“Minimally invasive” techniques have been recently been developed in order to achieve good clinical results with a low incidence of complications. The extralateral interbody fusion or direct transpsoas is a minimally invasive anterior arthrodesis. A total of 97 patients with 138 segments received surgery between May 2012 and May 2015. The follow-up was from 12 to 44 months. The mean age was 68 years (41–86). The most common cause of intervention was the adjacent segment (30%), deformity (22%), and lumbar disc disease (21%). The interbody cage was implanted as: single (stand-alone) in 33%, and additional fixation was used in the others: Screws, percutaneous unilateral (11%), bilateral (27%), or with a lateral plate (62%). The mean stay was 3.2 days (2–6). The score on a lumbar visual analogue scale decreased from 9 to 4.1, and dropped to 3 after 1 year. The improvement in disc height was from 8.4mm to 13.8mm, and a larger increase in the foramen diameter from 10.5 to 13.1mm, which were statistically significant. The early major complications recorded were, three motor femoral nerve injuries and retroperitoneal haematoma (4%), and the early minor were: two fractures (2%). As major late complications there was an abdominal hernia, a mobilization of 10mm and three radiculopathy (5%), and as minor late, three fracture, two mobilisations greater than 10mm, four mobilisations of less than 10mm, and one mobilisation of a screw plate (10%). The extralateral interbody fusion technique is a safe and reliable when performing a lumbar fusion by an alternative minimally invasive route.
Durante los últimos años se han desarrollado técnicas «mínimamente invasivas» de artrodesis que pretenden alcanzar los buenos resultados clínicos con una baja incidencia de complicaciones. La artrodesis intersomática extralateral o directa transpsoas es una artrodesis anterior mínimamente invasiva. Se han intervenido desde mayo de 2012 hasta mayo de 2015, un total de 97 pacientes con 138 segmentos intervenidos. El seguimiento fue de 44 a 12 meses. La edad media fue de 68 años (41-86). La causa más frecuente de intervención fue el segmento adyacente (30%), la deformidad (22%) y la discopatía lumbar (21%). La caja intersomática se implantó: sola («stand-alone»), en el 33% y se utilizó fijación adicional en el resto: tornillos percutáneos unilaterales (11%), bilaterales (27%) o con placa lateral (62%). La estancia media fue 3,2 días (2-6). La puntuación de la escala analógica visual lumbar pasó de 9 a 4,1 bajando a 3 a partir del año. La mejoría de la altura del disco fue de 8,4mm a 13,8mm y un aumento del diámetro mayor del foramen de 10,5 a 13,1. Dichas diferencias son estadísticamente significativas. Se registraron complicaciones precoces mayores: tres lesiones motoras del nervio femoral y un hematoma retroperitoneal (4%); y precoces menores: dos fracturas/hundimientos (2%). Como tardías mayores: una hernia abdominal, una movilización de 10mm y tres radiculopatías (5%); y como tardías menores: tres fracturas/hundimiento, dos movilizaciones mayores de 10mm, cuatro movilizaciones menores de 10mm y una movilización de un tornillo de una placa (10%). La técnica artrodesis intersomática extralateral constituye una alternativa segura y fiable a la hora de plantear una artrodesis lumbar por vía mínimamente invasiva.
It has been demonstrated over time that lumbar interbody fusion is an effective surgical procedure from a clinical and economic perspective for the treatment of a multitude of diseases that affect the spine (deformities, spondylolisthesis, degenerative processes, fractures or tumoural disease), the lumbar spine in particular.1 Although the principles that govern achieving good interbody fusion have remained unchanged through the years, the surgical techniques and instruments have developed very significantly. Currently we have a great variety of materials and techniques for lumbar interbody fusion. In recent years “minimally invasive” surgical techniques have been developed that aim to achieve at least the same clinical outcomes in terms of interbody fusion and symptom relief but with a lower rate of complications.2 At present we have several approach routes which enable us to perform various anterior interbody fusion techniques: the anterior approach (ALIF), transsacral approach (AxialLIF), posterior approach associated with pedicle screws (PLIF), transforaminal approach associated with pedicle screws (TLIF) and finally, extreme lateral interbody fusion or direct transpsoas (XLIF). XLIF is anterior arthrodesis of the lumbar spine performed as a minimally invasive procedure.
