Management of code stroke (CS) is complex, and the collection of information for subsequent evaluation is crucial. We present data obtained using a mobile application on the management of CS between 2020 and 2021 at the Hospital General Universitario Dr. Balmis (HGUB), a tertiary-level hospital that is the reference centre for endovascular treatment (EVT) in the province of Alicante.
Material and methodsWe conducted a prospective, observational study of all patients attended after CS activation at the HGUB in 1 year. Data were collected using a specifically designed mobile application (CODICT). We present a descriptive analysis of patients' baseline characteristics, call flow, acute phase care, treatment rates, and mortality and functional outcomes at discharge and at 3 months in patients receiving EVT.
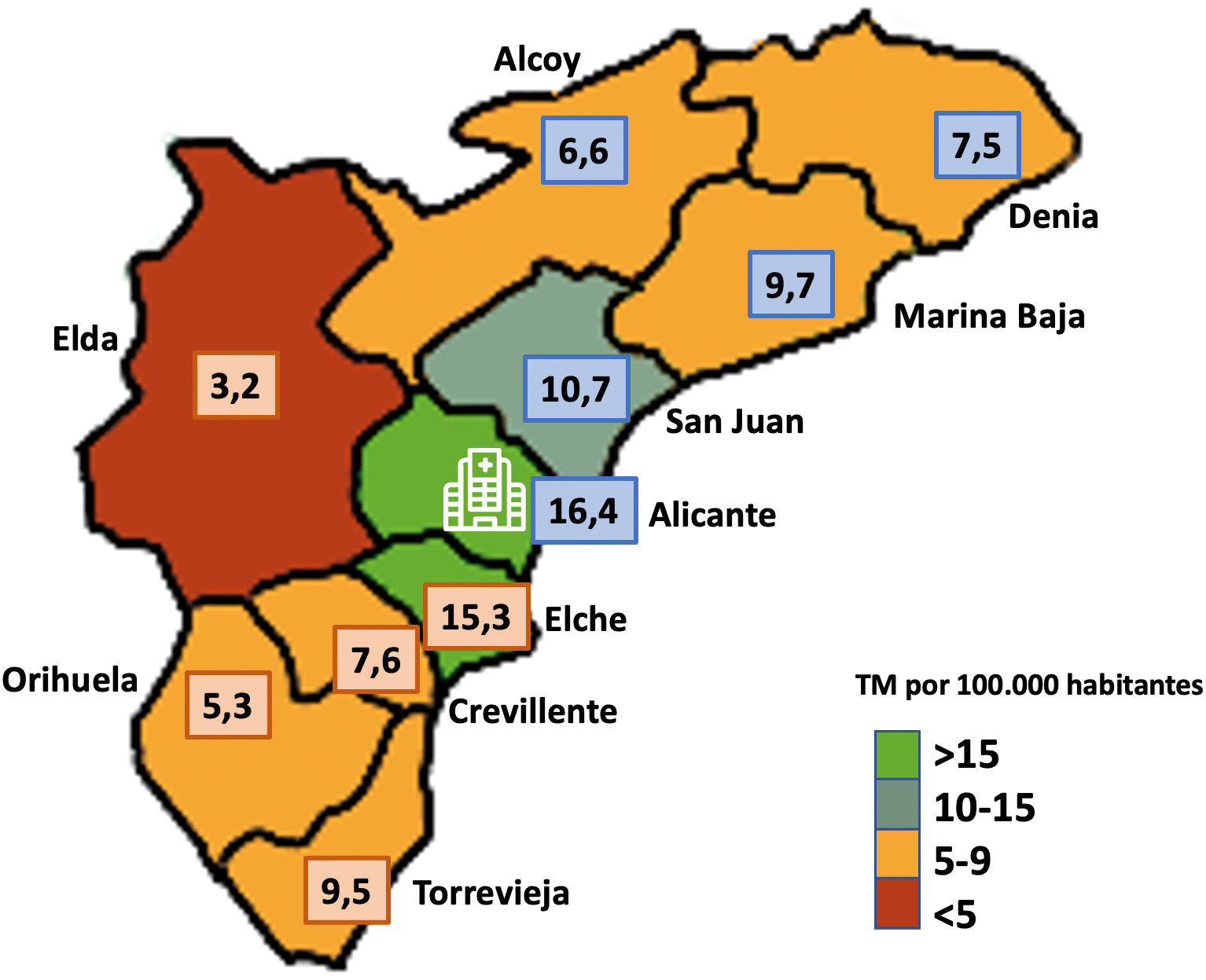
ResultsA total of 1018 CS activations were recorded. Revascularisation treatment (intravenous fibrinolytic treatment [IVT], EVT, or EVT+IVT) was performed in 252 patients (24.75%), of whom 177 (17.38%) received EVT, amounting to a mean rate of 9.43 per 100 000 population. By healthcare district, the lowest rate was 3.16 and the highest was 16.40. A total of 49.32% of patients receiving EVT presented favourable functional status (mRS≤2) at 90 days.
