Patent ductus arteriosus (PDA) in premature infants after birth is associated with an increased risk of morbidity and mortality. Indomethacin or ibuprofen are the current treatments, with success rate of 70–85%, but also show severe side effects.
ObjectiveTo demonstrate the success of intravenous paracetamol as a treatment for the hemodynamically unstable patient with ductus arteriosus closure, in a third level hospital in northeastern Mexico.
Subjects and methodsWe performed a cross-sectional, observational retrospective study. All patients brought to our department between March 2013 and September 2014 were included. We also included files confirming PDA through the Yeh criteria and echocardiographic data before and after the patients took paracetamol.
ResultsTwenty-four files were included in our study. 4 of them were unable to close their PDA, with paracetamol so they had to go to surgical closure. Success in closing PDA with paracetamol was 83%, and we found significant differences in the PDA measurements (2.5 [±0.8] vs. 0.8mm [±1.1] mm, P<0.001), the left atrium/aorta ratio, the right to left shunt, and ductus arteriosus/aorta ratio before and after treatment. Sepsis and bronchopulmonary dysplasia were found in 100% of patients who failed treatment, compared to 40 and 25% in the success group respectively. No side effects were present in any of the patients.
ConclusionsThe use of paracetamol for ductus arteriosus closure could be effective, economical and with fewer side effects than current treatments.
Patent ductus arteriosus (PDA) in premature infants is linked to a greater risk of morbidity-mortality.1,2 Incidence in premature infants is 8 per 1000 live births, and it is reported to occur in almost 80% of neonates with a weight lower than 1200g.3,4
Currently, there are few pharmacological options, which are limited to cyclo-oxygenase non-selective inhibitors (COX), as well as adding liquid and diuretic restrictions to treatment.5
Indomethacin and ibuprofen are pharmaceuticals which promote PDA closure (with a success rate of 70–85%), with multiple side effects such as digestive tract bleeding, intestinal perforation, hyperbilirubinemia and renal failure. Thus, its use may also be contraindicated in a large population of hemodynamically unstable premature newborns, in addition to its high cost.6
In recent years, paracetamol has been suggested as treatment for PDA closure, since it acts in the reduction of the co-substrate for the production of prostaglandins with fewer side effects.7–9 In our field, surgical closure is the gold standard, since the access to medications such as I.V. indomethacin and ibuprofen are limited due to import issues on behalf of suppliers. The objective of this study is to determine the efficacy of PDA in patients treated with paracetamol in a tertiary care hospital in northeastern Mexico.
Materials and methodsAn observational, descriptive, retrospective study was conducted in the Neonatology Service of a tertiary care hospital in northeastern México, between March 1st, 2013 and September 1st, 2014. The study was reviewed and authorized by the institution's Ethics Committee.
A review of our files was performed, including those where diagnoses of hemodynamically unstable PDA were documented and treated with paracetamol for the period mentioned above. We included files of preterm infants at ≤36 weeks of gestation with clinical evidence of hemodynamically unstable PDA as the only cardiovascular diagnosis classified through the Yeh criteria and an echocardiography.10 Amongst the Yeh criteria, there are the following parameters: tachycardia, wide pulses, active precordium, reduced diuresis, a cardiothoracic index greater than 0.6. Murmurs are often present, as is the need for mechanical ventilation or an increase of the parameters of the ventilator. A total of 3 or more criteria suggests PDA with hemodynamic repercussions.
The echocardiogram was performed in every patient prior to and after treatment with paracetamol, taking into account all data which defines the magnitude of the ductus arteriosus, such as ductal dimensions >1.5mm, left atrium to aorta ratio (LA/Ao) >1.3mm, the presence of left to right short-circuits and a ductus arteriosus-aorta ratio >0.5.11
Files that showed PDA, but without hemodynamic repercussions or with additional pathologies like congenital cardiopathies, were excluded.
In the included files, a treatment with paracetamol at 15mg/kg/dose every 6h for 6 days was documented as a first line of treatment for hemodynamically unstable PDA closure, since access to intravenous medications such as indomethacin or ibuprofen was limited due to importation problems on behalf of the supplier, leaving this as the only alternative for treatment through pharmacological closure with paracetamol and, if this failed, we turned to surgical closure. Additionally, a control echocardiography was documented in every file at the end of the 6-day period.
Patients were divided into two groups for their analytical comparison. The first group was made up of patients who had been successful in the treatment with paracetamol, whereas the second group was made up of patients for whom treatment had failed and required surgery.
Moreover, statistical analysis included more other variables like maternal aspects of prenatal control, clinical characteristics of the newborn, and morbidity and mortality data, such as hyaline membrane disease (HMD), sepsis, bronchopulmonary dysplasia (BPD), intraventricular hemorrhaging (IVH), and retinopathy of prematurity (ROP).