The XLIF technique has a series of advantages over other minimally invasive techniques, because the interbody implant enables us to correct deformity, restore intervertebral disc height, achieve interbody fusion of the operated segment and indirectly decompress the neurological elements. Complications using the XLIF technique appear to be fewer than those reported after other surgical techniques.3–6
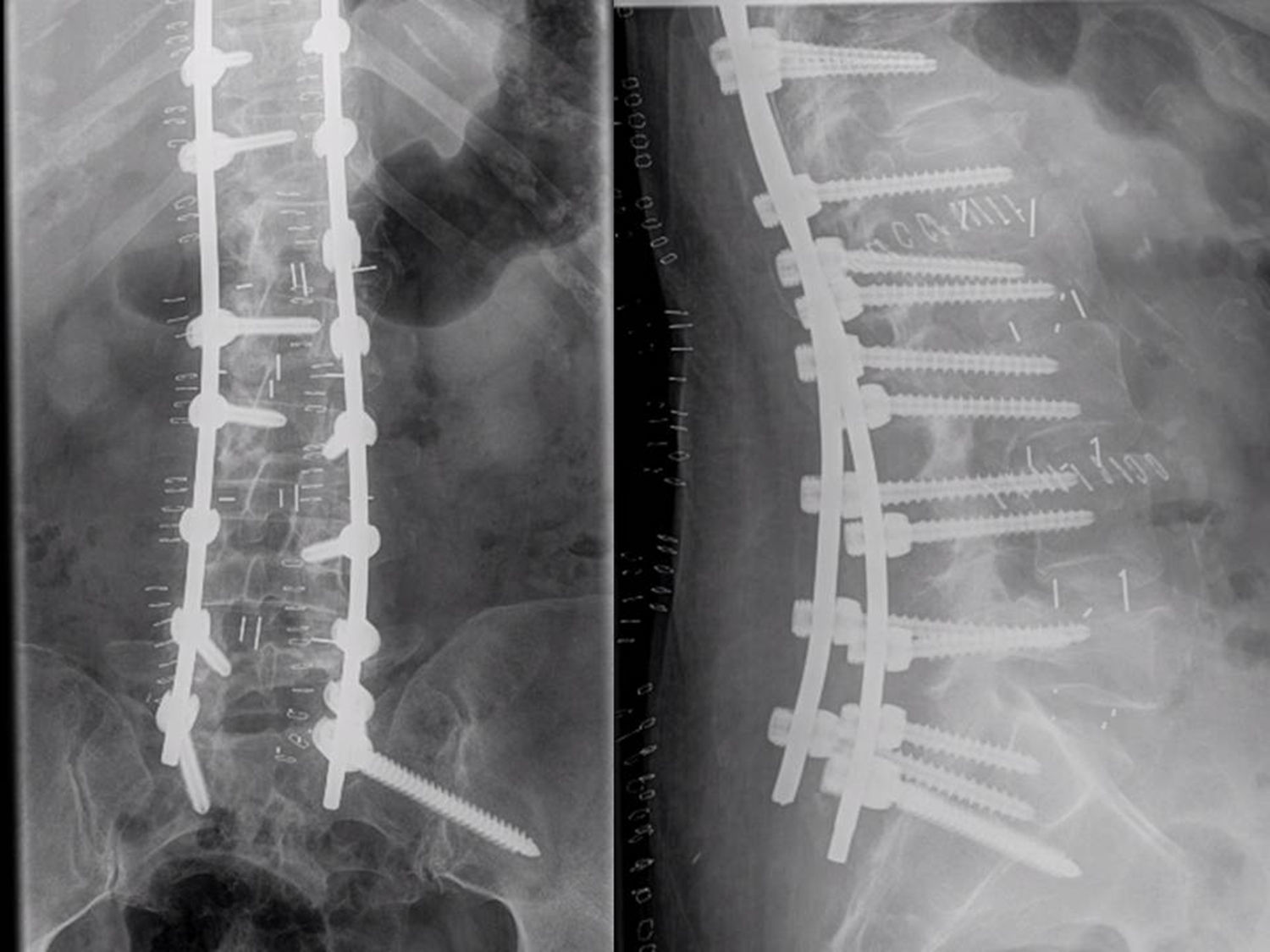
Material and methodsA total of 97 patients were operated from May 2012 to May 2015, and 138 segments were operated (1.4 per patient). The maximum follow-up was 44 months and the minimum 12 months. The mean age was 68 years (41–86). The most frequent cause for intervention was disease of the adjacent segment (30%) (Fig. 1), followed by deformity (22%) (Fig. 2) and lumbar discopathy (21%).