ConclusionThe data collected during IC care can be traced in real time through mobile applications. The potential of this approach is demonstrated by the volume of data collected during 1 year. These data show considerable disparities in access to EVT in the province of Alicante, which could be suggested as an area for improvement.
La atención al Código Ictus (CI) es compleja y resulta crucial recopilar información para su posterior evaluación. Exponemos los datos obtenidos mediante aplicación móvil, del manejo del CI durante 2020–2021 en el Hospital General Universitario Dr.Balmis (HGUB), hospital terciario referencia para tratamiento endovascular (TEV) de la provincia de Alicante.
Material y métodosEstudio observacional prospectivo de todos los sujetos atendidos por activación de CI en el HGUB en un año. Recogida de variables mediante aplicación móvil (CODICT) desarrollada para tal fin. Análisis descriptivo de las características basales de los pacientes, flujo de llamadas, atención en fase aguda, tasas de tratamiento y resultados funcionales y de mortalidad al alta y a los tres meses en los casos sometidos a TEV.
ResultadosSe recibieron 1018 activaciones de CI. 252 pacientes (24,75%) recibieron tratamiento revascularizador (Fibrinólisis intravenosa (FIV), TEV o TEV + FIV), de ellos, 177 (17,38%) recibieron TEV lo que supuso una tasa media de 9,43 por 100.000 habitantes. Por departamentos de salud la tasa más baja fue de 3,16 y la máxima de 16,40. Un 49,32% de los pacientes sometidos a TEV alcanzaron situación funcional favourable (mRS ≤ 2) a los 90 días.
ConclusiónLa trazabilidad de los datos recopilados durante la atención al CI es susceptible de realizarse a tiempo real mediante aplicaciones móviles. Su potencial queda patente en el volumen de datos recogidos durante un año. Se ha manifestado una fuerte disparidad en el acceso a TEV en la provincia de Alicante, susceptible de proponerse como área de mejora.
Stroke is the leading cause of disability worldwide1 and the second leading cause of death in Spain, and the first in women,2 and represents an important social and health problem.
A rapid response in the treatment of acute stroke is critical in reducing morbidity and mortality.3 Code stroke (CS) was created with the aim of identifying candidates for early revascularisation treatment and reducing management times, and has shown great benefits in the prognosis of these patients.4
In recent years, we have witnessed great advances that have led to increased survival and better functional prognosis in patients with acute ischaemic stroke (AIS). The implementation of stoke units (SUs) and intravenous fibrinolytic treatment (IFT) represent a milestone reached in the late 20th century. The development and improvement of new revascularisation treatments in recent years, in the form of different endovascular treatment (EVT) techniques, represent a promising achievement in the therapeutic management of this disease.5–9 EVT is fundamental in the treatment of AIS due to large-vessel occlusion, which is usually associated with higher rates of morbidity and mortality. However, all these therapies have been a huge organisational and logistic challenge in the different stroke care networks and for the professionals responsible for managing these patients.
In the specific case of the stroke care network in Alicante, the 2011–2015 stroke care plan of the Valencian Community,10 in its annex on EVT of AIS, established Hospital General Universitario Dr. Balmis (HGUB) as the reference centre for EVT for patients from the 10 health districts (HD) of Alicante.
Since 2015, when EVT was implemented at HGUB for the management of patients with AIS, the number of CS activations and patients undergoing EVT has progressively increased. This has had a significant impact on stroke care networks and hospitals with SU.
Given the high level of organisational complexity, it is crucial to gather information for subsequent assessment and identification of areas for improvement. Many professionals are involved, both at the hospital and elsewhere, which necessarily entails information inefficiency problems (duplication of information, delayed dissemination, and mistakes). Therefore, an easy-to-use data collection software application was developed for installation on the mobile phones of members of the neurology department who attend CS patients, to facilitate prospective data recording.
MethodsWe conducted a prospective observational study, recording data from all patients attended after CS activation at the HGUB during the period 01 July 2020 to 30 June 2021.
CODICT softwareThe first part of this project consisted in developing the software for the prospective registry; development followed guidelines on information security, intuitive interface, usability in iOS and Android mobile phones, and multi-user data entry. Once developed, and with the approval of the clinical research ethics committee of Institute of Health and Biomedical Research of Alicante, the software was installed on the mobile devices of the neurologists participating in the study. It allows for data entry for different variables, especially time-related variables, and includes categories for the remaining variables; a randomly generated alphanumeric code is assigned to each entry, and the application does not allow for the recording of any sensitive data that may lead to identification of the patients.
