The oropharyngeal dysphagia is a frequently present side effect amongst cerebrovascular pathology, being quite relevant due to the possible respiratory and/or nutritional side effects.
ObjectiveTo know the prevalence of oropharyngeal dysphagia in hospitalized-stroke patients within a neurorehabilitation unit.
MethodA cross-sectional study was designed whose target population was patients diagnosed of cerebrovascular pathology hospitalized in the neurorehabilitation unit within a mid/long term stay hospital in Madrid, Spain, from April 1st 2012 until January 31st 2015. Social-demographical and clinical variables have been chosen by checking the clinical records from the patients included.
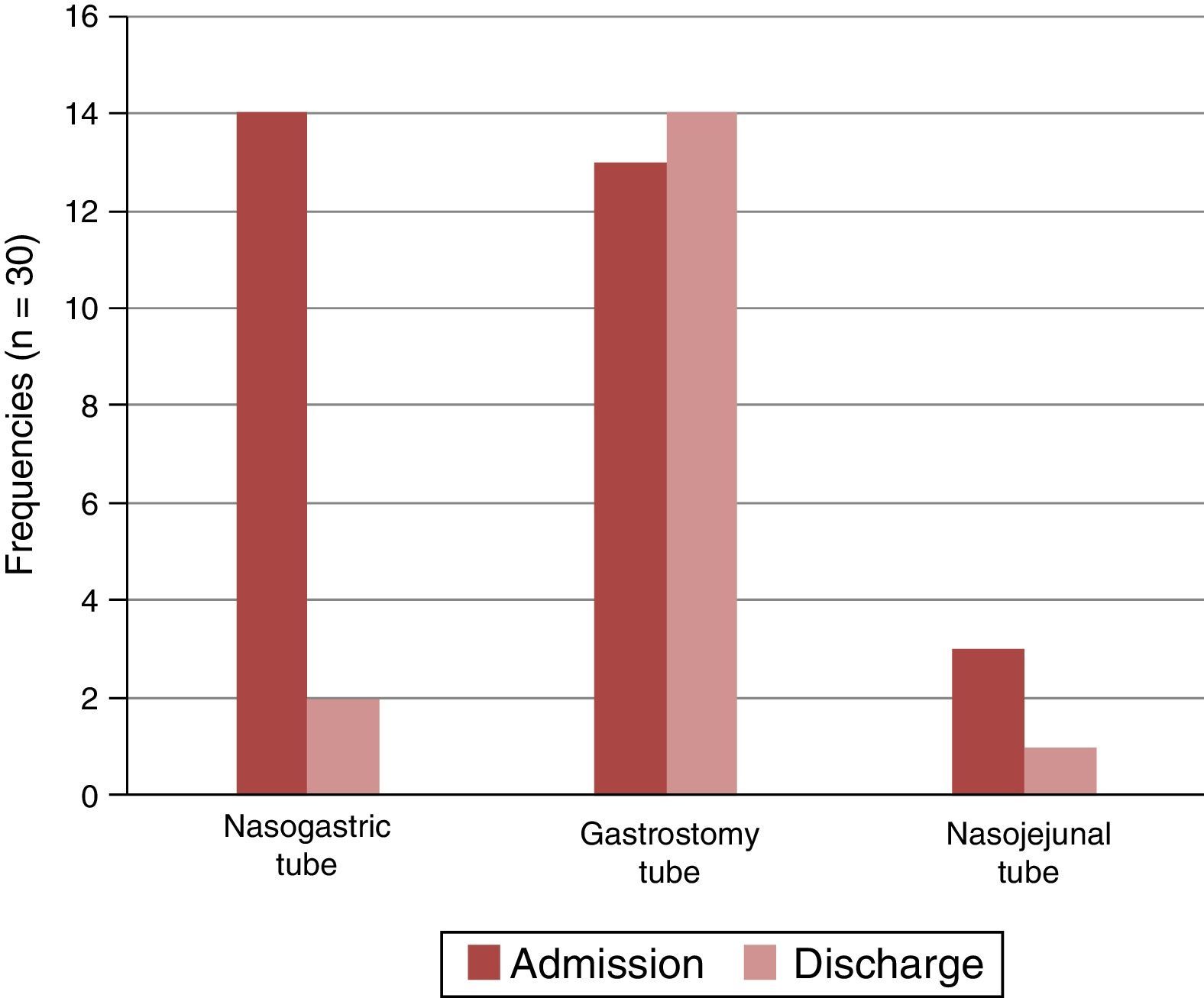
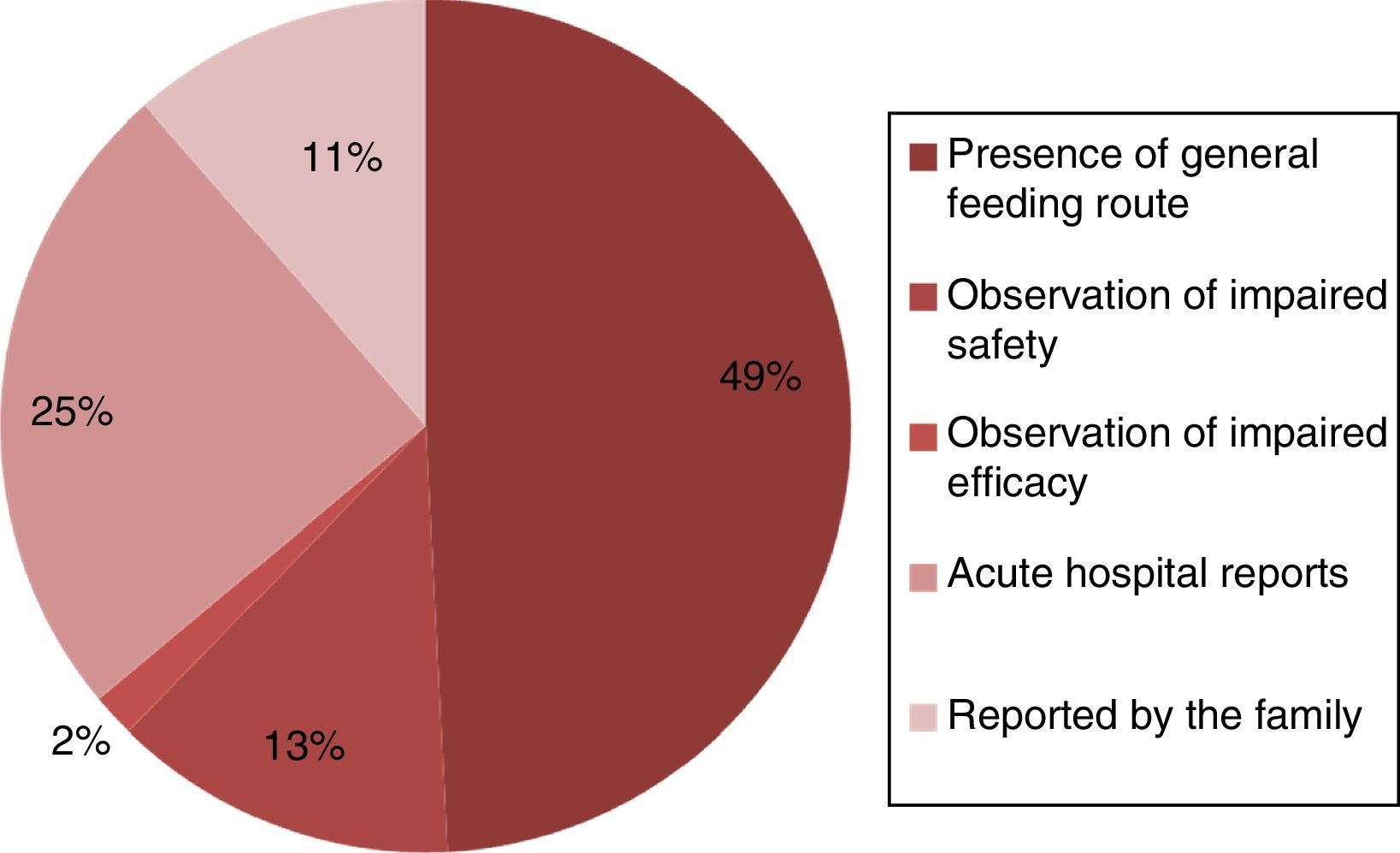
ResultsDuring the period time of the study 124 patients were admitted in the unit, amongst those 88 were male. A big part of the patients with oropharyngeal dysphagia were admitted with a diagnosis of focal-ischaemic stroke, 43.1% (n=58), and 39.7% (n=49) with intracerebral haemorrhagic stroke. It was also verified that 79.3% (n=46) of the patients diagnosed with dysphagia presented a total dependency, 17.3% (n=10) severe helplessness and 3.4% (n=2) moderate dependence in daily activities.
ConclusionDysphagia has a high prevalence within our unit and it is related to the degree of patient dependence related to life actions and, being recommended the use of the Volume–Viscosity Swallow Test when dealing with patients with stroke in order to identify early diagnosis.
La disfagia orofaríngea es una secuela que está presente de forma muy frecuente en la patología cerebrovascular, y es importante dadas las complicaciones que puede presentar a nivel respiratorio y/o nutricional.
