This study aims to develop a scale to measure the worry level of patients who will undergo gastrointestinal (GI) endoscopy with deep sedation, and to provide scientific references to alleviate their worries.
MethodBased on literature review, panel discussion, patient interview and expert consultation, we developed the first version of the scale. After two pre-investigations, the formal version of the scale was formed, and the reliability and validity were tested on 1389 respondents. Reliability was assessed by Cronbach's alpha. Construct validity was tested by confirmatory factor analysis (CFA) and the Spearman correlations analysis.
ResultsThe scale was composed of four dimensions: financial and time costs, sedation, examination, and psychology. It has 15 items. Reliability and validity were acceptable. The Cronbach's alpha of the whole scale was 0.959 and all the factor loadings were > 0.50. The Spearman correlations of the inter-dimensions ranged from 0.614 to 0.836, and the correlation coefficients between the dimensions and the total score were 0.795 to 0.957. The correlation coefficient between the total scale score and the APAIS was 0.833.
ConclusionsThis scale has good validity and reliability, which is useful for physicians and medical institutions to take appropriate measures to reduce patients' worries.
AbbreviationsAPAIS Amsterdam Preoperative Anxiety and Information Scale average variance extracted confirmatory factor analysis comparative fit index chi-square/degrees of freedom composite reliability gastrointestinal root mean square error of approximation Tucker-Lewis Index
Gastrointestinal (GI) endoscopy is widely performed in the diagnosis and treatment of digestive system diseases, with about 18 million procedures performed in the United States annually, and approximately 14 million per year in China (Forbes et al., 2021; Zhou et al., 2021). A 69% reduction in colorectal cancer incidence and 68% reduction in colorectal cancer mortality have been reported with colonoscopy screening (Săftoiu et al., 2020). Additionally, Japanese Guidelines reported a 47% reduction in gastric cancer mortality by endoscopic screening (Hamashima, 2018). The application of GI endoscopy undoubtedly greatly decreases the cost of treatment for patients and medical institutions. However, the current population coverage rate for GI endoscopy screening is not optimistic. In recent years, about one-third of the eligible population in the United States has not been screened in time (Pennazio et al., 2015).
As an invasive procedure, most patients undergoing GI endoscopy will experience some degree of discomfort (Sargın & Uluer, 2020). Using sedatives such as propofol has greatly reduced patients' discomfort, but in China, only 48.3% of patients underwent GI endoscopy with sedation (Zhou et al., 2021). Many factors prevent patients from performing GI endoscopy with sedation, such as worrying about insufficient sedation and potential side effects, lacking medical insurance to cover the examination fee, lacking knowledge about endoscopy, and worrying about the diagnosis (Pontone et al., 2022; Yang et al., 2018). Worry is a factor that may affect the patient's cooperation and tolerance of the procedure. Excessive worry or anxiety will increase the use of sedatives (Lee et al., 2019), then raise the medical risk for both patients and physicians, and make the procedure more difficult (Pontone et al., 2022). In addition, the patient's negative emotions during the procedure will also impact future follow-up and the willingness to receive repeated endoscopes (Forbes et al., 2021). Moreover, excessive worry will not only lead to insomnia, but also can aggravate the disease-related symptoms through brain-gut axis (Chellappa & Aeschbach, 2022; Ford et al., 2020).
Worry is characterized by negative thoughts about the future, poor control of attention, close concern about negative information and vague negative explanations (Arnáez et al., 2019; Capobianco et al., 2020; Feng et al., 2022). In the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), the term worry has been used as a major symptom of generalized anxiety disorder (Munir & Takov, 2022). Therefore, worry is a cognitive activity, and a part of anxiety (Hirai et al., 2008). We think that patients' perceptions about GI endoscopy with sedation are predominantly worried and have not yet reached anxiety. Thus, We use the term "worry" to indicate that it is sub-clinical phenomenon rather than pathological state (Green et al., 2003). However, previous studies generally applied anxiety scales such as Beck Anxiety Inventory (BAI) (Sargin et al., 2016), Spielberger's State-Trait Anxiety Inventory (STAI) (Sargın & Uluer, 2020), etc., to assess the anxiety level in patients prior to performing endoscopy.
Clinicians usually take steps to reduce patients' worry before the procedure. However, due to the lack of the understanding for patients' worry level, they sometimes fail to alleviate it effectively. Few criteria currently exist to measure the worry degree of patients about GI endoscopy with sedation. Therefore, we attempted to develop and validate a worry scale of GI endoscopy with sedation (deep sedation) to objectively assess patients' worry level. We hope that this study can provide a reference for physicians and medical institutions to take appropriate measures to reduce patient's worries about GI endoscopy with sedation.