Data collectionData were prospectively collected on mobile phones using the CODICT software, in real time in many cases, by the neurologist responsible for CS at that time. Recording began at the time of activation, with subsequent addition of all other variables from the patients' admission to and stay at the SU. Finally, the outpatient vascular neurology clinic recorded the functional status at 3 months of patients treated with EVT. Data were subsequently uploaded to an Excel spreadsheet for analysis.
Stroke care network in Alicante and study populationThe study was performed at HGUB, the reference hospital in Alicante for EVT in CS and one of the province's 2 SU, together with Hospital General Universitario de Elche (HGUE). Hospital care in CS is provided by HGUB in the HDs of the north of the province and by HGUE in the southern HDs. As there was a previous assessment by the neurology department of the HGUE, CS activations received by the HGUB from the southern HDs corresponded to activations for EVT assessment. All candidates for EVT were referred to the HGUB (Fig. 1).
Data processing and statistical analysisStatistical analysis was performed using the R statistics software (version 4.0.5), with the RStudio interface (version 1.3.959).11
Qualitative variables are expressed as frequencies and percentages. Normally distributed quantitative variables (Shapiro–Wilk test and/or Kolmogorov–Smirnov test) are expressed as means and standard deviation (SD). Non-normally distributed quantitative variables are expressed as median and interquartile range (IQR).
For estimating the different population rates, we used data from the Population Information System for the different HDs of Alicante, as of 31 December 2020 and obtained from official registries; results are expressed as rates per 100 000 person-years. We performed an inferential analysis, and results are expressed together with their 95% confidence intervals (95% CIs).
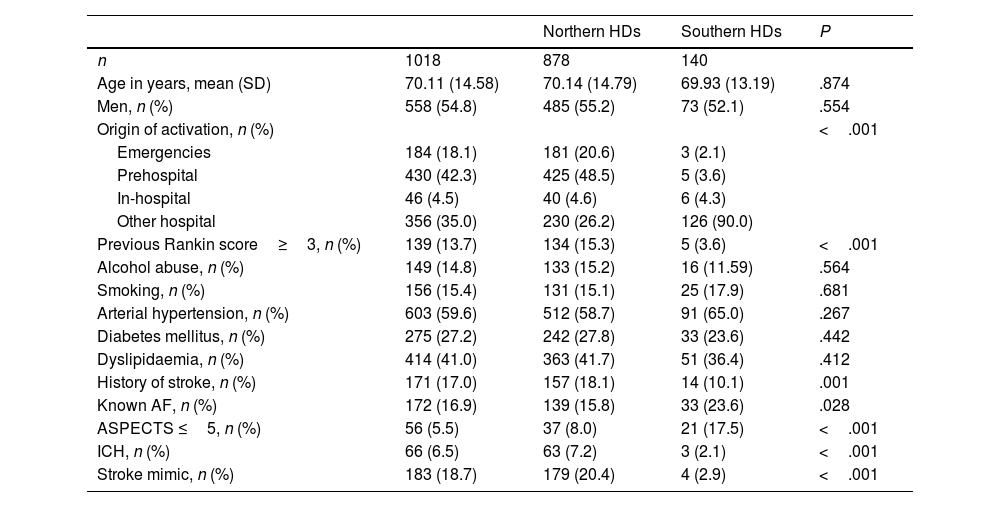
ResultsClinical and sociodemographic characteristics of code stroke activationsDuring the study period, 1018 telephone calls for CS activation were recorded. Patients' sociodemographic characteristics are listed in Table 1. Mean age was 70.11 (14.58) years. We observed a slight preference for CS activation in men (54.8%), who showed a significantly younger age than women (69.03 vs 71.41 years). Regarding the origin of activations, a high percentage of prehospital activations (42.3%) were made by the emergency services.
Clinical and sociodemographic characteristics of code stroke activations.