The surgery was performed with the patient in the lateral position (Fig. 3) on a radiotransparent table with a break at the lumbosacral area. When the anatomy of the lumbosacral spine and pelvis allowed, we positioned the patient with the painful side upwards, i.e., the approach was via the side where the radicular symptoms presented. With the help of the imaging intensifier on lateral view, we marked a vertical line crossing the centre of the intervertebral disc to be operated and another horizontal line on the centre of the disc. Another incision of about three or four cm was made through which up to three levels could be reached. After the skin and the subcutaneous tissue, the oblique abdominal muscle fascia was opened to the retroperitoneum. Through blunt dissection, the transverse process of the superior vertebra, the psoas muscle and the intervertebral disc were palpated using a finger. The guiding needle was placed in the appropriate position under radioscopic control and a first neurophysiological check made. A working window was created through the psoas muscle using a series of dilators. This gesture was performed under strict intraoperative neurophysiological control at all times. The Ravine© (K2M) separator was used and introduced through the needle located in the intervertebral disc; we then proceeded to open it. The site for fixing the first valve to the vertebral body with a nail of the same length was located under radioscopic control. The needle was removed from the intervertebral disc and the other valve opened and fixed to the other vertebral body. After setting the light sources, the anterior and/or posterior valve was placed with special care, under neurophysiological control at all times, since the femoral nerve can be compressed causing it neuropraxia. Once the intervertebral disc had been located it was opened with a scalpel and the discectomy performed. The vertebral discs were then prepared down to subchondral bone and dilators introduced which gave us an idea of the size, length and width of the implant. Once the measurements had been decided a test cage was introduced and its placement and primary stability checked under radioscopic control. The definitive implant is radiotransparent because it is polyetheretherketone and has markers to check its appropriate interbody placing. It is inserted filling it with demineralised bone matrix to promote interbody fusion. Practically all implant models have cages with heights from 8 to 14mm in 2mm increments, lengths from 45 to 60mm in 5mm increments and widths of 18 and 22mm. The interbody fusion cage was placed stand-alone in 33% of our patients; additional fixation was used in the remainder. This fixation was achieved with unilateral percutaneous screws (11%), bilateral percutaneous screws (27%) or with a lateral plate (62%), depending on the patient's anatomy and pathology.
We perform the XLIF technique under constant neurophysiological monitoring which keeps us informed of the situation of the lumbar plexus at all times.
Thanks to the use of monitoring,7,8 the rate of complications after this surgical technique has drastically reduced making it an inestimably valuable tool for the spinal surgeon. We use four intraoperative neurophysiological monitoring techniques: transcranial motor evoked potentials (TcMEP), somatosensory motor evoked potentials (SSEP), free running-EMG and triggered-EMG.
A statistical study was performed of the progress of disc and foraminal height measurement before surgery, during the immediate postoperative period and in the follow-up consultations. To that end, a comparative study was undertaken using SPSS 15.0, performing the t-test adjusted with the Bonferroni method for multiple comparisons, paired calculation of the differences and creating a linear model for paired comparison of the measurements obtained in disc and foraminal height at the different times.
ResultsSurgery time per segment was 35min, 57min if additional fixation was performed. With regard to postoperative analysis, the mean hospital stay was 3.2 days (2–6), estimated blood loss per segment was 40ml. On analysis of outcomes with regard to pain, the higher the VAS score the greater the pain, the preoperative lumbar visual analogue scale (VAS) score reduced from 9 to 4.1, in the postoperative period (a 53% reduction), and to 3 (a 66% reduction) at 1 year. The VAS of the foot reduced from 9 in the preoperative period to 5.2 in the postoperative period (reduction of 42%) and remained stable at 1 year.
From a radiological perspective, an improvement in intervertebral disc height was observed from 8.4mm in the preoperative period, to 13.8mm, which constituted a gain of 65%, and an increase in the major diameter of the foramen from 10.5mm to 13.1mm (a gain of 24%).
We differentiated complications into medical or surgical and then, early or delayed and major or minor complications. “Early complications” were defined as those that occurred in the first month and therefore could be directly associated with the surgical intervention. We defined a “major complication” as any event that required reoperation and/or in which there was motor neurological impairment that had reduced by at least one point from the previous examination (Table 1).
