The elderly constitute a growing world population group, with more than 200 million people over 60 years of age. This fact has increased the detection of chronic-degenerative diseases, as well as the prescription and consumption of medicines. The elderly are particularly susceptible to adverse drug events or interactions with other drugs due to their physiological changes, genetic predisposition and environmental exposure. It becomes necessary to adapt the health systems with integral and multidisciplinary approaches suitable to this demographic change, as the knowledge about appropriate prescription, clinical pharmacology and medication use in the elderly has become essential.
It has been shown that about two thirds of elderly patients receive inappropriate drug doses, and a substantial percentage of their hospital admissions are associated with potentially preventable toxic effects of drugs. To date, expert criteria, error detection tools and educational prescription plans have been developed by expert consensus for the safe use of drugs in the geriatric population. The objective of this study is a brief review of the principal physiological changes in an older adult, and summarize the contributions of the consensuses on prescription.
Introduction
According to the World Health Organization (WHO), any individual who is more than 60 years old is considered elderly or an older person. This definition applies for most industrialized countries and the UN.1 The number of elderly is increasing worldwide with over 200 million older people, and an increase of 30% is expected in the next few years.1
In Mexico, in 2010 the National Institute of Statistics and Geography (INEGI by its Spanish acronym) recorded over 11 million elderly in its census,2 and according to the projections by the National Population Council, by the year 2050 older people will represent 28% of the Mexican population, with approximately 36 million people.3 Nowadays, the elderly population is growing twice as fast as the country’s population growth rate.
The increase in life expectancy has an impact in terms of health, which is reflected in a substantial increase in chronic degenerative diseases, thus making the technological and economic development that this epidemiologic transition requires necessary, with a demand for multidisciplinary medical strategies. Prescription and consumption of medications has increased among the geriatric population, hence the presence of adverse pharmacological events. The objective of this document is to make a brief review of the main physiological changes of the elderly, as well as summarizing the contribution of consensuses about prescriptions in this population.
Pharmacology in the elderly
The elderly population presents physiological and pharmacologic changes which make it especially susceptible to presenting secondary or adverse events to medications, even with commonly used pharmaceutics.4,5 The need to know about prescriptions, clinic pharmacology and use of medication in the geriatric population becomes evident, in addition to preparing social, economic and health systems for current and future population demographic changes.6-8 It is estimated that people over 65 consume 25-50% of all prescribed pharmaceutics, and are responsible for 70% of the total pharmaceutical expenditure.9 Different studies have calculated that two thirds of geriatric patients receive an inappropriate dosage of medication, especially those with renal elimination.10-12 Moreover, the harmful effects of the pharmaceutics may have safety consequences and economically affect the health system.13
Approximately 30% of hospital admissions of older patients is linked to the toxic effects of pharmaceutics. The related adverse effects of pharmaceutics have been associated with preventable problems, like depression, constipation, falls, immobility, confusion and hip injuries.13
In a study conducted in patients who live in retirement homes, it was proved that approximately two thirds of residents had an ADR in a period of four years and out of them 1 in 7 required hospitalization.14 In the US in 2012 problems related to medications caused 106 000 deaths with a cost of 85 billion dollars. Other authors have calculated the ADR-related expenditure to be $76.6 billion in outpatient care, $20 billion in hospitals and $4 billion in nursing homes.13,15
Physical changes in the elderly