| Northern HDs | Southern HDs | P | ||
|---|---|---|---|---|
| n | 1018 | 878 | 140 | |
| Age in years, mean (SD) | 70.11 (14.58) | 70.14 (14.79) | 69.93 (13.19) | .874 |
| Men, n (%) | 558 (54.8) | 485 (55.2) | 73 (52.1) | .554 |
| Origin of activation, n (%) | <.001 | |||
| Emergencies | 184 (18.1) | 181 (20.6) | 3 (2.1) | |
| Prehospital | 430 (42.3) | 425 (48.5) | 5 (3.6) | |
| In-hospital | 46 (4.5) | 40 (4.6) | 6 (4.3) | |
| Other hospital | 356 (35.0) | 230 (26.2) | 126 (90.0) | |
| Previous Rankin score≥3, n (%) | 139 (13.7) | 134 (15.3) | 5 (3.6) | <.001 |
| Alcohol abuse, n (%) | 149 (14.8) | 133 (15.2) | 16 (11.59) | .564 |
| Smoking, n (%) | 156 (15.4) | 131 (15.1) | 25 (17.9) | .681 |
| Arterial hypertension, n (%) | 603 (59.6) | 512 (58.7) | 91 (65.0) | .267 |
| Diabetes mellitus, n (%) | 275 (27.2) | 242 (27.8) | 33 (23.6) | .442 |
| Dyslipidaemia, n (%) | 414 (41.0) | 363 (41.7) | 51 (36.4) | .412 |
| History of stroke, n (%) | 171 (17.0) | 157 (18.1) | 14 (10.1) | .001 |
| Known AF, n (%) | 172 (16.9) | 139 (15.8) | 33 (23.6) | .028 |
| ASPECTS ≤5, n (%) | 56 (5.5) | 37 (8.0) | 21 (17.5) | <.001 |
| ICH, n (%) | 66 (6.5) | 63 (7.2) | 3 (2.1) | <.001 |
| Stroke mimic, n (%) | 183 (18.7) | 179 (20.4) | 4 (2.9) | <.001 |
AF: atrial fibrillation; ASPECTS: Alberta Stroke Program Early CT Score; HD: health district; ICH: intracranial haemorrhage; SD: standard deviation.
Table 2 presents the distribution of CS activations by each HD. Data are expressed as absolute frequency and percentage, as well the estimated incidence based on the population of each district.
Code stroke activation by health district and incidence.
| HD | n (% of the total) | Population | CS per 100 000 person-years, mean (95% CI) |
|---|---|---|---|
| Alcoy | 58 (5.7) | 137 336 | 42.23 (32.36–55.00) |
| Alicante | 359 (35.3) | 280 535 | 127.97 (115.24–142.09) |
| Denia | 182 (17.9) | 174 194 | 104.48 (90.10–121.10) |
| San Juan | 168 (16.5) | 225 153 | 89.51 (76.72–104.38) |
| Marina Baja | 109 (10.7) | 184 956 | 58.93 (48.62–71.37) |
| Total northern HDs | 876 (86.1) | 1 002 174 | 87.61 (81.95–93.64) |
| Elche | 51 (5.0) | 169 599 | 30.07 (22.62–39.87) |
| Elda | 16 (1.6) | 189 629 | 8.44 (4.99–14.03) |
| Orihuela | 18 (1.8) | 169 580 | 10.61 (6.49–17.14) |
| Torrevieja | 38 (3.7) | 188 602 | 20.15 (14.46–27.96) |
| Crevillente | 17 (1.7) | 157 314 | 10.81 (6.50–17.70) |
| Total southern HDs | 142 (13.9) | 874 724 | 16.00 (13.51–18.95) |
| Not assigned | 2 (0.2) | – | 1.07 (0.18–4.30) |
| TOTAL | 1018 (100) | 1 876 898 | 54.24 (50.98–57.70) |
CI: confidence interval; CS: code stroke; HD: health district.
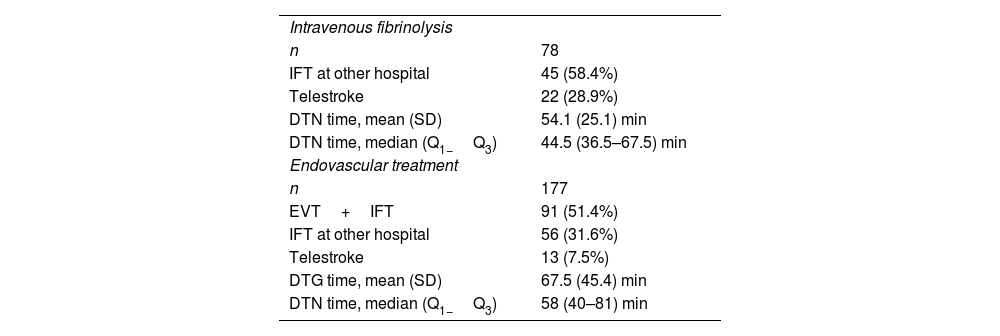
A total of 255 patients (25.04%) underwent some type of revascularisation treatment. Of the 169 patients receiving IFT, 102 were treated at a hospital other than HGUB. Of the 177 patients receiving EVT, 91 received IFT, and 86 primary EVT. Table 3 shows the total number of patients receiving each type of revascularisation treatment and the corresponding door-to-needle (DTN) times. Calculation of door-to-needle (DTN) times only included those cases treated at the HGUB, as data from other hospitals were not available.