Complications.
| Major early surgical (4%) | Minor early surgical (2%) | Major late surgical (5%) | Minor late surgical (10%) | Major early medical (0%) | Minor early medical (10%) |
|---|---|---|---|---|---|
| Three motor injuries to the femoral nerve | Two fractures/depression | One abdominal hernia | Three fractures/depression | Paralytic ileus | |
| One retroperitoneal haematoma | Three radiculopathies. One movement of the cage greater than 10mm | Two movements greater than 10mm | |||
| Four movements less than 10mm | |||||
| One movement of a plate screw |
There were no deaths, injuries to the dura mater, no cerebrospinal fluid fistulae or psuedomeningoceles, no periradicular fibroses, no major vascular injuries, no visceral injuries and no infection in our series.
The major surgical complications merit more detailed mention.
Motor injuriesAs mentioned earlier, there were three motor injuries. The three were on the contralateral side at level L4–L5 and affected the femoral nerve. All three were detected by the neurophysiologist and all three fully recovered in less than 6 months. We attribute these injuries to over distraction of the disc space when inserting the test cage (Fig. 4).
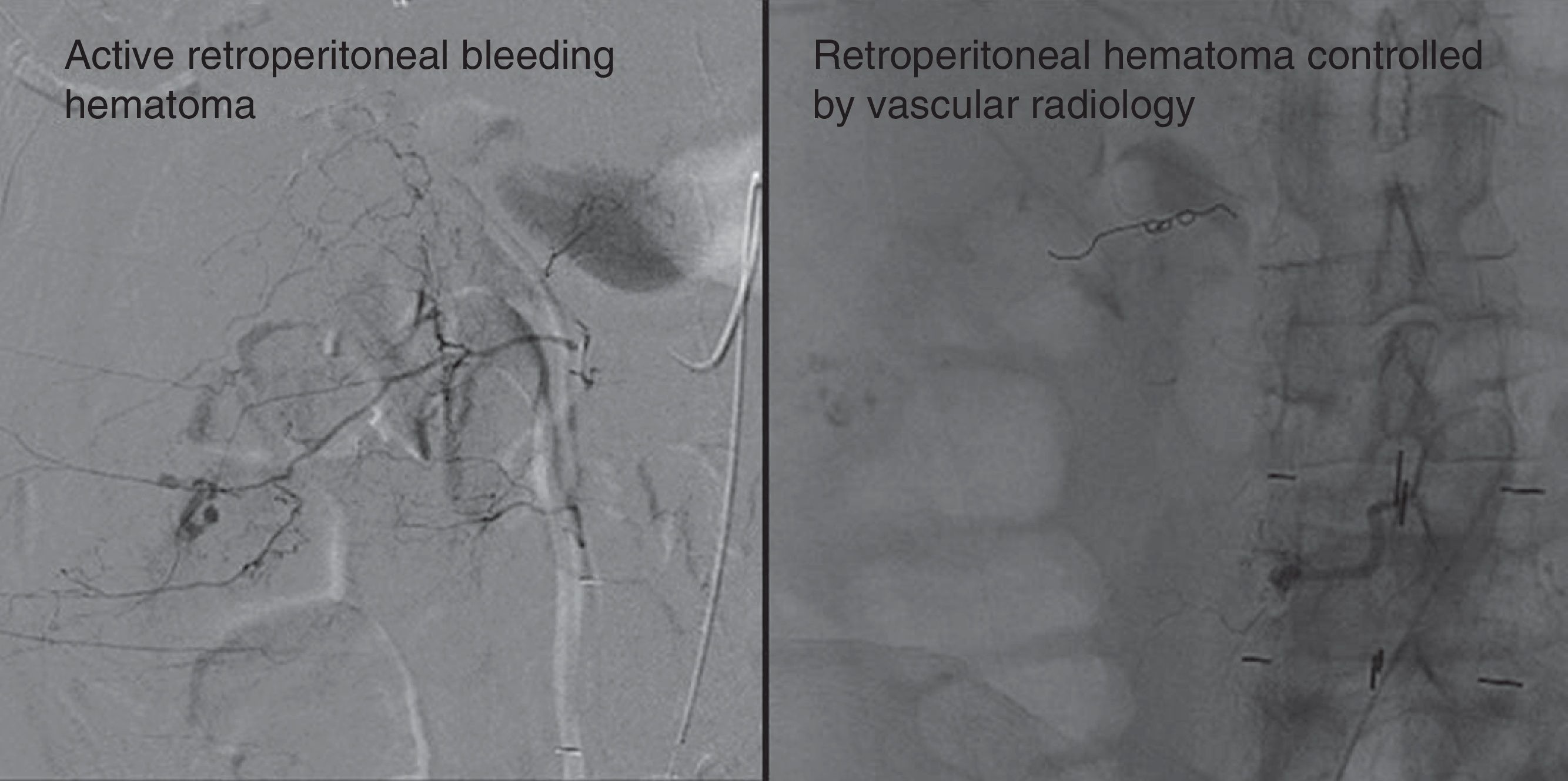
Retroperitoneal haematomaThis was a 76-year-old patient treated with anticoagulants for valvular heart disease. Five days after the XLIF the patient started with sweats, tachycardia, decreased haematocrit levels. A large retroperitoneal haematoma was observed from 5 points due to active bleeding (Fig. 5, left) (treated by the vascular surgery department and the bleeding was controlled (Fig. 5, right).