Physiologically, the elderly is in a state characterized by a reduction in functional reserves and their ability to adapt,6,16-18 which suggests a different response to that of a young patient when dealing with a disease or the administration of certain medication. Proper knowledge of the changes in pharmacokinetics and pharmacodynamics in the elderly is necessary for a correct prescription, which minimizes or avoids adverse effects of medications.6,18-20
Variability in response to pharmacological intervention is conditioned by genetic factors, age, diseases, interactions and prescription compliance, which results in alterations in the pharmacokinetics and pharmacodynamics profiles, in addition to the frequent atypical presentations of diseases and the administration of multiple medications.21,22
Pharmacokinetics
Pharmacokinetics determine the relationship between a medication administration and the concentration which it reaches in the body with time (in relationship with the dosage, presentation, frequency and form of administration), and despite the fact that many changes of these parameters have been described, inter-individual variability is the rule.6,18,19
Bioavailability refers to the proportion of the medication that reaches circulation, and it is a function of the form of administration, the chemical properties of the medication and the absorption and amount of dosage which is eliminated through the hepatic metabolism of the first step before reaching circulation.6,17 Bioavailability is affected by age, because absorption becomes slower, increasing the necessary time to reach maximum concentration in plasma. Some medications require an acid environment for its absorption, like ketoconazole, ampicillin or iron, and may have a decline of their bioavailability from 5 to 10%, as a result of hypochlorhydria secondary to atrophic gastritis or treatment with H2 antagonists and proton-bomb inhibitors.17-19 In the elderly, the hepatic metabolism of the first step is diminished, and oral medication bioavailability which goes through this process is greater.17,18
Distribution volume depends on the plasma’s union to protein, on water and lipid proportion and on tissue perfusion. The latter may decrease with age, causing a slower distribution, and a reduction of the dosage load with most medications should be considered.17,18 Concerning water and lipids proportion, body fat in the elderly is considered to increase between 20 and 40% and corporal water decreases by 10 to 15%, leading to an increase in concentration of water-soluble medications and a slower elimination of fat-soluble medications.18-21
Some medications which present a lower distribution volume in the elderly are digoxin, cimetidine, gentamicin, phenytoin and theophylline, among others, and this translates to high plasmatic levels of the medications.18
The most important elimination mechanisms are hepatic and renal. Hepatic metabolism in older people has a substantial decrease in its activity and there are also changes in the gastrointestinal system, like a decrease in gastric acid secretion and intestinal motility.6,19 This decrease in elimination rate prolongs medications’ half-lives and carries with it the need to increase administration intervals.6,18 This occurs with medications like acetaminophen, amitriptyline, barbiturates, ibuprofen, lidocaine, prazosin, propranolol, salicilates and warfarin, among others.18
Pharmacodynamics
Pharmacodynamics describes the effects of medications in tissue (what medications cause in the body).6-18 Although it can be altered by age, these changes have not been thoroughly studied. Almost every action of the medications are mediated by a interaction of medication molecules with tissue receptors, and these can be altered by hormones, neurotransmitters and transportation systems, among others, and the central nervous and cardiovascular systems play a very important role.6
Pharmacogenetics
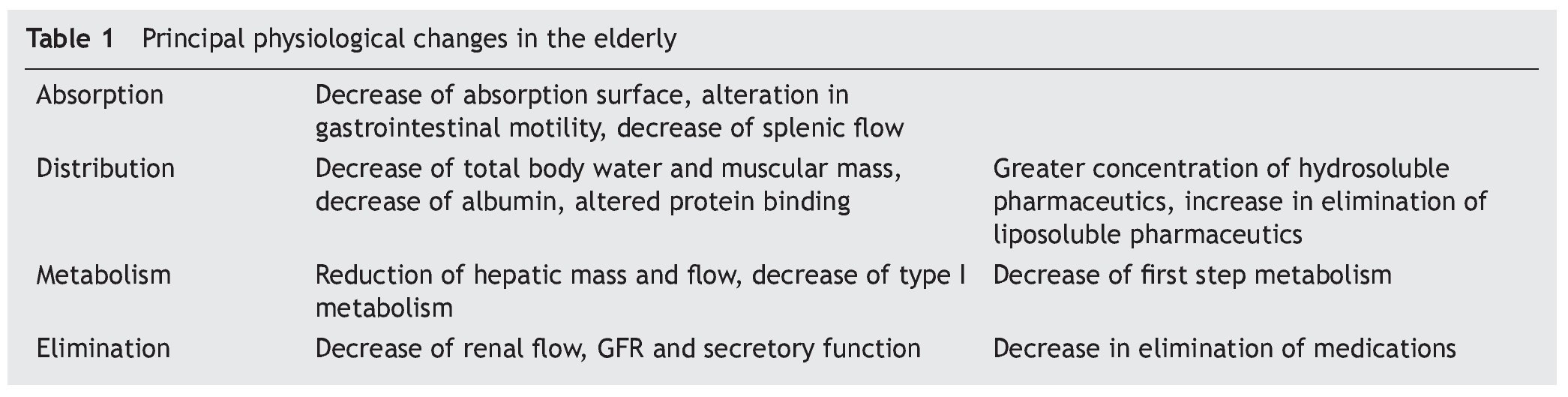
Genetic variation is one of the causes of versatility in responses to medications and is estimated to contribute between 20 and up to 95%, even though the genetic expression can also be related to age and environmental factors.6 The aging process itself and the presentation of diseases have polygenic causes, thus the response to many medications can also be altered by polymorphisms in genes that may not be responsible for the pharmacokinetic or are not its direct target.6 In table 1 there is a summary of the main physiological changes linked to age.
