Currently, the assessment of lymphoedema related to breast cancer (BCRL) is performed through the global perimeter volumetry. We implemented an additional system with partial measures (hand, forearm, and upper arm) that allows us to approximate the segmental distribution of oedema. We used this measurement tool to determine the oedema distribution and its evolution, as well as its possible impact on clinical assessment.
MethodsWe carried out a retrospective observational study of the patients referred to our service with suspected BCRL.
Inclusion criteriaUnilateral breast cancer, availability of global and partial digital medical record, and follow-up for a minimum of 24 months.
Of the 210 selected patients, 190 were considered affected (≥10% excess volume). We analysed at three time points (initial, final, and peak involvement) the oedema distribution and segmental predominance and its relationship with the evolutionary course and the severity of the process. We subsequently examined, at the initial timepoint, the concordance of the global assessment with the partial assessment for the clinical classification of the 210 patients in the initial sample.
ResultsThe BCRL oedema was characteristically irregular, with the forearm being the most affected segment and the hand the least affected (RM ANOVA: p<0.001). The irregularity was related to its severity (χ2: p<0.001) and the evolutionary course (Student t-test: p<0.005 for the hand). Overall, disagreement of 46.67% was observed between the clinical classification of the global and partial assessment.
ConclusionsThis work supports the need to add partial volumetry to the commonly used global assessment.
Actualmente la volumetría perimetral global se utiliza para valorar el linfedema relacionado con cáncer de mama (LRCM). Nosotros implementamos un sistema adicional que permite aproximarse a la distribución segmentaria del edema mediante tres indicadores parciales: mano, antebrazo y brazo. Utilizamos esta herramienta para conocer la distribución del edema, su evolución y su posible repercusión en la valoración clínica.
MetodologíaSe realizó un estudio observacional retrospectivo de los pacientes remitidos a nuestro servicio con sospecha de LRCM.
Criterios de inclusiónCáncer de mama unilateral, con registros volumétricos en la historia clínica digital y 24 meses de seguimiento mínimo.
De los 210 pacientes seleccionados, en 190 pacientes afectos (≥10% de exceso de volumen) se analizaron en tres momentos de medición (inicial, final y máxima afectación) la distribución del edema, su predominio segmentario y la relación con la evolución y la gravedad del proceso. Posteriormente se examinó la concordancia de los indicadores globales con los parciales en la valoración clínica de los 210 pacientes de la muestra inicial.
ResultadosEl LRCM fue característicamente irregular, siendo el antebrazo el segmento predominante y la mano el menos afecto (MR ANOVA: p<0,001). La irregularidad se relacionó con la gravedad del proceso (chi cuadrado: p<0,001) y su evolución (t de Student: p<0,005 para la mano). Además, se apreció, en conjunto, una discordancia en la valoración clínica del índice global con los índices parciales del 46,67% (W de Kendall=0,467).
ConclusiónEl estudio apoya la necesidad de añadir volumetría parcial a la valoración global habitualmente utilizada.
Limb swelling is usually the first clinical manifestation of breast cancer-related lymphoedema (BCRL) and is the only persistent symptom throughout the entire clinical course. Thus, measuring its dimensions is key to identifying the clinical suspicion, diagnosis, and evaluation of lymphoedema. Perimetral assessment are currently used to obtain global upper limb measurements. Therefore, despite the fact that the irregularity of the oedema in BCRL has been pointed out, no studies have yet been carried out in a wide population of patients to measure its distribution in the various anatomical segments of the limb. We designed a measurement method that includes partial calculations to approximate the segmental concentration of oedema. The objectives of this study were, through a retrospective review:
- (1)
To understand the distribution of oedema in BCRL and to verify if there is a typical presentation pattern.
- (2)
To assess the influence of factors such as the severity of the process and the evolution time.
- (3)
We also aimed to analyse the impact of the irregularity of lymphoedema on clinical assessments.
We conducted a retrospective study of all patients referred for suspected BCRL. The first records in the digital clinical history were dated from December 2006. All these patients were followed up, regardless of whether they were initially diagnosed with lymphoedema. To assess both the distribution of the oedema at a given moment, as well as its evolution and severity over time, we included patients with unilateral breast cancer with global and partial volumetric digital medical records and a minimum follow-up period of 24 months. All the patients diagnosed with BCRL received the treatments considered necessary based on their clinical situation throughout the entire clinical course of their disease.
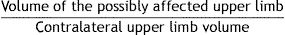
Our method, comparatively measure the perimeters in both limbs with a tape measure. We do it with the patient in a sitting position, at 45° of shoulder antepulsion, with the forearm pronated, and with the elbow, wrist and hand in full extension. We start behind the metacarpophalangeal joints of the hand and taking the base of the nail of the third finger as a reference point to adjust the first mark. We then continue at fixed distances of 4cm, distal to proximal, without exceeding the limit of the axillary fold. Thus, we obtain a variable number of measurements, limited to 14, depending on the length of the limb. Next, by applying the cylinder formula (P2/π for distances of 4cm), we obtain the estimated total volumes, and by comparing both limbs, we calculate the global volume ratio (GVR). The formula used in this calculation is:
Subtracting 1 from this ratio and multiply the result by 100, the global excess volume in percentage (GEV) of the possibly affected member is obtained.