Revascularisation treatment.
| Intravenous fibrinolysis | |
| n | 78 |
| IFT at other hospital | 45 (58.4%) |
| Telestroke | 22 (28.9%) |
| DTN time, mean (SD) | 54.1 (25.1) min |
| DTN time, median (Q1−Q3) | 44.5 (36.5–67.5) min |
| Endovascular treatment | |
| n | 177 |
| EVT+IFT | 91 (51.4%) |
| IFT at other hospital | 56 (31.6%) |
| Telestroke | 13 (7.5%) |
| DTG time, mean (SD) | 67.5 (45.4) min |
| DTN time, median (Q1−Q3) | 58 (40–81) min |
DTG: door-to-groin puncture; DTN: door-to-needle; EVT: endovascular treatment; IFT: intravenous fibrinolytic treatment; Q1–Q3: quartiles 1 and 3; SD: standard deviation.
Fig. 2 shows the rates per 100 000 person-years of patients undergoing EVT distributed by HD of origin, using a colour-coded map.
Rate of endovascular treatment per 100 000 person-years by health district of origin. The hospital symbol indicates the approximate location of the HGUB. The numbers in blue squares correspond to northern HDs and in orange squares to southern HDs. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
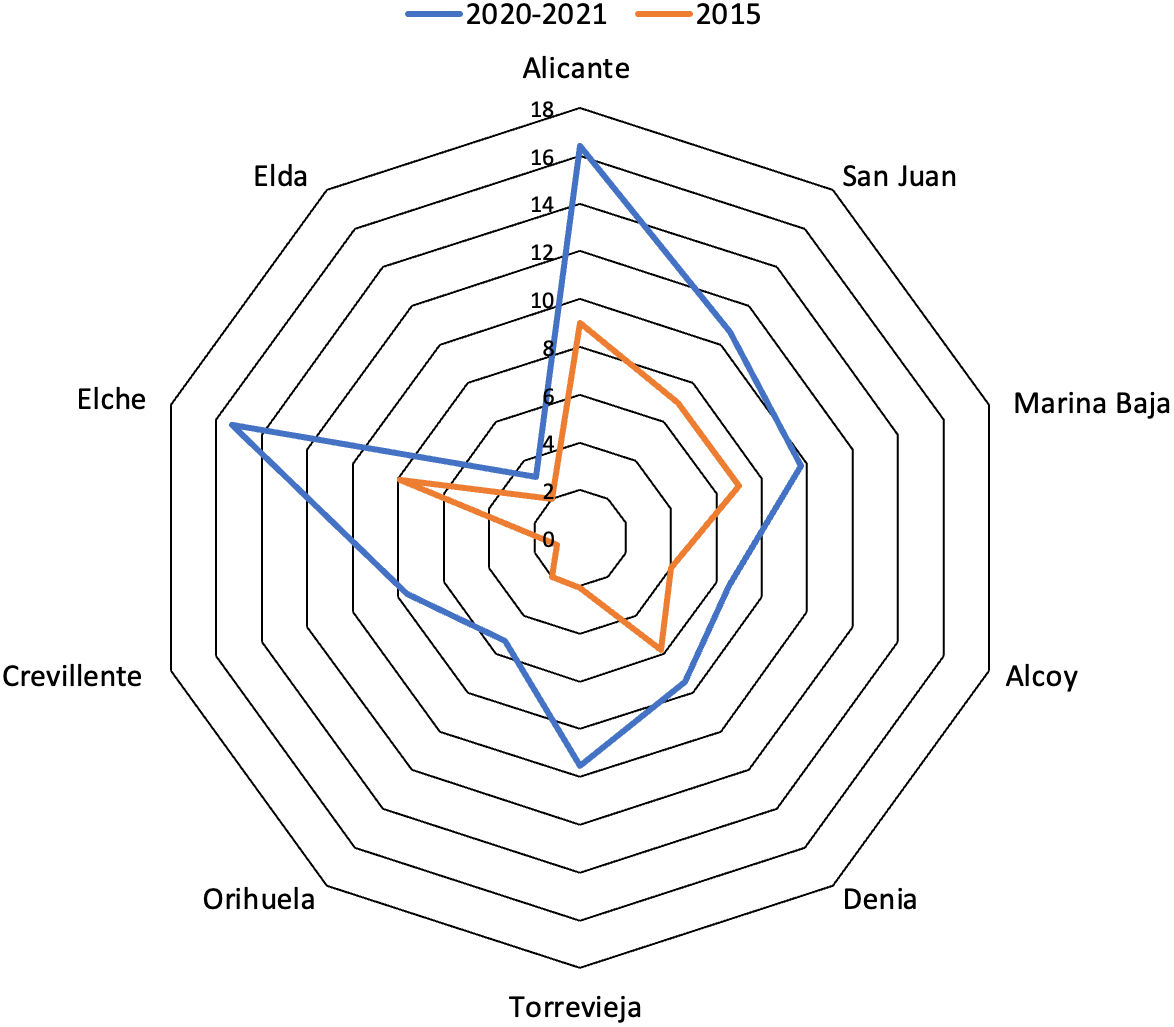
We compared the progression of these rates against rates from 2015, as shown in Fig. 3.