Adverse effects of the use of medications in geriatrics
Prescription errors in the elderly population are generally related to pharmacological changes, inadequate orientation about dosage modification, and lack of recommendations or guides about safety of some medications in the geriatric population.21,22
Sometimes, randomized and controlled studies do not include patients over 65 years, consequently the results on the safety of some medications cannot be generalized to this population. Adverse effects of medications include adverse reactions and prescription errors. An adverse medication reaction (AMR) is defined as any undesired sign or symptom which appears after medication administration at therapeutic doses. A severe or extremely severe AMR is one which requires hospitalization or causes irreversible damage including death.1,6,18 Adverse reactions are classified based on their relation with a medication in five groups (A-E). Type A is linked to the medication’s pharmacologic action, predictable or dosage-associated (pharmacokinetic changes, medication-medication, medication-food or medication-disease interactions), and represent most of the adverse effects. In group B there is no relation with pharmacologic actions and are independent of dosage, these are less frequent but more severe (allergic reactions, cytotoxic, idiosyncratic, etc.), and are unpredictable.22,23 The reactions of group C are related to prolonged and continuous use of a medication, such as dependency reactions or tachyphylaxis. Group D refers to late or long-term reactions like teratogenicity, and carcinogesis and group E is produced when a medication is suspended (“rebound effect”).
However, there are many classification systems. Mallet et al suggest a simple approach to the problem, and summarizes it in three categories, which are adverse reactions by pharmacologic interactions; patients who consume multiple medications and/or have multiple diseases (nine or more medications and five or more comorbidities); and the “prescription cascade” phenomenon, where the adverse effect of a medication leads to the prescription of another agent which at the same time causes a new secondary effect which would add a new medication.23-25 Most adverse reactions to medications in hospitalized elderly are type A and therefore represent predictable reactions and are potentially preventable.26,27
The medications that relate the most to adverse reactions and events are medications used to treat cardiovascular diseases, followed by rheumatologic and endocrinological medications, and this corresponds with the frequency and morbidity of these diseases in Mexico.27
Polypharmacy
The use of concomitant medications is justified in the treatment of multiple chronic diseases. Polypharmacy is a term which describes patients who receive multiple medications, and in the elderly, this represents the rule rather than the exception.16,17
According to data from population studies in the United States, 90% of the elderly consume at least a weekly medication, over 55% of women and 44% of men of advanced age consume five medications or more, and 40% of residents in nursing homes consume over eight weekly medications.4,5,16
With this practice the risk of AMR increases drastically, because on many occasions, there are duplicates of the same kind of medication, and the adverse effects are not identified, leading to a prescription cascade.23-25,28
Adverse reactions may be difficult to detect in elderly patients because they frequently have atypical presentations, like lethargy, confusion, falls, constipation and depression.
Nursing homes residents are the most vulnerable of this group.28
An appropriate use of medications in geriatrics?
With the purpose of minimizing the problems that emerge as a consequence of inappropriate prescription of medications in the elderly, consensus criteria have been developed in order to improve safety among this population.
Beers criteria
Beers et al,28 in 1999, supported by a group of experts in geriatrics, geriatric pharmacology, psychopharmacology and pharmacoepidemiology, in addition to the revision of scientific literature, developed a consensus of medications used in the elderly and their frequent adverse effects. Criterion were developed which have been widely used to describe treatment patterns and educate and inform clinical doctors. A revision of these criteria was made in 199729 and later in 200330 to reevaluate new products, to reassess the severity assigned to each medication and to identify new situations or major considerations. The application of these criteria have allowed an improvement of pharmacological therapy safety, since it identifies risk factors associated with prescription and suggests safety improvement programs.