We use a common diagnostic criterion for the BCRL, an GEV ≥10% (GVR≥1.1). Severity is determined according to the classification accepted by the International Society of Lymphology (ISL) criteria,1 where mild cases show GEV <20% (GVR<1.2), moderate GEV 20–40% (GVR 1.2–1.4), and severe GEV >40% (GVR>1.4). In addition, to the GVR and the GEV we have implemented a partial calculation – the partial volume ratio (PVR) and the partial excess volume (PEV) – of the three segments of the limb (hands, forearms, and upper arm). With the first and second perimeters we obtain the ratio and excess volume of the hand segment, with the third to seventh measurements we calculate those referred to the forearm segment, and the ninth measurement onwards give those of the upper arm segment. We exclude the eighth measurement from this standardised calculation because its segment position is variable. Finally, we calculate each partial ratio by applying the same process as described for the global ratios. Since we have the partial indicators, we rely on them for the clinical assessment of the BCRL.
Study characteristicsData collection was done using a Microsoft Excel 2016 spreadsheet. In addition to the data of the object of study, data was collected on sex, age, laterality of breast cancer, follow-up time, type of breast surgery and radiotherapy treatment were collected.
For the study of distribution of oedema and its evolution, given that the oedema volumes frequently vary in patients with BCRL throughout their clinical course, the patients who at some point during follow-up showed a global and/or partial excess volume ≥10% were included.
Measurement data were recorded at three time points: at the initial assessment, final assessment, and time of peak involvement (which, in some cases, coincided with the first or last measurement). To study the distribution of the oedema and the possible existence of a typical distribution pattern, in addition to the means of the ratios in each segment, we also assessed, through their partial excesses volume, the segmental predominance in each patient (which segment predominated, according to the partial excess volumes).
The comparison between the initial and final measurements helped us to know the influence of the evolution time on the irregularity of lymphoedema.
The time of maximal involvement was specifically used to relate the irregularity of the lymphoedema to the severity of the process.
The study of clinical-diagnostic agreement was carried out in the initial measurement, when the first clinical assessment of the patient had originally been established. We compared the global volume excess in all the selected patients to the maximum partial volume excess to analyse the degree of coincidence or divergence of clinic assessment (diagnosis and the severity classification).
Statistical analysisThe analysis of our data showed that our samples were highly skewed to the right due to extreme values of severely affected patients. The Kolmogorov–Smirnov test found non-normal distribution in 9 of the 12 variables. In the case of variables of considerable size with unequal variances, we rejected the application of non-parametric tests.2 We carried out a transformation of our data, testing the BOX COX family of transformations,3 of which only the reciprocal transformation normalised all the samples.
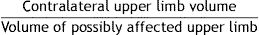
In our case, the inverse transformation corresponds to the inverse measurement of the volume, that is:
Subtracting this inversed volume ratio from 1 and multiply the result by 100, we obtain the volume defect in percentage of the unaffected limb, the inverse way of evaluating the differences between both limbs. The same formulas were applied to each of the partial segments.
The statistical studies were performed in these variables of inverse volumetry, with normal distribution.
We carried out correlational analysis of all variables through Pearson coefficient.
Since our samples are related, for the inference studies we used the Repeated Measures ANOVA (RM ANOVA) for the oedema distribution study. We performed the Mauchly test for checking the variances and when the sphericity condition was not satisfied, we applied the Greenhouse–Geisser test. The comparison between the initial and final measurements was performed through the Student t-test.
For the relationship between the segmentary predominance and the severity of process, we used the chi square test.
Finally, in the concordance study, we carried out the calculation of the Kendall coefficient of concordance.
All these statistical analyses were implemented using SPSS software (version 19.0; IBM Corp., Armonk, NY).
Ethical approvalThis study was approved by the local ethics committee.
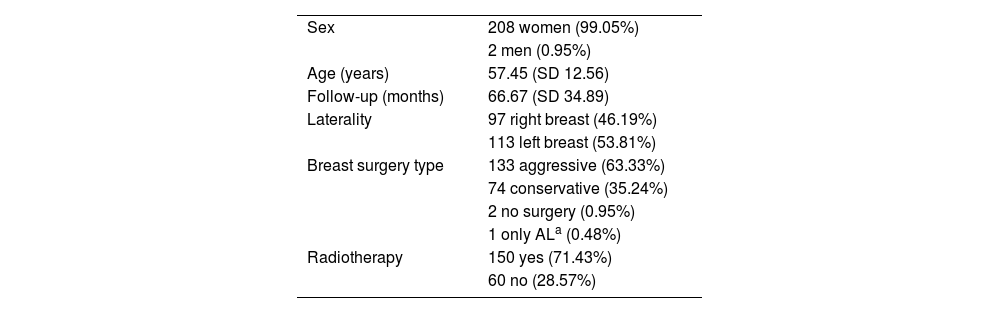
ResultsThe final sample included 210 patients and the general data for this sample are summarised in Table 1. Two individuals were male (0.95%). Three patients had not undergone a mastectomy, two because they had metastatic cancer and one because she had a primary lymph node tumour and had only undergone axillary lymphadenectomy. The mean follow-up time exceeded 5 years.
General sample data, n=210.
| Sex | 208 women (99.05%) |
| 2 men (0.95%) | |
| Age (years) | 57.45 (SD 12.56) |
| Follow-up (months) | 66.67 (SD 34.89) |
| Laterality | 97 right breast (46.19%) |
| 113 left breast (53.81%) | |
| Breast surgery type | 133 aggressive (63.33%) |
| 74 conservative (35.24%) | |
| 2 no surgery (0.95%) | |
| 1 only ALa (0.48%) | |
| Radiotherapy | 150 yes (71.43%) |
| 60 no (28.57%) |
Of the 210 patients, the oedema remained below a level of 10% excess volume during the entire follow-up (an average of 57.1 months) in 20 cases (9.52%). These patients were considered non-lymphoedemic and were excluded from our analyses of the distribution and evolution of oedema.