Abdominal herniaAn obese 82-year-old woman presented a painful mass at the level of the surgical scar after a fall 7 months post intervention. The symptoms resolved on placing a mesh at this level.
Radicular painThree persistent radiculopathies after the operation were recorded, radiculography was performed on all of them and infiltration of corticosteroids, one of them clearly improved and therefore the procedure was repeated on two further occasions and the clinical symptoms resolved. In the other two cases, the radiculopathy had been caused by facet compression. After imaging studies a posterior decompression was performed using a minimally invasive technique and the symptoms resolved.
Movement of the implantThe implant moved more than 10mm in a 75-year-old woman who had undergone a stand-alone procedure who, after 2 asymptomatic months and after indirect trauma, started to experience severe lumbar pain radiating to her lower left limb. The imaging study showed movement greater than 10mm (Fig. 6). The cage was changed via the same transpsoas route for another of a greater height (12mm rather than 10mm) and four percutaneous screws were placed at that level.
The total major complication was 9% and minor complications 13%. The sum of all these complications gives us an incidence of 22%.
The incidence of pain, discomfort, paresthesia and symptoms to the proximal third of the thigh on the side of the approach route deserves separate mention. There are many reports (Table 3) of this circumstance. These events presented in 30% of cases in our series. All of them resolved in less than 6 months.
The statistical study found statistically significant differences in the difference in disc and foraminal height.
The complete series comprised 138 implants using the clinical criteria used in most of the literature, the preoperative period, immediate postoperative period and at follow up at 6, 12, 18 and 24 months were considered the appropriate times for measuring the disc and foraminal heights. The progress of both radiological parameters was similar, both the discs and the foramens recorded a statistically significant increase. The mean height of the discs was 7.2mm and after surgery it was 12.58mm, therefore the improvement was 5.44mm (75%) (p 0.0001). The foramens improved by 6.74mm (63%) (p 0.001), since they went from 10.6mm to 17.34mm. During the follow-up consultations statistically significant differences were recorded in the reduction in disc and foraminal height increase. Both parameters decreased during the first 6 months, the mean reduction was approximately 1mm (discs: 0.73mm and foramens 1.03mm). During subsequent follow-up (at 12, 18 and 24 months) a reduction of less than 0.5mm was recorded (Table 2).
During subsequent follow-up (at 12, 18 and 24 months) a reduction of less than 0.5mm was recorded.