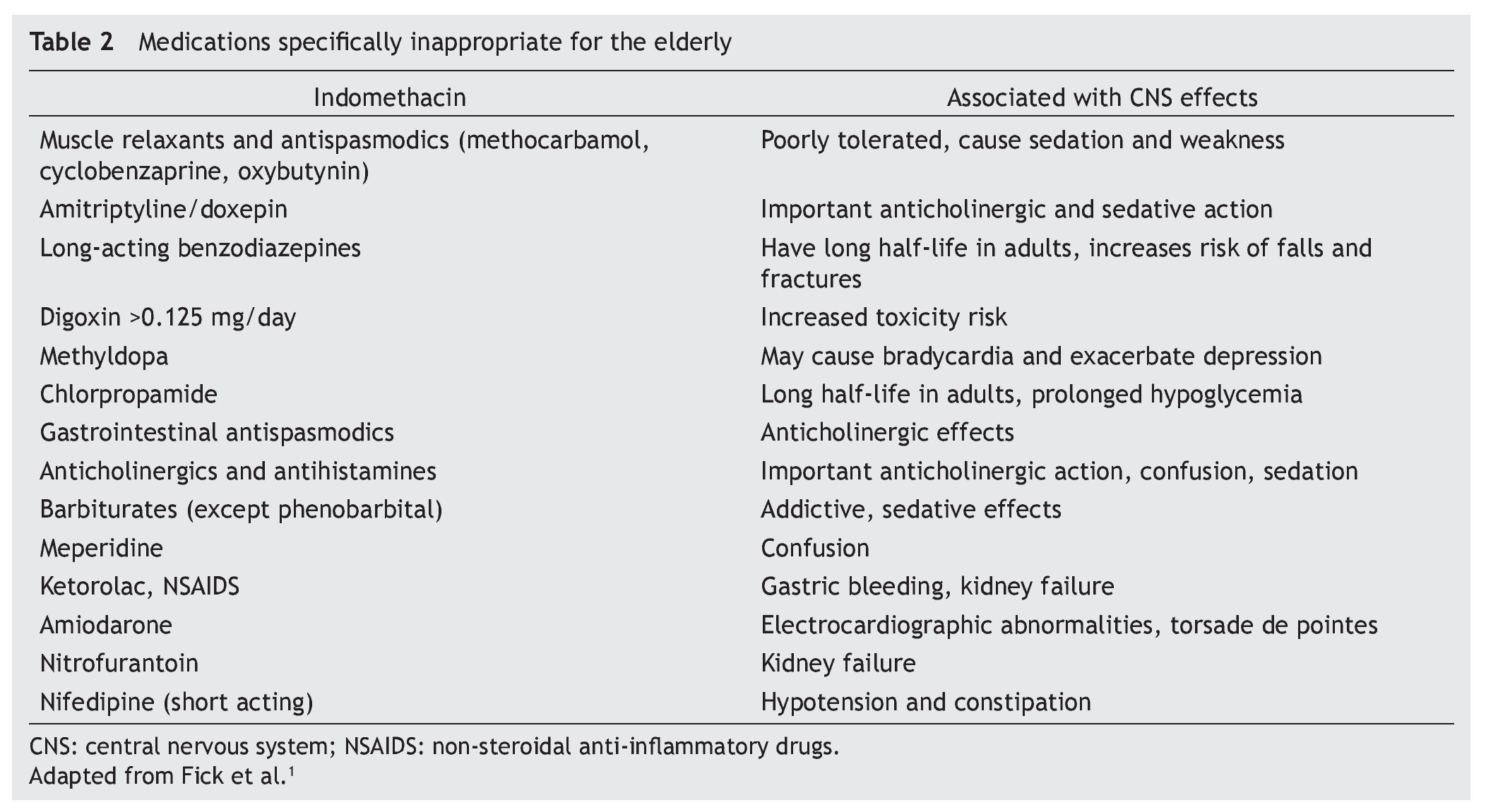
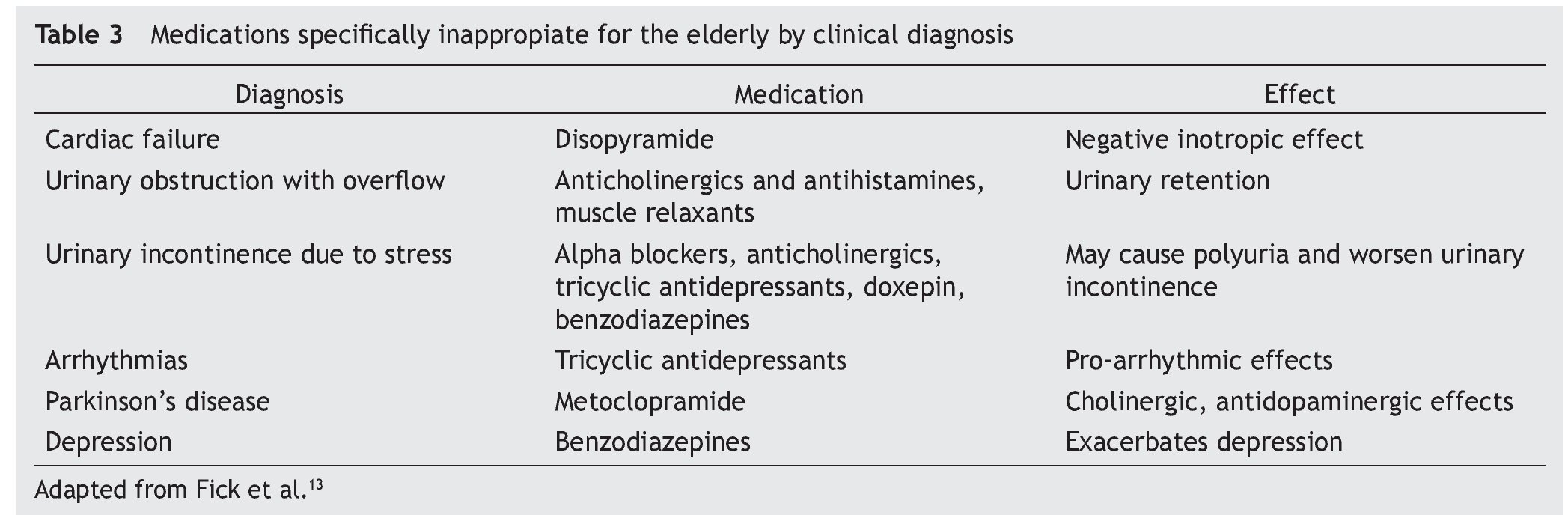
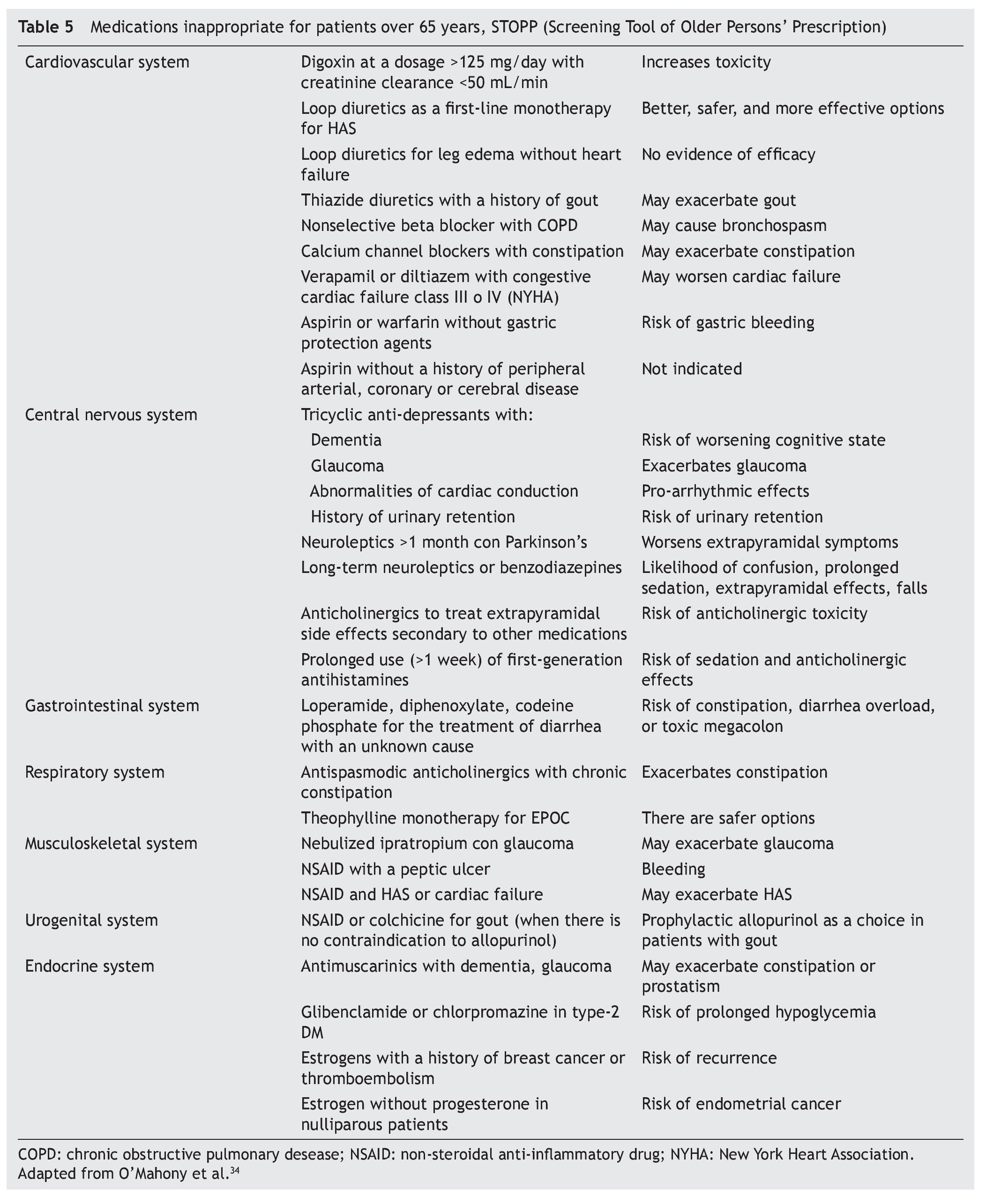
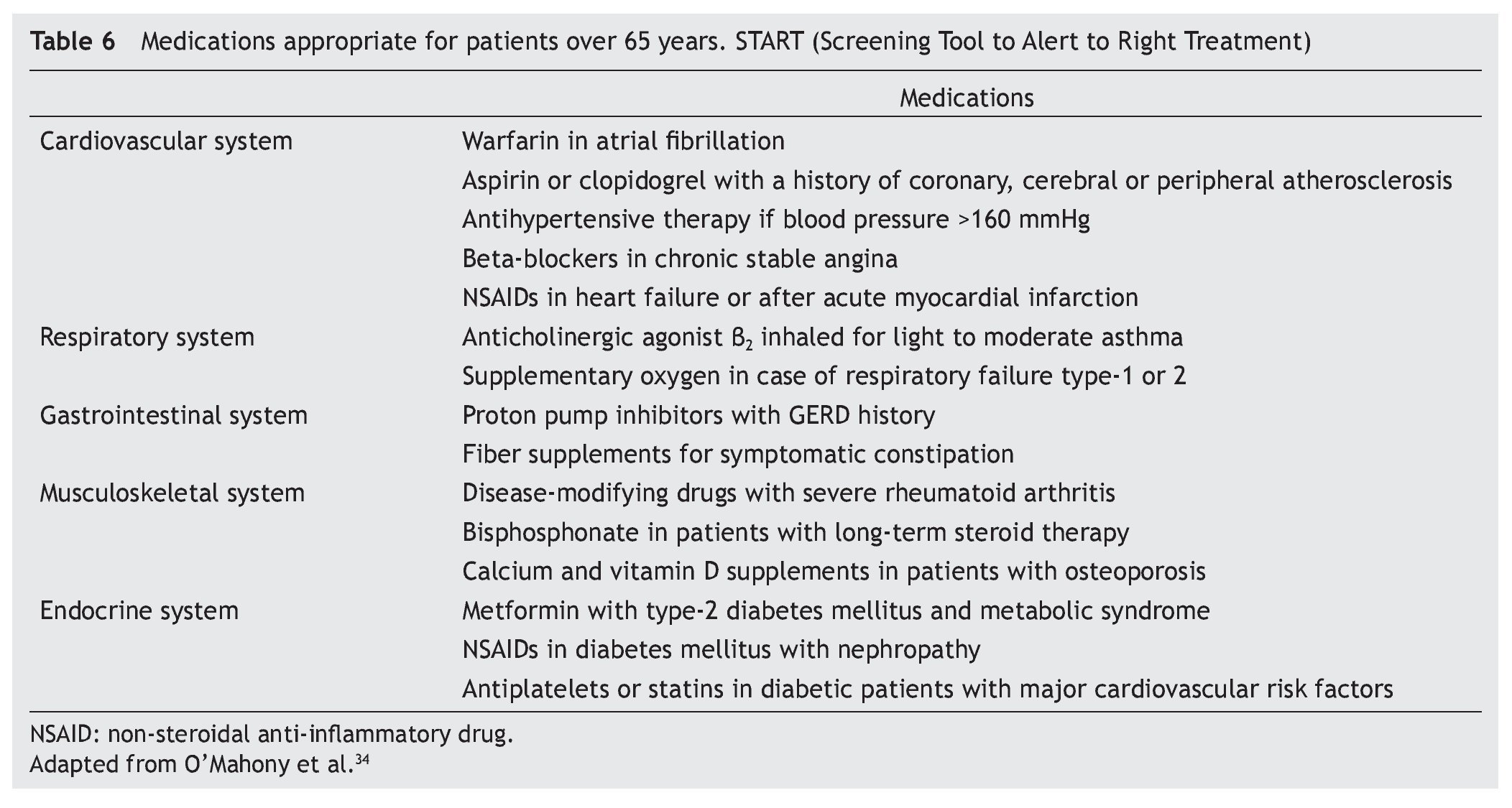
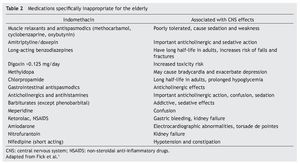
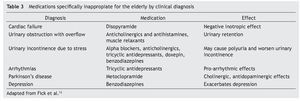
Beers’ criteria grouped medications into two groups; medications which should be avoided by the elderly because of their inefficacy or representation of an unnecessary risk, having other alternatives (table 2), and those medications which should not be used in the elderly even when they meet specific medical requirements (table 3). Moreover it stresses the importance of identifying prescription cascade.13
Medications mostly implicated in adverse events are cardiovascular, antibiotics, diuretics, anticoagulants, hypoglycemiants, steroids, opiates, anticholinergics, benzodiazepines and non-steroidal anti-inflammatory, among others.