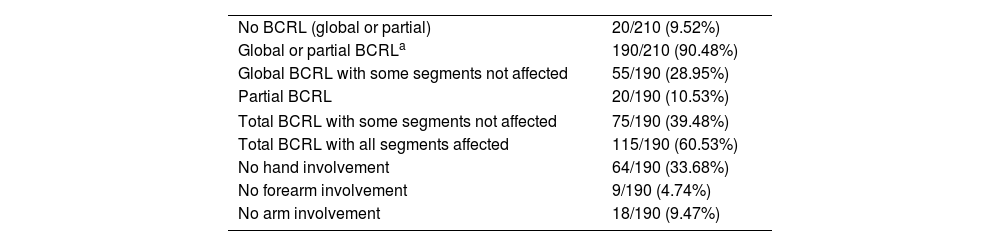
The characteristics of global or partial involvement throughout the entire follow-up are shown in Table 2. Twenty patients (10.53%) presented partial lymphoedema (PL) exceeding a 10% excess volume only in some of the partial indices (with GEV<10%), while 55 patients with global lymphoedema (GEV≥10%) showed some segments that were oedema-free. The hand remained oedema-free (an excess volume <10%) throughout the follow-up in 64 patients (33.68%), compared to 18 (9.47%) in which there was no upper arm lymphoedema and 9 (4.74%) without forearm lymphoedema.
Global or partial involvement characteristics over the whole patient evolution. Total number of patients: 210 patients with lymphoedema: 190 (results shown as the number of patients and %).
| No BCRL (global or partial) | 20/210 (9.52%) |
| Global or partial BCRLa | 190/210 (90.48%) |
| Global BCRL with some segments not affected | 55/190 (28.95%) |
| Partial BCRL | 20/190 (10.53%) |
| Total BCRL with some segments not affected | 75/190 (39.48%) |
| Total BCRL with all segments affected | 115/190 (60.53%) |
| No hand involvement | 64/190 (33.68%) |
| No forearm involvement | 9/190 (4.74%) |
| No arm involvement | 18/190 (9.47%) |
The 190 patients who showed global or partial measurements equal to or greater than 10% excess volume at some point during follow-up were considered BCRL patients and became part of the study group for the oedema distribution.
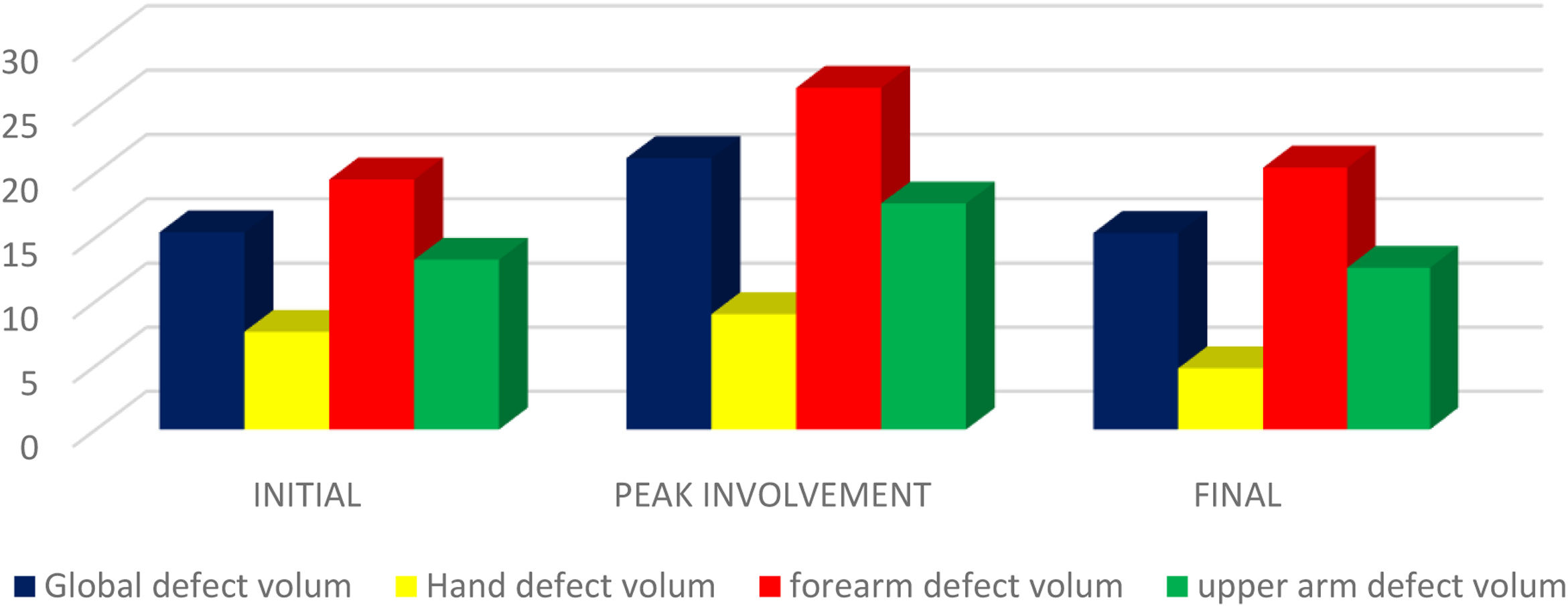
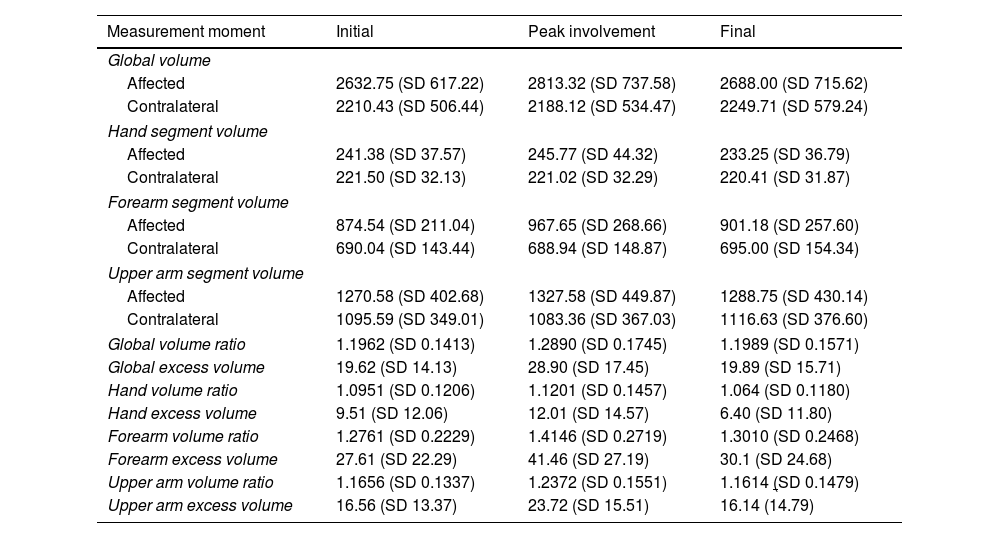
The data of the direct and inverse volumetry are shown in Tables 3 and 4. In both, the forearm ratios were highest at all three measurement time points, with means that always exceeded those of the global ratios at magnitudes that were quasi-proportional to them. On the contrary, the hand ratios were the least affected at all three measurement time points. Moreover, this distribution pattern had tended to increase by the final measurement compared to the initial one.
