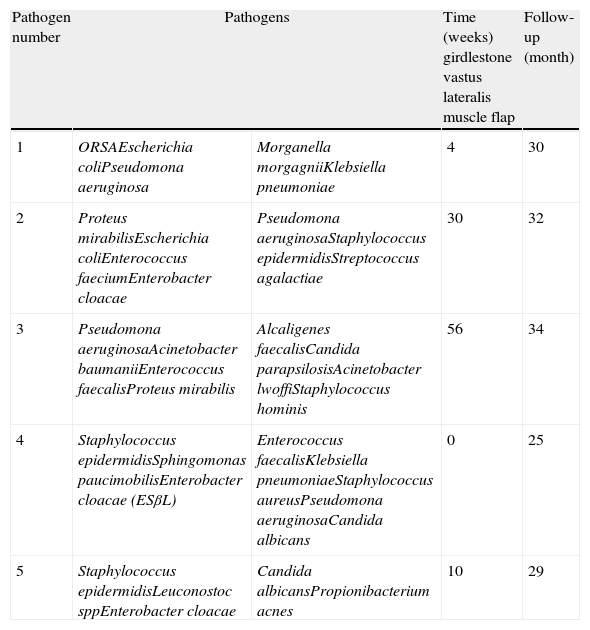
Patients were placed in the lateral position on the operating table and a lateral incision was made on the skin of the thigh. The hip was approached in order to perform extensive radical debridement. After debridement, we placed wet dressings on the resulting cavity (Figs. 1 and 2).
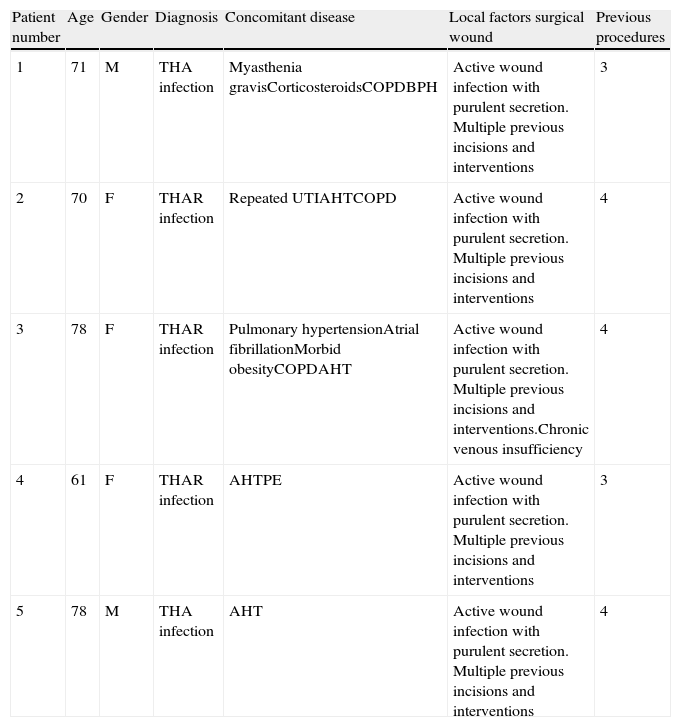
Flap dissection usually began on the anterior margin of the rectus femoris muscle. The vascular pedicle was easily located by medially retracting this muscle. Dissection continued distally, with the end of the flap being immediately distal to the muscle–tendon junction. Subsequent dissection between the vastus lateralis and vastus intermedius muscles was performed by separating them carefully and ligating the perforating vessels. The flap was isolated together with its vascular pedicle. Subsequently, once its distal insertion was released, we rotated the flap 180° and used it to fill the debrided cavity. The transposition of the flap was fixed by suture in the periacetabular area.
During the postoperative period, patients remained in bed for 1–2weeks, without traction, with local treatment every 24h and with periodic repositioning, avoiding the lateral position on the intervened limb for 3weeks. They also followed intravenous antibiotic therapy. Thereafter, partial load with a walking frame or cane was allowed on an outpatient basis.
All patients continued antibiotic treatment, based on previous cultures, for at least 6weeks.
ResultsThe mean follow-up period was 30months (range: 25–34months). The mean period between Girldestone-type resection arthroplasty and vastus lateralis flap transposition was 20weeks (range: 0–56weeks).
The mean duration of surgery was 180min (range: 120–210min), with a mean 3 units of packed erythrocytes being required during the procedure (range: 1–4 units).
Healing of the deep hip infection was achieved in all 5 intervened patients, without the need for any other procedure except surgical cures of small defects in the surgical wound. There were no new fistulas or phlogotic signs of infection, with subsequent cultures being negative. The surgical wound healed within a mean period of 15days (range: 10–20days).
C-reactive protein became normalised 1month after the intervention.
There was no decrease in knee flexion/extension strength.
All patients required a walking frame or cane for ambulation.
One patient (case 4) presented pneumonia 9months after surgery.
DiscussionDeep infection after hip arthroplasty is a complication with difficult solution. Conventional treatment consists of adequate debridement and antibiotic therapy, but a percentage of these infections are not resolved by such methods. The Girdlestone resection arthroplasty technique is the most popular option in patients with recurrent, deep infections,1,2 but even with it, 20% of infections are not resolved,3,4 with the possibility of disarticulation being considered.
In general, in these recalcitrant cases, after the Girdlestone technique it is possible to observe large dead spaces in the acetabulum cavity, as well as in the previous femoral neck and the greater trochanter areas. These spaces represent an excellent breeding ground for the perpetuation of infection for various reasons: the haematoma located in that area, poor antibiotic penetration and fibrotic tissue surrounding it.
Following extensive debridement, filling these spaces with healthy and well-vascularised muscle tissue may resolve the previously described causes of infection, thus ensuring an adequate, local supply of blood and, therefore, of antibiotic therapy.5
There are various flap possibilities, including free latissimus dorsi flaps, which require microsurgical anastomosis, and locoregional flaps, such as gluteus medius, tensor fascia lata,6 rectus femoris4 and rectus abdominis7 flaps, all with some limitations (inadequate volume, general lesion due to previous approaches, difficulties in their implementation, etc.4,6,7).
Vastus lateralis muscle flaps enable an adequate filling of the dead space. This muscle and its vascularisation are generally well-preserved, even after multiple previous interventions. In addition, it shares a fasciocutaneous region which can be used in the subsequent wound closure, allowing ample resections of devitalised tissue and fistulas.4,7–9 It does not cause functional defects in the donor area, as they are compensated by the rest of the quadriceps muscles; muscular coverage of the femur is maintained by the vastus intermedius and rectus femoris muscles. Partially filling the cotyloid cavity prevents the elevation of the remaining proximal femur, facilitating ambulation and a possible review surgery in a second procedure.
ConclusionIn our experience, vastus lateralis muscle flaps have shown good results as a treatment for recalcitrant deep infections after hip arthroplasties. These results were based on an appropriate antibiotic therapy and surgical debridement, achieving wound healing and normalisation of C-reactive protein levels.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rodríguez-Rosales G, et al. Tratamiento de la infección recalcitrante de cadera mediante colgajo de músculo vasto lateral. Rev Esp Cir Ortop Traumatol. 2012;56:439–43.