While Beers’ criteria is very useful, there are some limitations in their use. Some medications listed as inappropriate, may have acceptable applications; likewise, there are medications which are not included and may confer risk with their use.7,31,32
The InterRAI Corporation is a network of researchers and clinics from 30 different countries around the world, and it has developed and standardized instruments for geriatric care currently being used in many countries. These instruments provide valid scales in geriatric patients, important in clinical practice, which may have a positive effect on individual care and treatment.7,33
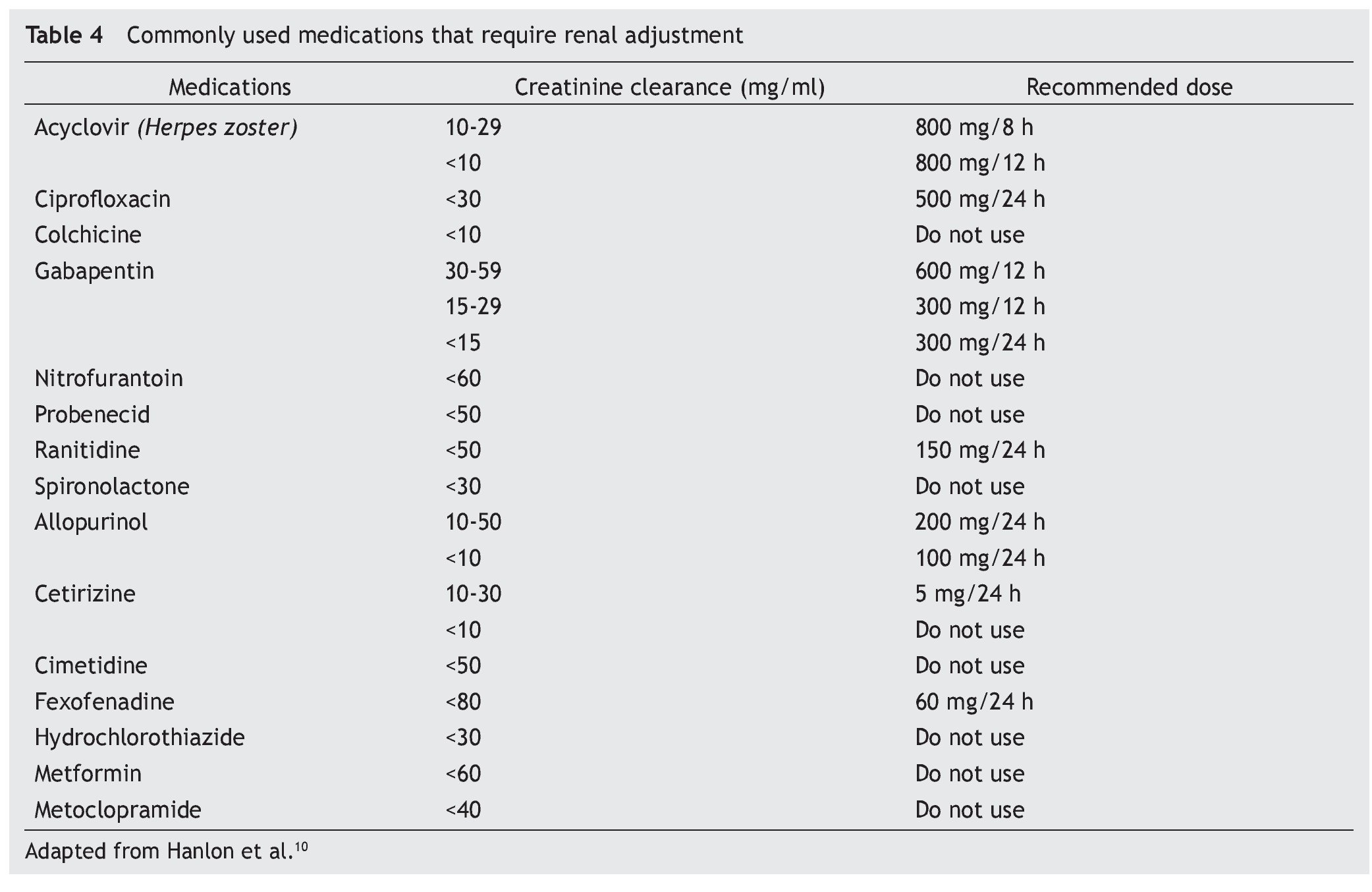
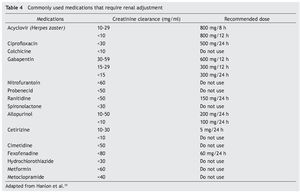
In 2009, Hanlon et al conducted a consensus in order to establish guidelines for the use of oral medications with renal elimination used in the elderly. The obtained results were in the form of two recommendations, medications which should be avoided in patients with a renal function of <30 mL/min like chlorpropamide, colchicine, cotrimoxazole, glyburide, meperidine, nitrofurantoin, probenecid, propoxyphene, spironolactone and triamterene; and those which require dosage reduction or a more ample administration interval, like acyclovir, amantadine, ciprofloxacin, gabapentin, memantine, ranitidine, rimantadine and valacyclovir. Frequently used medications which require renal adjustment can be found in table 4.