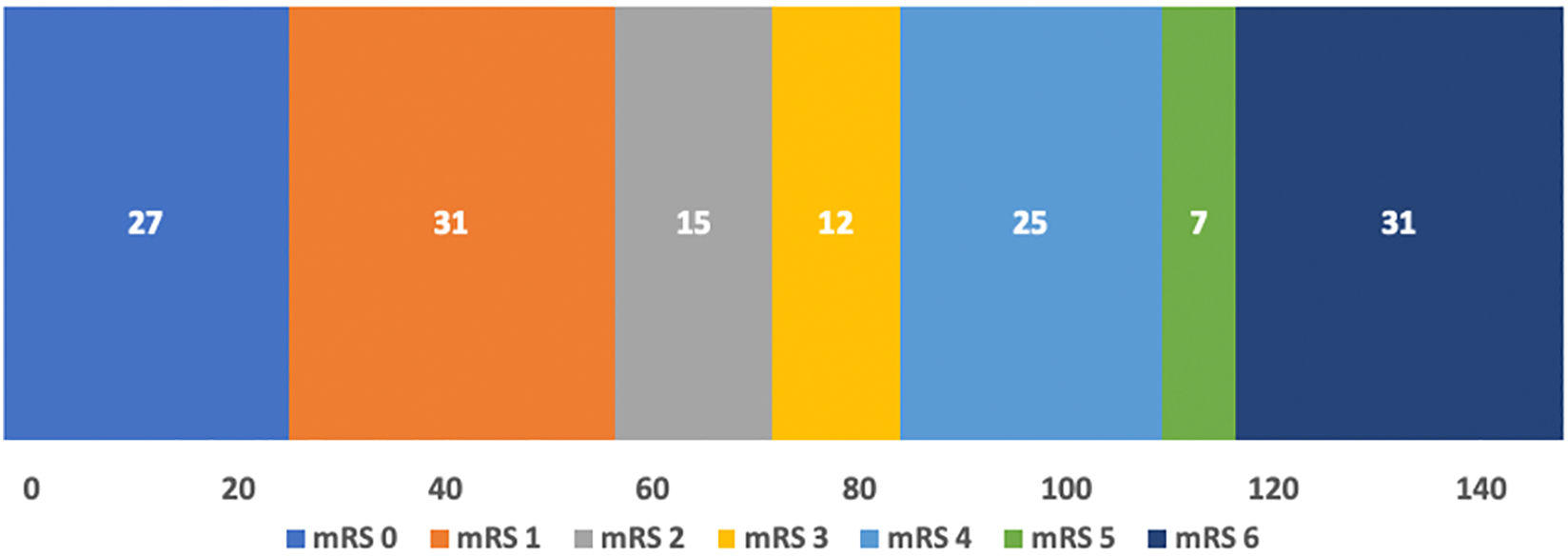
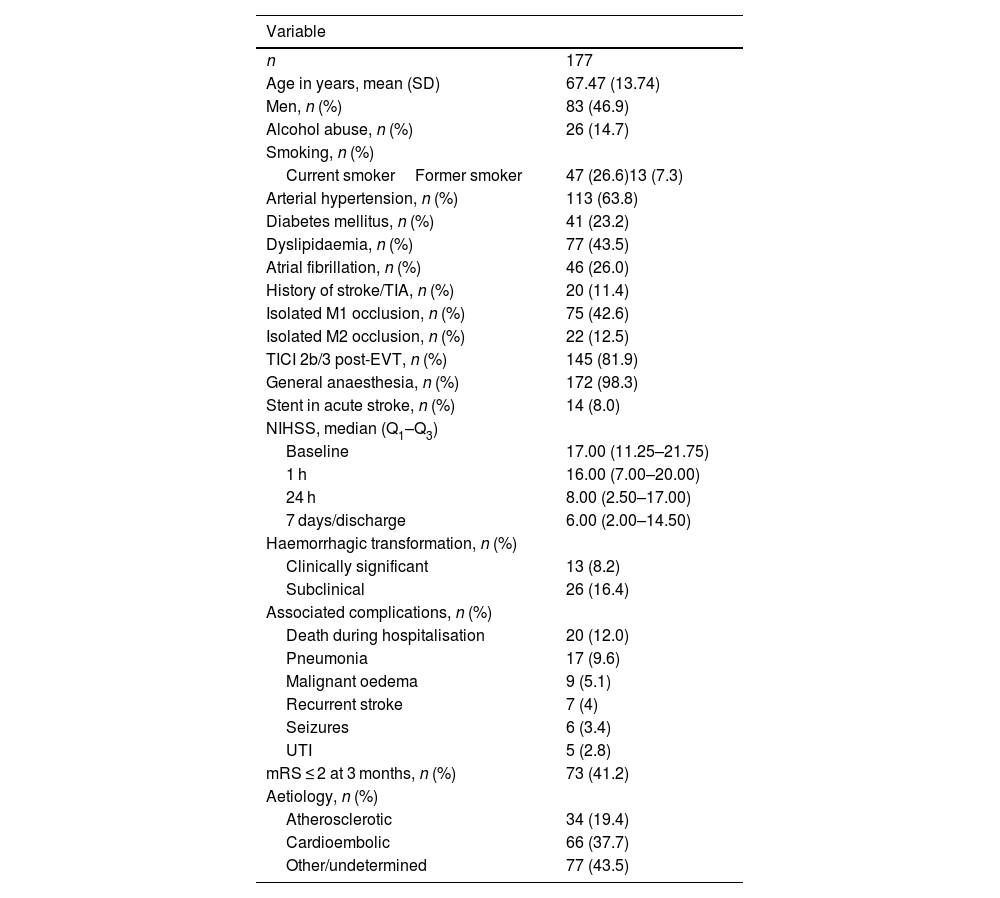
Table 4 presents the characteristics of patients undergoing EVT, as well as several related technical aspects and data on the clinical progression of the patients. Fig. 4 shows the distribution of patients' functional status at 3 months after EVT. In the modified Rankin Scale (mRS) assessment at 3 months, 29 patients (16.3%) were lost to follow-up; most of these were foreign patients who returned to their home countries.
Clinical characteristics of patients undergoing endovascular treatment and clinical outcomes.
| Variable | |
|---|---|
| n | 177 |
| Age in years, mean (SD) | 67.47 (13.74) |
| Men, n (%) | 83 (46.9) |
| Alcohol abuse, n (%) | 26 (14.7) |
| Smoking, n (%) | |
| Current smokerFormer smoker | 47 (26.6)13 (7.3) |
| Arterial hypertension, n (%) | 113 (63.8) |
| Diabetes mellitus, n (%) | 41 (23.2) |
| Dyslipidaemia, n (%) | 77 (43.5) |
| Atrial fibrillation, n (%) | 46 (26.0) |
| History of stroke/TIA, n (%) | 20 (11.4) |
| Isolated M1 occlusion, n (%) | 75 (42.6) |
| Isolated M2 occlusion, n (%) | 22 (12.5) |
| TICI 2b/3 post-EVT, n (%) | 145 (81.9) |
| General anaesthesia, n (%) | 172 (98.3) |
| Stent in acute stroke, n (%) | 14 (8.0) |
| NIHSS, median (Q1–Q3) | |
| Baseline | 17.00 (11.25–21.75) |
| 1 h | 16.00 (7.00–20.00) |
| 24 h | 8.00 (2.50–17.00) |
| 7 days/discharge | 6.00 (2.00–14.50) |
| Haemorrhagic transformation, n (%) | |
| Clinically significant | 13 (8.2) |
| Subclinical | 26 (16.4) |
| Associated complications, n (%) | |