Mean and SD of global and partial volumes, volume ratios (in c.c.) and volume excess (in %), n=190.
| Measurement moment | Initial | Peak involvement | Final |
|---|---|---|---|
| Global volume | |||
| Affected | 2632.75 (SD 617.22) | 2813.32 (SD 737.58) | 2688.00 (SD 715.62) |
| Contralateral | 2210.43 (SD 506.44) | 2188.12 (SD 534.47) | 2249.71 (SD 579.24) |
| Hand segment volume | |||
| Affected | 241.38 (SD 37.57) | 245.77 (SD 44.32) | 233.25 (SD 36.79) |
| Contralateral | 221.50 (SD 32.13) | 221.02 (SD 32.29) | 220.41 (SD 31.87) |
| Forearm segment volume | |||
| Affected | 874.54 (SD 211.04) | 967.65 (SD 268.66) | 901.18 (SD 257.60) |
| Contralateral | 690.04 (SD 143.44) | 688.94 (SD 148.87) | 695.00 (SD 154.34) |
| Upper arm segment volume | |||
| Affected | 1270.58 (SD 402.68) | 1327.58 (SD 449.87) | 1288.75 (SD 430.14) |
| Contralateral | 1095.59 (SD 349.01) | 1083.36 (SD 367.03) | 1116.63 (SD 376.60) |
| Global volume ratio | 1.1962 (SD 0.1413) | 1.2890 (SD 0.1745) | 1.1989 (SD 0.1571) |
| Global excess volume | 19.62 (SD 14.13) | 28.90 (SD 17.45) | 19.89 (SD 15.71) |
| Hand volume ratio | 1.0951 (SD 0.1206) | 1.1201 (SD 0.1457) | 1.064 (SD 0.1180) |
| Hand excess volume | 9.51 (SD 12.06) | 12.01 (SD 14.57) | 6.40 (SD 11.80) |
| Forearm volume ratio | 1.2761 (SD 0.2229) | 1.4146 (SD 0.2719) | 1.3010 (SD 0.2468) |
| Forearm excess volume | 27.61 (SD 22.29) | 41.46 (SD 27.19) | 30.1 (SD 24.68) |
| Upper arm volume ratio | 1.1656 (SD 0.1337) | 1.2372 (SD 0.1551) | 1.1614 (SD 0.1479) |
| Upper arm excess volume | 16.56 (SD 13.37) | 23.72 (SD 15.51) | 16.14 (14.79) |
The volume ratios are expressed in 4 decimals to make visible than the decimal part corresponds to excess volume.