The statistical software SPSS version 20 was used. Non-parametric tests were administered (Chi square) with an alpha value of 0.05, and the null hypothesis was rejected when the critical value was lower than 0.05.
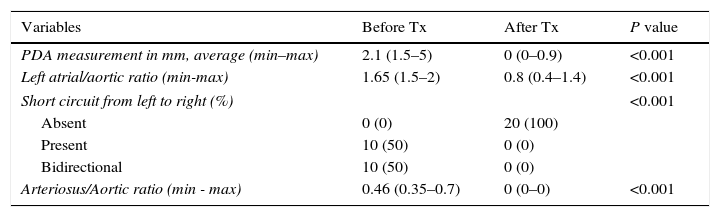
ResultsA total of 24 charts reporting hemodynamically unstable PDA treated with paracetamol were obtained during the period from March 1st, 2013 to September 1st, 2014. The effectiveness of the closure of the ductus arteriosus with paracetamol was 83.3% (in 20 patients), finding a significant difference in the measurements of the diameter of the ductus arteriosus before and after the treatment (2.5 [±0.8]mm vs. 0.8 [±1.1]mm, P<0.001).
The mothers’ ages ranged from 13–38 years, with a maximum of 3 pregnancies. Seven of the mothers (29%) presented some pain during pregnancy, emphasizing urinary tract infections and preeclampsia. Of all mothers, 79% had adequate prenatal care.
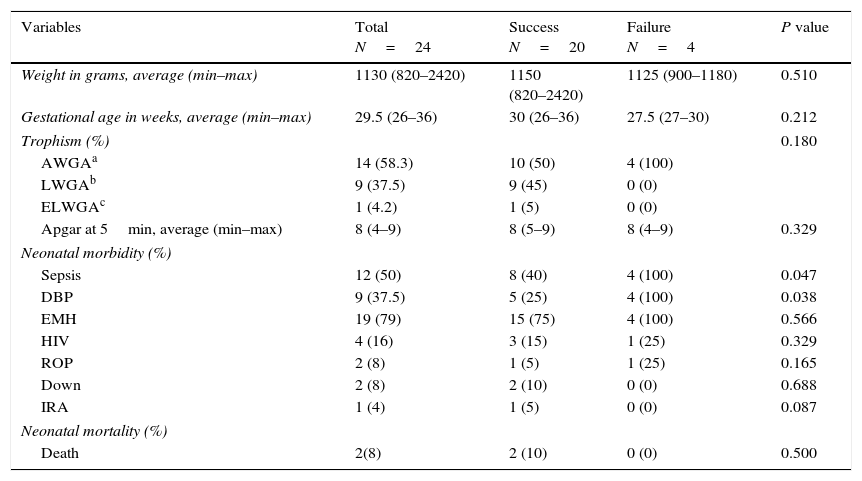
Of the population studied, 13 patients were female (54%), and 11 were male (46%). The gestational age between the treatment failure and success groups was not found to be statistically significant (30 vs. 27.5s) (P=0.212), nor was their weight in grams (1150g vs. 1.125g) (P=0.510).
Weight was also classified according to trophism as follows: appropriate for gestational age (AGA), small for gestational age (SGA), and large for gestational age (LGA), without statistical significance. Apgar at 5min was very similar in both groups, with a minimum score of 4 and a maximum score of 9 points (P=0.329). Regarding neonatal morbidity, it was noted that after failing to respond to paracetamol treatment, neonatal sepsis obtained a significant value (P=0.047), compared to 40% of patients that were successfully treated. In addition, DBP was found in 100% of failures of treatment with paracetamol vs. 25% in successful patients, giving a P value = 0.038 (see Table 1).
Characteristics of the newborn.
| Variables | Total N=24 | Success N=20 | Failure N=4 | P value |
|---|---|---|---|---|
| Weight in grams, average (min–max) | 1130 (820–2420) | 1150 (820–2420) | 1125 (900–1180) | 0.510 |
| Gestational age in weeks, average (min–max) | 29.5 (26–36) | 30 (26–36) | 27.5 (27–30) | 0.212 |
| Trophism (%) | 0.180 | |||
| AWGAa | 14 (58.3) | 10 (50) | 4 (100) | |
| LWGAb | 9 (37.5) | 9 (45) | 0 (0) | |
| ELWGAc | 1 (4.2) | 1 (5) | 0 (0) | |
| Apgar at 5min, average (min–max) | 8 (4–9) | 8 (5–9) | 8 (4–9) | 0.329 |
| Neonatal morbidity (%) | ||||
| Sepsis | 12 (50) | 8 (40) | 4 (100) | 0.047 |
| DBP | 9 (37.5) | 5 (25) | 4 (100) | 0.038 |
| EMH | 19 (79) | 15 (75) | 4 (100) | 0.566 |
| HIV | 4 (16) | 3 (15) | 1 (25) | 0.329 |
| ROP | 2 (8) | 1 (5) | 1 (25) | 0.165 |
| Down | 2 (8) | 2 (10) | 0 (0) | 0.688 |
| IRA | 1 (4) | 1 (5) | 0 (0) | 0.087 |
| Neonatal mortality (%) | ||||
| Death | 2(8) | 2 (10) | 0 (0) | 0.500 |
Shows demographic variables as well as morbidity and mortality in the success and failure group.