| Death during hospitalisation | 20 (12.0) |
| Pneumonia | 17 (9.6) |
| Malignant oedema | 9 (5.1) |
| Recurrent stroke | 7 (4) |
| Seizures | 6 (3.4) |
| UTI | 5 (2.8) |
| mRS ≤ 2 at 3 months, n (%) | 73 (41.2) |
| Aetiology, n (%) | |
| Atherosclerotic | 34 (19.4) |
| Cardioembolic | 66 (37.7) |
| Other/undetermined | 77 (43.5) |
2B/3: time to TICI 2b/3; EVT: endovascular treatment; mRS: modified Rankin Scale; NIHSS: National Institutes of Health Stroke Scale; Q1–Q3: quartiles 1 and 3; SD: standard deviation; TIA: transient ischaemic attack; TICI: Thrombolysis in Cerebral Infarction Scale; UTI: urinary tract infection.
There is growing interest in the use of new technologies and data science in multiple areas of medicine, including neurology and stroke care networks. In this respect, CODICT is a pioneering application in this field. A review of articles on stroke-related mobile applications revealed no other application with similar characteristics.12 We did not find any prospective registry based on data collected through mobile applications. Although mobile applications have been developed, such as the JOIN app, which uses real-time data to optimise the management of CS by improving communication between team members, its functionality does not focus on data collection.13,14
Our study shows the multiple opportunities for data collection using non-traditional platforms. After the implementation of the application and subsequent data analysis, several key aspects of CS management in the province of Alicante have been identified.