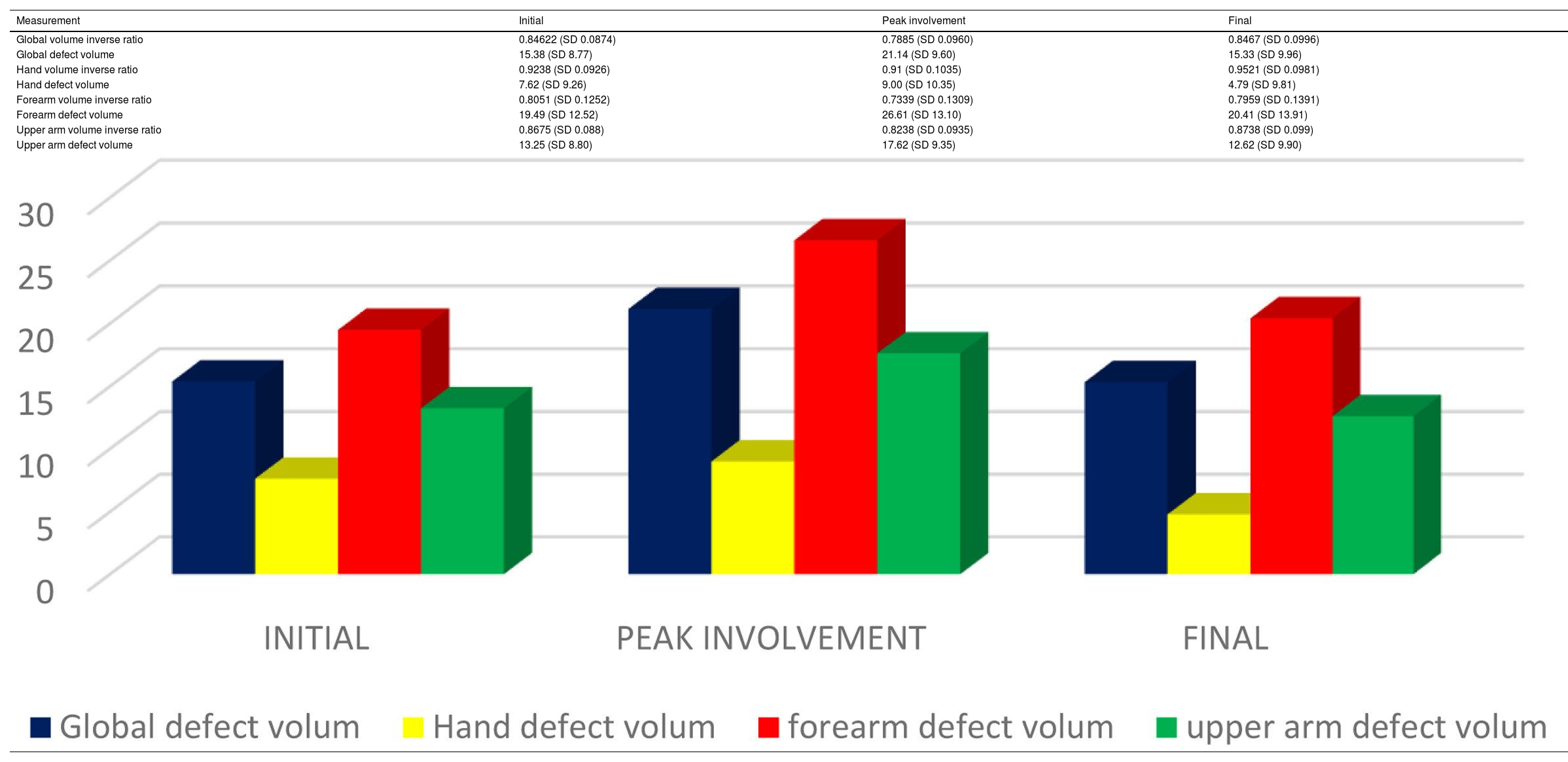
(With graph): mean and SD of inverse ratios and volume defect of non affected limb (volume defect in %), n=190.
| Measurement | Initial | Peak involvement | Final |
|---|---|---|---|
| Global volume inverse ratio | 0.84622 (SD 0.0874) | 0.7885 (SD 0.0960) | 0.8467 (SD 0.0996) |
| Global defect volume | 15.38 (SD 8.77) | 21.14 (SD 9.60) | 15.33 (SD 9.96) |
| Hand volume inverse ratio | 0.9238 (SD 0.0926) | 0.91 (SD 0.1035) | 0.9521 (SD 0.0981) |
| Hand defect volume | 7.62 (SD 9.26) | 9.00 (SD 10.35) | 4.79 (SD 9.81) |
| Forearm volume inverse ratio | 0.8051 (SD 0.1252) | 0.7339 (SD 0.1309) | 0.7959 (SD 0.1391) |
| Forearm defect volume | 19.49 (SD 12.52) | 26.61 (SD 13.10) | 20.41 (SD 13.91) |
| Upper arm volume inverse ratio | 0.8675 (SD 0.088) | 0.8238 (SD 0.0935) | 0.8738 (SD 0.099) |
| Upper arm defect volume | 13.25 (SD 8.80) | 17.62 (SD 9.35) | 12.62 (SD 9.90) |
Regarding the segmentary predominance, the forearm was a predominant segment in 125 patients (65.75%) in initial measurement, 137 (72.1%) in final measurement and 150 (78.95%) in peak involvement moment. The hand segment was at the other end with segmentary predominance in 17 patients (8.5%) at the beginning, 11 (5.79%) in the final evaluation and only 7 (3.68) in peak involvement.