As for neonatal mortality, it was documented that 2 patients who had been successful in treatment with paracetamol died 15–20 days after closing the ductus arteriosus. The death was due to other comorbidities such as sepsis, obtaining a value P=0.500, which was not significant.
A statistically significant reduction (P=<0.001) in the diameter of the ductus arteriosus was found, being between 1.5 and 5mm before treatment with paracetamol and between 0 and 0.9mm at the end of treatment.
There were also significant differences in echocardiographic parameters such as left/aortic atrial ratio, right to left short circuit, and ductus arteriosus/aorta ratio, with a P value of <0.01 (see Table 2).
Echocardiographic variables.
| Variables | Before Tx | After Tx | P value |
|---|---|---|---|
| PDA measurement in mm, average (min–max) | 2.1 (1.5–5) | 0 (0–0.9) | <0.001 |
| Left atrial/aortic ratio (min-max) | 1.65 (1.5–2) | 0.8 (0.4–1.4) | <0.001 |
| Short circuit from left to right (%) | <0.001 | ||
| Absent | 0 (0) | 20 (100) | |
| Present | 10 (50) | 0 (0) | |
| Bidirectional | 10 (50) | 0 (0) | |
| Arteriosus/Aortic ratio (min - max) | 0.46 (0.35–0.7) | 0 (0–0) | <0.001 |
All four echocardiographic variables measured before and after treatment are shown. Persistence of the ductus arteriosus.
Reports have recently been published on the use of paracetamol as a treatment for PDA, which is safer and cheaper compared to the already established treatment.
Although it is known that the standard gold treatment with ibuprofen and indomethacin has an adequate success rate, the use of these drugs has important contraindications for newborns, which include thrombocytopenia or intracranial hemorrhage (altered platelet activity), renal failure (due to decreased renal perfusion), necrotizing enterocolitis with co-administration of corticosteroids (risk of intestinal perforation) and hyperbilirubinemia (competitive union with albumin).12,13
Our study shows an adequate percentage of PDA closure using intravenous acetaminophen. Previous studies have been published in which paracetamol was also successful orally, as in the study by Yurttutan et al.,14 where he presented 6 cases, of which 5 patients were successful with the treatment, as well as in the study by Aikio et al.,15 which decreased the annual incidence of PDA after the introduction of paracetamol.
Data on pharmacokinetics and pharmacodynamics, including tolerance in preterm and term newborns, have also been studied and published.16 Another characteristic in favor of the use of acetaminophen is that premature infants have a lower risk of hepatotoxicity due to its use since the enzymes involved in the formation of the hepatotoxic metabolite of paracetamol remain immature.17
As early as 1985, Peterson RG showed the effects of analgesics associated with closure of the ductus arteriosus in utero in fetuses and newborns.18
Our project observed that the 4 patients who failed treatment with paracetamol presented sepsis and BPD during the time interval to stabilize and go to surgical closure. These pathologies associated with PDA are frequent, as demonstrated by Chiang et al.,19 where their results reported that 81% of patients had BPD, as well as a 25% rate of recurrent sepsis.
The explanation for this situation could be that due to the requirements of mechanical ventilation with high parameters in patients with PDA, the risk of in-hospital sepsis secondary to mechanical ventilation increases, so that integrating sepsis, prolonged mechanical ventilation, and oxygen therapy will predispose patients to BPD (see Table 1).
Currently, making the decision to start and manage PDA with any of the treatments is a challenge. The onset of treatment is controversial because of the large number of newborns that will recover without any management, and another important point is that the current treatments (ibuprofen, indomethacin and surgical closure) have high efficacy, but are not harmless, and the high risk of side effects in vulnerable preterm infants seems to make the decision more complicated. However, in this study, it is emphasized that treatment should be performed in hemodynamically unstable patients who have been evaluated both clinically and in an echocardiographic form. These patients are the best candidates for treatment with paracetamol over a cycle of 6 days.
ConclusionsThe success rate in the closure of hemodynamically unstable PDA with paracetamol was 83%. After the administration of acetaminophen, it was observed that the cardiac variables such as the left/aortic atrial ratio, the left to right short circuit and the ductus arteriosus/aorta ratio improved when compared to pre-treatment echocardiography.
The use of acetaminophen for the closure of the ductus arteriosus could be an effective, economical and accessible treatment, being able to be used as first line treatment, since it presents fewer collateral effects than the gold standard, and the geographical areas with limited resources would gain the most benefits.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo financial support was provided.
Conflict of interestThe authors have no conflicts of interest to declare on this project.