The most relevant aspect of the data shown in this study is the unequal access to recanalisation therapies in Alicante. The rate of EVT in Alicante amounted to a mean of 9.43 patients per 100 000 person-years, ranging from 3.16 in the HD of Elda to 16.44 and 15.33 in the HDs of Alicante and Elche, respectively. Both districts have an SU and a 24-h on-call neurology service available throughout the year. Some possible reasons for this difference may be the characteristics of the population, geographical factors, patient referral networks, decreased awareness and knowledge of patients and professionals, and the presence of on-call neurologists.
Only 25% of patients finally received revascularisation treatment of any kind. One of the main reasons for ruling out revascularisation treatment was unfavourable functional status, present in 13.7% of the cases; better optimisation of the neurology department's workload may be achieved if improvements were made in the determination of the patient's previous functional status by the professionals activating CS.
It is also interesting to observe the increase in rates of EVT over a period of 5 years, an increase that (we may hypothesise) is explained not only by population growth, but also by an improvement in the CS management process, increased awareness among the population and healthcare professionals, greater cumulative experience, and an increased number of indications. It is therefore to be expected that the number of EVT will continue to increase.
Of the patients receiving EVT, 49.32% maintained a good functional prognosis (mRS≤2) at 3 months of treatment; this figure is very similar to the typical success rate of this treatment.15 This figure may be underestimated, as the main source of censored data in our registry (29 patients) corresponded to foreign patients who were lost to follow-up after returning to their home countries. In these cases, we assumed an acceptable functional status. A meta-analysis of the results of the MR CLEAN, EXTEND-IA, ESCAPE, SWIFT PRIME, and REVASCAT clinical trials revealed a futile recanalisation rate of 54%,16 which is slightly higher than the rate reported in our study. This underscores the relevance of EVT-based recanalisation techniques for the functional prognosis of patients. Early treatment of AIS is absolutely fundamental.
One potential benefit of time recording applications is precisely the improvement in those times due to the well-known Hawthorne effect, as shown in the study by Noone et al,17 which reported that the use of a time recording application led to a significant improvement in the key management times in CS. Some of these applications, such as the ESN-app, have even shown a benefit in functional outcomes.18
In our study, we observed a mean DTN time of 47.90 (7.90) min, and a door-to-groin (DTG) puncture time of 67.56 (43.39) min. Since the implementation of the application, we have observed a progressive improvement in these times, with a DTN time of 40.8 and DTG time of 81.9 in the first 3 months of the study, and a DTN time of 31.3 and DTG time of 55.6 in the last trimester of the study. However, these improvements may not be exclusively due to the use of the CODICT application, as progressive improvements made to the hospital protocol for CS management may also have contributed.
The main limitation of our registry is the selection bias inherent to data collection from a single hospital. Data were lost in cases of patients referred to their reference hospital, with healthcare being provided there and no further contact being made. Furthermore, the lack of time monitoring at other hospitals prevents the analysis of such new metrics as door-in door-out (DIDO) times, which are fundamental to study processes at centres without EVT.19 Furthermore, in southern HDs, activations were first assessed at the HGUE; as a result, many of these were not recorded in the registry. Activations from southern HDs to the HGUB were made via a telephone call from the HGUE on-call neurologist to the HGUB on-call neurologist to suggest EVT. As all patients in the province who may be eligible for EVT are referred to the HGUB, no data were lost in these cases. Although we lack official data from the different HDs on the total number of diagnoses of ischaemic stroke and their aetiologies, we do have data on the registered population as of the date of the study, and therefore the rate of EVT per 100 000 person-years may be an appropriate measurement for estimating access to EVT.
ConclusionThe registry of data collected through the CODICT mobile application enables the optimisation of certain aspects of clinical management by monitoring the process and identifying potential areas for improvement in real time, gathering a large volume of data in a short period of time. Those data have revealed an inequality in access to EVT in the different HDs of the province of Alicante. Given the implications of EVT for the vital and functional prognosis of these patients, there is a need for social and healthcare efforts to achieve equitable access to these resources.
FundingThe development of the CODICT application was partly funded by the Institute of Health and Biomedical Research of Alicante (ISABIAL).
Informed consent and data confidentialityThe authors observed their centre's protocols for accessing medical records for the purpose of drafting this type of study for research and dissemination among the scientific community. No informed consent was necessary for this study.
Ethical considerationsThe authors observed their centre's protocols for accessing medical records for the purpose of drafting this type of study for research and dissemination among the scientific community. The study was approved by the drug research ethics committee of the health district of Alicante - Hospital General, on 27 May 2020 (report 2020-06).