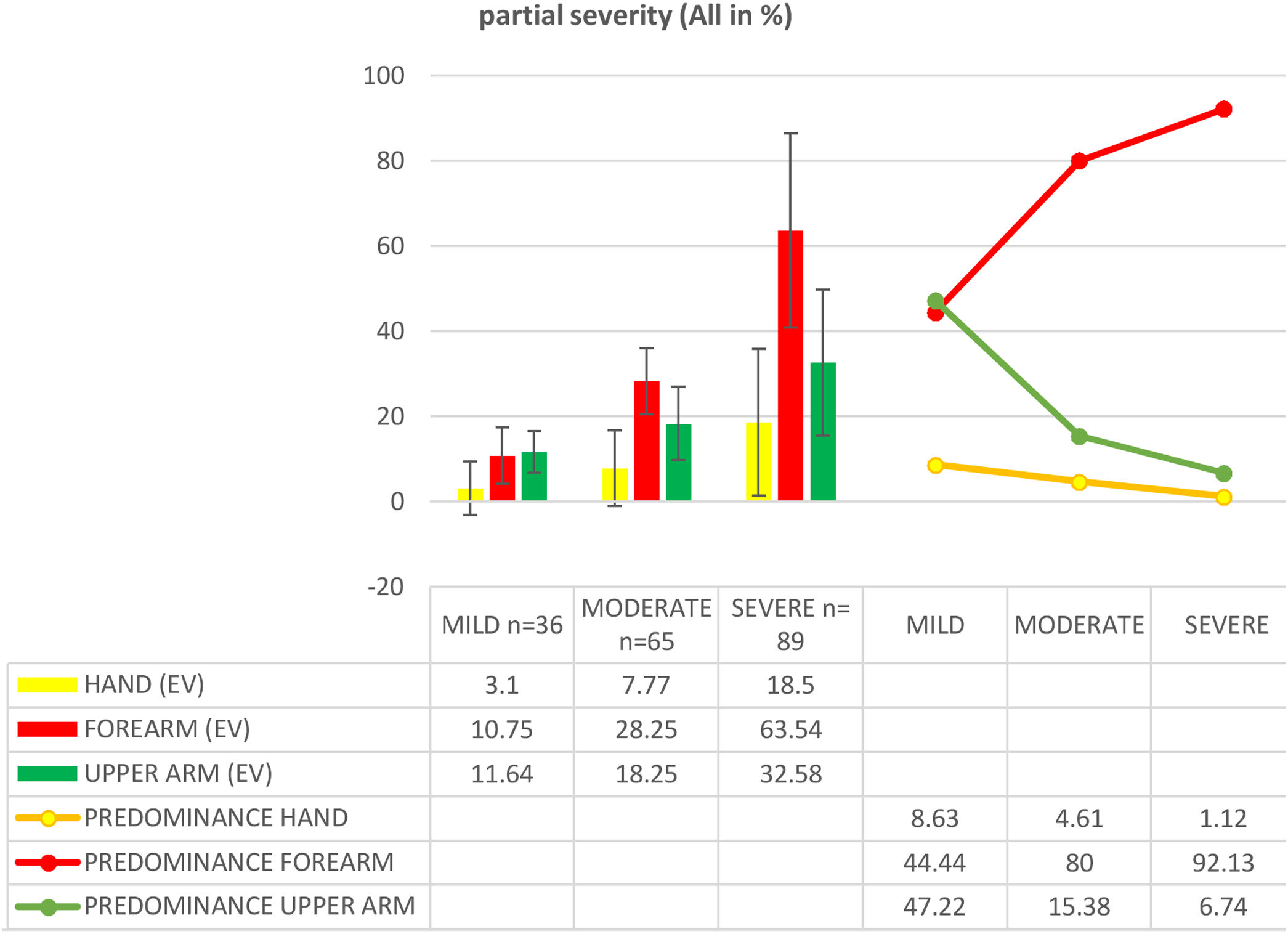
The distribution and the segmentary predominance of oedema according to the severity groups at the time of peak involvement of the oedema also showed a close relationship between this pattern and the severity of the process (Graph 1).
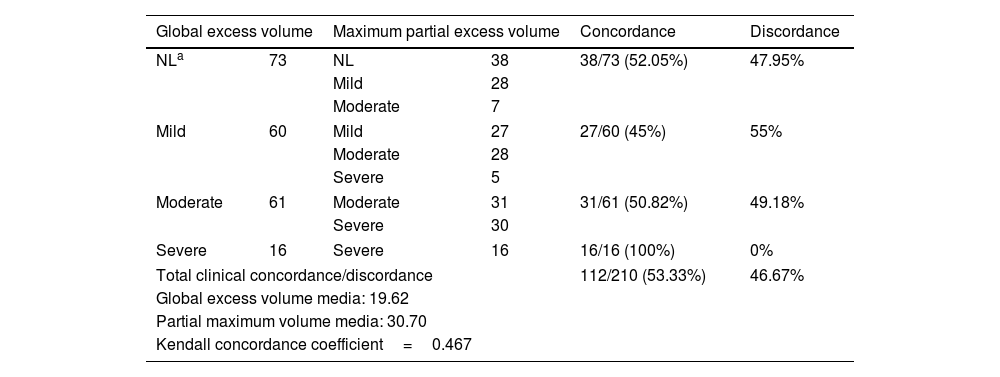
Finally, data for the comparison and concordance between global and partial ratios in the initial measurement are shown in Table 5. The concordance of clinical assessment between the global excess volume and the maximum partial volume excess (classification as no lymphoedema or mild, moderate or severe lymphoedema) was 53.33%, thereby corresponding to divergence of 46.67%.