| Comparison of disc height measurements pre-Sx with progress | |||||
|---|---|---|---|---|---|
| Mean | Standard deviation | Lower | Higher | Sign. | |
| Pair 1 Disc. Pre-disc. Post Sx | 5.440 | 2.738 | −5.908 | −4.972 | 0.000 |
| Pair 2 Disc. Post Sx–Disc-Post_6m | 0.739 | 1.238 | 0.527 | 0.950 | 0.000 |
| Pair 3 Disc. Pos_6–Disc. Post_12m | 0.350 | 0.730 | 0.205 | 0.495 | 0.000 |
| Pair 4 Disc. Post_12–Disc post_18m | 0.394 | 0,782 | 0.202 | 0.586 | 0.000 |
| Pair 5 Disc. Post_18–Disc Post_24m | 0.438 | 0.619 | 0.214 | 0.661 | 0.000 |
| Comparison of largest foraminal diameter height measurements pre Sx with progress | |||||
|---|---|---|---|---|---|
| Mean | Standard deviation | Lower | Higher | Sign. | |
| Pair 1 Foramen. Preforamen. Post Sx | −6.73 | 4.157 | −7.449 | −6.029 | 0.000 |
| Pair 2 Foramen. Post.QX–Foramen-Post_6m | 1.030 | 2.007 | 0.687 | 1.373 | 0.000 |
| Pair 3 Foramen. Post_6–Foramen. Post_12m | 0.470 | 0.915 | 0.288 | 0.652 | 0.000 |
| Pair 4 Foramen. Post_12–Foramen. Post_18m | 0.364 | 0.797 | 0.168 | 0.560 | 0.000 |
| Pair 5 Foramen. Post_18–Foramen. Post_24m | 0.125 | 0.336 | 0.004 | 0.246 | 0.044 |
The XLIF technique is an anterior arthrodesis technique via a lateral transpsoas approach, first described by Pimenta9 in 2001 reporting more than 100 transpsoas operations at that time since 1998. Several authors have reported their results (Table 3) since the publication of the surgical technique by Ozgur et al.10 until the present date.
Several authors have reported their results (Table 3) since the publication of the surgical technique by Ozgur to the present date.
| Author | Year | Series | Disease | Conclusions |
|---|---|---|---|---|
| Rodgers et al.20 | 2007 | 100 patients | Degenerative | A safe technique, with a really low rate of complications (2%) and significant clinical improvement on the VAS scale (68% improvement) |
| Anand et al.22 | 2008 | 12 patients | Deformity | Minimally invasive procedures (XLIF) less blood loss and greater pain improvement compared to conventional techniques |
| Knight et al.23 | 2009 | 58 patients | Degenerative | Rate of complications of 22.4% half of which were associated with the approach route. They describe 3.4% motor neurological injury with improvement at 1 year and other “major” complications. They indicate that mortality using the extreme lateral technique was less than that of other traditional techniques |
| Rodgers et al.24 | 2009 | 100 patients | Adjacent segment | Report excellent results with a complications rate of 9% and only 1% symptoms related to dysesthesia and weakness at the level of the upper third of the thigh ipsilateral to the approach side |
| Oliveira et al.25 | 2010 | 15 patients | Stand- alone XLIF using BMP | Low rate of complications (6.7%) 100% fusion demonstrated by CAT |
| Rodgers et al.11 | 2010 | 300 patients | XLIF obese and non-obese | They did not find significant differences between the two groups and concluded that patient satisfaction exceeded 89% |
| Ozgur et al.26 | 2010 | 62 patients, 113 segments | Degenerative | 19% minor complications and none considered major. Fusion was achieved in 91% of cases |
| Oliveira et al.27 | 2010 | 21 patients | Degenerative | Highlight the indirect decompression of the neurological elements |
| Anand et al.28 | 2010 | 28 patients | Degenerative | All the patients maintained the correction with 57% improvement on the VAS scale |
| Dakwar et al.29 | 2010 | 25 patients | Adult deformity | Both the surgery time (a mean of 108min) estimated blood loss per patient (53ml) were extremely low, with a 20% rate of minor complications and major complications of 4% and a reduction in the VAS score of 70.4% |
| Wang and Mummaneni30 | 2010 | 23 patients | Adult deformity using XLIF bilateral percutaneous screws and BMP | The incidence of problems in the anterior face of the thigh ipsilateral to the XLIF surgery was 30% and the fusion rate confirmed by CAT was 100% |
| Tormenti et al.21 | 2010 | 8 patients | Adult scoliosis XLIF with posterior percutaneous screws compared to subsequent techniques alone (PLIF or TLIF) | Confirming a much greater correction capacity with the XLIF procedure (70.2% compared to 44.7%). However the high rate of complications is noteworthy: 75% of the patients experienced symptoms in the proximal third of the thigh and 25% presented motor injuries. They also reported the onset of other major complications such as: intestinal perforation, pleural effusion, paralytic ileus and pulmonary thromboembolism |
| Rodgers et al.4 | 2010 | 600 patients, 741 levels operated | Degenerative | The reported rate of complications was 6.2%. The low rate of neurological complications (0.7%) is worthy of note, all of which were transient |
| Sharma et al.31 | 2011 | 43 patients | Degenerative | Concluding that after 1 year follow-up a gain of 3.7° on the coronal plane and 2.8° on the sagittal plane per segment operated with 25% of symptoms in the proximal third of the thigh |