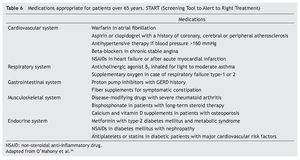
Two identification tools to identify mistakes in prescriptions for the elderly were developed with the use of the English acronyms STOPP (screening tool of older persons’ prescription) and START (screening tool to alert to right treatment); identifying those medications which should be avoided, as well as those appropriate in the treatment of the elderly. The most commonly used medications are mentioned in tables 5 and 6.34 These studies proved that the potential omission of adequate medications in the elderly is as prevalent as the inclusion of inappropriate medications which should be avoided.5,34 A multidisciplinary team allows for a better quality in the attention of the elderly, and adequate prescriptions and an optimal control with a decrease of AMR.
Education for prescriptions and general standards
The challenge in prescribing medicine to the elderly
The elderly have approximately 3 times more prescriptions than younger people. While the metabolism characteristics of geriatric patients which affect medication pharmacology are not modifiable, the choice of medication, length of the treatment and dosages are decisions which depend on the doctor, and are factors which can be optimized with the right knowledge and proper training in the treatment of geriatric patients.
Every new medication must be evaluated in the following contexts: pharmacokinetic, pharmacodynamics and changes related to age regarding body composition and physiology.28
While on occasion there are differences between geriatric guidelines and clinical practices from country to country, and the prescription is strongly influenced by feedback strategies and national forms, it is important to harmonize clinical and political recommendations as well as effective measures applied to our population in order to improve medical prescription.
Planning of an integral systemic approach to the elderly and teaching strategies for continuous medical education, represent an essential component of a quality medical education.35-36 Some important points to consider, with the purpose of improving the quality of prescriptions in the geriatric population, are: to conduct an integral assessment of patients, in the medical, functional, mental and social aspects; to use medications of proven efficacy, known toxicity and with experience of use in the geriatric population, to periodically review medications prescribed by different doctors, including dosage and length; to avoid unnecessary medication; periodical monitoring and evaluation of therapeutic objectives and whether or not these are properly being met; prescribe medications with fewer adverse reactions and interactions; choose medications with easily recognizable presentations and administration intervals which allow for adequate compliance; search for the minimum effective dosage and increase progressively if necessary, as well as educate the patient and personnel responsible for their care on the proper administration, which avoids self-medication.8-9, 24, 35,36
Conclusions
The elderly present physiological changes which affect the pharmacology of the medications used. Pharmacological studies cannot always extrapolate a medicine’s effect on the elderly, thus the most important challenge is to achieve optimal pharmacotherapy individualization.
The application of consensus criteria during prescription helps the clinic in the decision-making process and functions as a tool to minimize problems associated with the use of medications. Prescription must be based on general standards or principles of the use of medications in the elderly, whose main objective is to decrease the use of multiple medications and increase safety and treatment adhesion.
Physicians who attend the elderly should integrate their individual clinical experience with the best external evidence and comprehensible information in prognosis, limitations, preferences, family support and cost of treatment. A multidisciplinary approach and assistance coordination are indispensable in order to optimize this process.
Received: November 2013;
Accepted: July 2014
*Corresponding author:
Servicio de Dermatología,
Hospital Universitario “Dr. José Eleuterio González”,
de la Universidad Autónoma de Nuevo León,
Ave. Francisco I. Madero Pte. s/n y Ave. Gonzalitos, Col. Mitras Centro,
C.P. 64460 Monterrey, Nuevo León, México.
E-mail address:lorale@hotmail.com (A.L. Tamez Peña).