Concordance of the clinical assessment between the global measurement and partial measurements in terms of the number of patients and % (initial measurement), n=210.
| Global excess volume | Maximum partial excess volume | Concordance | Discordance | ||
|---|---|---|---|---|---|
| NLa | 73 | NL | 38 | 38/73 (52.05%) | 47.95% |
| Mild | 28 | ||||
| Moderate | 7 | ||||
| Mild | 60 | Mild | 27 | 27/60 (45%) | 55% |
| Moderate | 28 | ||||
| Severe | 5 | ||||
| Moderate | 61 | Moderate | 31 | 31/61 (50.82%) | 49.18% |
| Severe | 30 | ||||
| Severe | 16 | Severe | 16 | 16/16 (100%) | 0% |
| Total clinical concordance/discordance | 112/210 (53.33%) | 46.67% | |||
| Global excess volume media: 19.62 | |||||
| Partial maximum volume media: 30.70 | |||||
| Kendall concordance coefficient=0.467 | |||||
Regarding the correlation, it was positive among all the indicators global and partial. The highest Pearson coefficients for the global excess volume were obtained with the forearm excess volume (0.812–0.913) and the lowest with the hand excess volume (0.458–0.554). Comparing partial segments against each other sheds the highest correlation between forearm and arm (0.548–0.621) and the lowest between hand and arm (0.232–0.384).
The comparison of the three partial indicators through RM ANOVA shows that the excess volume is affected by the segmental distribution in the three measurement moments (p<0.001) and also in the pairwise comparisons (p<0.001).
Regarding the influence of the evolution time, Student t-tests for paired samples found significant differences between the initial and final values for the hand (p<0.005).
In the peak involvement measurement moment, the segmental predominance according to the severity of the process showed a chi square test also highly significant (p<0.001).
As to as the clinical concordance study between global and partial assessment, the Kendall coefficient of concordance was 0.467.
DiscussionOur measurement method is performed using perimetry because it is a simple and reliable method that can adequately distinguish oedema for the assessment of BCRL.4–10 Taking into account not only its reliability, but also its availability and execution time, it could be considered the gold standard test for assessing BCRL.7 We draw on the disk model to transform the perimeter measurements into volumes. Use of the frustum model (truncated cone) formula seems to have prevailed in the literature to date due to its apparent logic regarding the shape of the upper limbs, with standardised measuring instruments available for it.10 However, all the studies that confront both methods with water displacement do so on the absolute volumes of the limbs and never on the comparative figures. Other aspects such as the elliptical shape of the limb that can decrease the volumetric calculation by up to 5%11 and approximate it to one or another formula are not taken into account. Sitzia12 made a comparison between the volume percentages obtained with the two methods, finding an absolute mean difference of 1.5%, but this difference corresponded to a mean volume of 53.7%, which implies a relative mean difference lower than 3%. In addition, he made a relevant error because his adjustment of the cylinder formula to the same segment that is used in the truncated cone did not modify the volume percentages, when they should be different. In our experience, when the cylinder formula is calculated with one less segment, the differences are considerably reduced. Neither did he confront excess volume percentages with supposedly more objective methods. He assumed the superiority of the frustum method due to its similarity to the shape of the limb. Moreover, in his conclusions he recommended for later studies to compare the percentages obtained from the perimeters with real image studies. Various authors support and continue to use the cylinder formula for both clinical and experimental studies.13–16 While using comparative indicators and with a considerable number of measurement points (in our case every 4cm) to avoid bias,17 the differences between both formulas does not significantly impact on the assessment of lymphoedema.
Based on the standard whole limb assessment system, we implemented additional calculations that allow us to partially assess the anatomical areas of the upper limbs. Although the regular interval method we use is an excellent clinical tool because of its speed, it presents drawbacks when it comes to partial measurements. The perimeter markings change for each patient depending on the limb length, so that a segment of the same length does not necessarily correspond to the same anatomical segment in different patients. Using our measurement system, measurement 8 is located around the elbow joint, an area often affected by oedema.18–20
However, this point could be located from the proximal forearm to the distal arm, meaning that it should be excluded from the standardised partial calculation. In some cases, this may lead to some measurement bias, especially in the upper arm of short limbs and in the forearm of long limbs. Although measurements adjusted to bone references would eliminate this problem, the method would be more complex if we also wanted to maintain the number of measurements recorded, for the sake of greater comparison accuracy. Thus, it should be made clear that our method is a clinical tool and that the partial assessment is not intended to exactly calculate the volume of the anatomical segments of both limbs, but rather to establish a reliable comparison between them to obtain an approximation of their involvement.
The 10% criterion, which we chose as a relative criterion for the diagnosis of BCRL, has also been endorsed by various authors as a cut-off for diagnosis.19,21,22 In contrast, the absolute criteria (perimeter difference of 2cm or difference in volume of 200ml) seemed inadequate, given the individual variability in limbs.23 Along these lines, normative studies carried out in a healthy population that analysed these criteria showed different cut-off points for the diagnosis of BCRL, depending on the level of measurement.24
Our study suggested that the irregularity of BCRL is an inherent characteristic of this pathology. Differences in excess volume between the three segments was a constant which increased as a function of the severity of the lymphoedema. This irregularity could be explained by a global lymphatic system alteration, other than the simple stopcock theory, with local compensatory mechanisms18,25,26 beyond the changes that may occur directly in the lymphadenectomy area. In some cases, the oedema was concentrated in only one or two limb segments, leaving the rest of the limb free.
Indeed, some experimental segmental studies using bioimpedance and volumetry have highlighted the frequent occurrence of partial lymphoedema, or differences in the involvement between the measured segments, that may otherwise go unnoticed with global measurement methods.19–21,27 A segmental assessment study using bioimpedance and perometry in a group of 27 patients diagnosed with lymphoedema21 found that 7.4% had partial lymphoedema but a negative diagnosis by global excess volume. In other words, an excess volume of 10% was only exceeded in some segments, while more than 40% of patients with a global excess volume exceeding 10% presented some segments with less than 10% of excess volume.
In our study, 75 of all the 190 patients (39.47%) presented an anatomical area free of oedema during the follow-up period.