| Uribe et al.32 | 2012 | – | Experimental | Achieving good correction of the deformity exposing the necessity to use more aggressive procedures such as Smith Petersen and/or pedicle subtraction osteotomy. |
| Pimenta et al.33 | 2013 | 30 patients | Prospective and randomised prospective study stand-alone XLIF with tricalcium phosphate compared with BMP | Fusion was achieved in both groups with only one case where the bone formation in the BMP group made reoperation necessary |
| Meredith et al.34 | 2013 | 18 patients and 32 levels operated | XLIF in the thoracic and thoracolumbar area | 100% fusions. The authors agree that at this level this procedure offers two very significant advantages: an approach surgeon is not necessary for the operation neither is selective pulmonary intubation to enable access to the disc space |
| Malham et al.35 | 2014 | 30 patients | XLIF prospective, non-randomised study | Significant improvement in intervertebral disc height with a 100% fusion rate |
With regard to clinical results, because this is a general review of patients with different disorders it is true that the final outcomes are difficult to evaluate. We consider this review interesting because, despite the persistent VAS score in the leg, there was improvement of 42%. This appears to us a hopeful outcome, despite the diversity of diseases, because we believe that patients with a VAS score of 5 or less usually decide not to undergo an operation.
With regard to the analysis of our major surgical complications, it is worth mentioning that there are several authors that report motor injury in the side ipsilateral to the approach side.4,11 All due to retraction and/or compression of the nerve in approaching the disc (especially at level L4–L5). However, injuries occurring on the contralateral side appear less likely, at least in theory. Nevertheless, Taher et al.12 report up to 3.4%; they attribute these to over distraction, or displacement of a disc fragment towards the foramen. Although not common, vascular injuries13–19 can occur, especially if there are large deformities in the spine. Vascular complications after the transpsoas XLIF procedure are rare since the approach used means that the vessels are relatively distant from the approach route. The abdominal hernia related to defective closure of the abdominal fascia and was associated with major obesity. Injury to the ilioinguinal nerve when making the abdominal muscle incision can cause paralysis of the musculature at this level triggering bulging. We had no case in the series presented. There are few published articles that refer to complications. Apart from the series by Rodgers et al.20 reporting 2% of total complications and the study by Tormenti et al.21 with 150%, the remainder report complications11,22–29 ranging around 25%. This is consistent with the abovementioned experience of HCSC.
On analysis of the clinical–radiological outcomes, the statistical study of the progress of the disc and foraminal heights shows that after surgery all levels operated gained in height enabling the indirect decompression of the posterior elements, which is consistent with the literature and with the clinical outcomes obtained. It is worth highlighting that considering movement of the implant as pseudoarthrosis, the failure rate of the arthrodesis was 1%, this figure is similar to that of the most recent series published.29–35 We found no references on this point. We believe that the infradimension of the implant size in terms of both its height and its width plays a key role in the onset of this complication. It is nonetheless remarkable that movement with clinical repercussions and six paucisymptomatic implant movements presented even when percutaneous screws via a posterior route were used. It appears clear that the only situation where we found no movement was when we used a “mini-plate” via a lateral route.
Conclusions- -
The XLIF procedure is an anterior arthrodesis technique via a lateral transpsoas approach.
- -
An approach surgeon is not needed for the procedure.
- -
Intraoperative neurophysiological monitoring is essential to reduce the rate of complications that derive from the approach route.
- -
Clinical improvement is important from a clinical and a radiological perspective.
- -
The rate of major complications is low compared to that of other lumbar arthrodesis procedures.
- -
The major complications can be resolved relatively easily.
- -
The XLIF procedure constitutes a safe and reliable alternative when planning a minimally invasive lumbar arthrodesis.
Level of evidence II.
Ethical responsibilitiesProtection of people and animalsThe authors declare that neither human nor animal testing have been carried out under this research
Data confidentialityThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors declare that no patients’ data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Domínguez I, Luque R, Noriega M, Rey J, Alia J, Marco-Martínez F. Artrodesis intersomática lumbar extralateral. Técnica quirúrgica, resultados y complicaciones con un seguimiento mínimo de un año. Rev Esp Cir Ortop Traumatol. 2017;61:8–18.