ObjetivoConocer la prevalencia de disfagia orofaríngea en pacientes con ictus hospitalizados en una unidad de neurorrehabilitación.
MétodoEstudio descriptivo transversal, teniendo como población accesible a los pacientes diagnosticados de patología cerebrovascular ingresados en la unidad de neurorrehabilitación de un hospital de media-larga estancia de Madrid en el periodo comprendido entre el 1 de abril de 2012 al 31 de enero de 2015. Se han recogido variables tanto sociodemográficas como clínicas a través de la consulta de historias clínicas de los pacientes incluidos en el estudio.
ResultadosEn el periodo de estudio ingresaron 124 pacientes en la unidad, de los cuales 88 eran varones. Se presenta una prevalencia de disfagia orofaríngea del 46,8% (n=58). Gran parte de los pacientes con disfagia orofaríngea han ingresado con diagnóstico principal de accidente cerebrovascular de origen isquémico focal (43,1%; n=52) y un 39,7% (n=49) con diagnóstico de ictus hemorrágico intraparenquimatoso. Asimismo, verificamos que el 79,3% (n=46) de los pacientes diagnosticados de disfagia presentan un nivel de dependencia total, el 17,3% (n=10) dependencia severa y el 3,4% (n=2) dependencia moderada para las actividades básicas de la vida diaria.
ConclusiónLa prevalencia de disfagia en nuestra unidad es alta, objetivando también una posible relación con el grado de dependencia para las actividades básicas de la vida diaria de los pacientes, siendo recomendable la realización del Método de Exploración Clínica Volumen-Viscosidad a los pacientes con ictus con el propósito de realizar un diagnóstico precoz de este trastorno.