The concentration of oedema in the forearm, which in our study was related to the severity of lymphoedema, has also been reported in several other studies. Czerniec et al.21 found comparative percentages of bioimpedance remarkably similar to our volumetric observations, with figures for the forearm, especially in the proximal area, that were almost double those of the upper arm. Similarly, another segmental study in patients with breast cancer from the time of surgery up to one year later concluded that, in many cases, partial oedema preceded BCRL (using exclusively the global criteria to distinguish BCRL) and indicated that the forearm had the highest volume, especially in the proximal regions.20 The forearm was used to study the pathophysiology of BCRL because of the frequently observed concentration of oedema in this area.25 Studies using ultrasound also found that the ulnar area of the forearm was the most sensitive to oedema at the time of diagnosis.28
In contrast, the hand was the least affected segment. Approximately one third of patients in this current study did not experience local lymphoedema during their entire follow up; in those who did experience involvement, persistent oedema was mixed with initial oedema that disappeared or diminished over time, thereby reducing its partial ratio at the final measurement time point. Some experts exclude the hand from limb measurements (instead starting them from the level of the ulnar styloid) because the shape of the hand does not conform either to a cylinder or a truncated cone shape.4,5 Other authors consider assessment methods that include the hand in the perimeter measurements to be reliable,6,10,14 even finding a clear correlation of the perimeter volumes with the volumetry by water displacement in all the geometric figures analysed, including that of the cylinder.6 In our opinion, and from a clinical point of view, the hand must be evaluated. As with the rest of volumetry, more than an exact volume, we are interested in a precise comparison to study the extent of hand involvement that provides us a very valuable information to assessment of BCRL. Our results for the hand are consistent with other observations pointing to the frequent preservation of its lymphatic flow, which would explain its lesser involvement in BCRL.25,26 However, it should be noted that although the involvement of the hand was minimal at the time of peak BCRL, its volume did considerably increase in many severe cases. Thus, in accordance with previous observations,26 this implies that while the hand is unaffected in some patients, others experience significant oedema in this segment.
In general terms, the irregular distribution of oedema in BCRL may be because of different local compensation mechanisms whose efficiency may vary according to the segment in question. Hence, this distribution would tend towards a typical pattern consisting of a preferential concentration in the forearm, less involvement of the hand, and intermediate involvement of the upper arm. The analysis of peak involvement point to a clear relationship of this pattern with the severity of the oedema and the comparison between the initial and final measurement points suggests that this typical distribution becomes more consolidated throughout the clinical course, although in this case it was only significant for the hand.
Regarding the clinical concordance between the global and partial ratios, by using the same criteria for the partial assessment as for the global assessment, we classify patients as having lymphedema when at least one of the segments meets these criteria and we assess its severity based on of that segment. Thus, in the initial assessment, 47.95% of our patients who were considered non-lymphedema received a positive diagnosis with the partial criteria and 46.67% presented different severity classifications, always more severe according to the partial assessment.
The Kendall coefficient, below 0.5%, confirms a poor agreement between the global and partial measurements. Thus, if we accept the results of the partial measurement as reliable, indirect perimeter volumetry would considerably increase the positive predictive value and, especially, the negative predictive value. Hence, the volume excesses in BCRL concentrated in specific areas and overlapped with those in unaffected or less affected areas, giving rise to global ratios that were not indicative of the real clinical severity of these patients.22
One of the advantages of perimeter measurements compared to other volumetric methods is precisely that, it allows segmental assessments to be carried out.29 Although it is true that the simple observation of perimeter measurements can give us a good idea of the predominance of oedema, these must be translated into volumes for their quantification, so that evaluative conclusions can be reached. One of the two systematic reviews on lymphoedema measurement carried out to date indicated that bioimpedance in the early stages of lymphoedema, when there is usually partial or mild lymphoedema, is more sensitive compared to perimetry.8 Thus, applying partial measurements can help correct or reduce this difference. Our method is only one possibility. Preliminary calculations based on our data show frequent differences between the proximal and distal segments of the forearm and especially of the upper arm, so it could be interesting to extend the partial measurement to 5 segments.
Further studies in a healthy population will be necessary to establish both the global and partial cut-off points for the excess volume criteria.
ConclusionsThis study shows that the BCRL is characteristically irregular with a tendency to a typical pattern, with the forearm being the most affected segment, and the hand the least affected. The partial volumetry improves diagnostic sensitivity and clinical assessment in BCRL. Obtaining partial volumes in a spreadsheet is simple and, apart from the fact that there may be discussion about which segments should be measured and how to measure them, we consider partial volumetric measurement essential to be able to correctly assess BCRL.
FundingThis research has not received specific aid from public sector agencies, the commercial sector or non-profit entities.
Ethics considerationsThe study was approved by the Research Ethics Committee of the Consorcio Hospitalario Provincial de Castellón. It was conducted according to the ethical principles laid down in the Declaration of Helsinski (52nd WMA General Assembly, Edinburgh, Scotland, October 2000) and the rules of best clinical practice.
Informed consentThe ethics committee, based on article 58-2 of the Spanish biomedical research law (law 14/2007) and the Spanish General Data Protection Regulation of May 25, 2018 (RGPD), exempted our study from informed consent. The data was pseudonymized and included in a database, adhering to both current national legislation (Organic Law 3/2018 of December 5 and GDPR) and the European Parliament Regulation (EU 2016/679)
Conflict of interestThe authors declare have no conflict of interest.
Jorge Renau Tomás (Health Information Manager).
Angel Masoliver Forés (Doctor. Public Health Specialist).