MethodsThis study was approved by the Ethical Committee of the Third Xiangya Hospital of Central South University, China (received permission on October 28, 2022, No.22234).
Study populationParticipants were recruited from those who visited the department of gastroenterology in the Third Xiangya Hospital of Central South University or accepted the online scales from October 2022 to January 2023. Any outpatient or physical examination individual aged 18 years or older planning to undergo diagnostic GI endoscopy with sedation (deep sedation) was eligible for inclusion. Participants were excluded if they were unable to fill out the scale independently or were unwilling to participate.
Measurement toolsDemographic questionnaire: It included gender, age, living alone or not, education, income, experience with unsedated GI endoscopy and experience with sedation GI endoscopy.
Amsterdam Preoperative Anxiety and Information Scale (APAIS): The scale comprises of 3 dimensions and 6 items, with satisfactory psychological measurement properties. It is currently the most widely used preoperative anxiety scale in clinical practice. In addition, it has been translated into Chinese and tested for reliability and validity. Furthermore, its effectiveness in assessing preprocedure anxiety for patients in China has been demonstrated (Wu et al., 2020). APAIS was used for the calibration validity test.
Study designThe scale was developed in three phases. First, we developed a provisional scale through literature review, panel discussion, patient interview and expert consultation. Second, two pilot surveys were conducted to adjust the dimensions and items of the scale. Third, we carried out a formal questionnaire with larger sample size, and the final scale was fitted with APAIS for verification (Fig. 1).
Phase 1: questionnaire developmentIn Pubmed, Web of Science, Google academic and other websites, we used “worry”, “concern”, “apprehension” and “endoscopy” as keywords to collect resources. Based on literature review and panel discussion, 5 dimensions and 13 items were identified. Subsequently, we conducted cognitive interviews with patients and consulted experts in statistics and gastrointestinal fields. According to the results, we revised the dimensions and related items and preliminarily determined 5 main impact domains: price and convenience, sedation, procedure and results, medical norms, and psychology. Then we developed 2–5 items in each dimension, for a total of 18 items.
Phase 2: pre-investigationTwo pre-investigations were conducted. The first pre-investigation received 239 valid questionnaires and the second received 200. We analyzed the reliability, validity, and inter-dimensional correlations, and performed descriptive analysis of demographics. After the first pilot test, we removed the dimension of medical norms and made appropriate adjustments to the items, reducing the number of items from 18 to 16. After the second pilot test, we combined two items with overlapping concepts and formed a scale with 15 items.
Phase 3: formal data collectionThe formal scale consisted of three parts. The first part was designed to collect personal characteristics of the respondents. The second part consisted of 15 items, each using a 5-point Likert scale ranging from 5 (extremely worried) to 1 (not worried at all), to assess the worry level of patients about GI endoscopy with sedation. The third part was the APAIS. We delivered the questionnaires in both paper and electronic format. The respondents participated voluntarily, and all data were confidential and anonymous. A total of 1389 valid questionnaires were received to test the reliability and validity of the scale.
Statistical analysisWe used IBM SPSS statistical software package version 23.0 (IBM, Armonk, NY) for data analysis.
Reliability: Cronbach's alpha was used to examine the internal consistency. In general, values above 0.7 indicated good internal consistency (Tian et al., 2022).
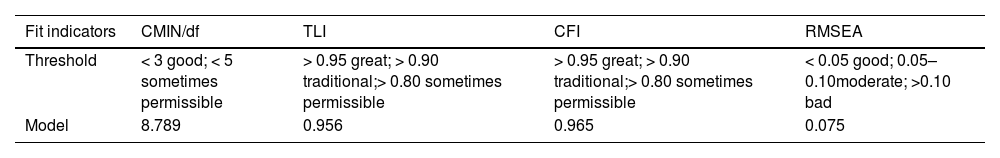
Validity: Correlation analysis and confirmatory factor analysis (CFA) were applied to evaluate the criterion validity and construct validity of the scale. Bartlett test of sphericity scores 〈0.05 and a KMO score of 〉 0.70 for the degree of sampling were considered suitable for factor analysis (Zhang et al., 2021). Indices such as chi-square/degrees of freedom (CMIN/df), root mean square error of approximation (RMSEA), comparative fit index (CFI), and Tucker-Lewis index (TLI) were used to evaluate the model fit.
ResultsRespondent characteristicsOf the 1389 respondents, 525 are male (37.80%) and 864 are female (62.20%). The majority are aged between 21 and 60 (1261, 90.78%). Most of the respondents do not live alone (1217, 87.62%). In terms of education, the largest number is graduate (545, 39.24%), followed by intermediate (291, 20.95%). Regarding to the monthly income, the distribution of the respondents is as follows: ¥2000 and below (272, 19.58%), ¥2001–4000 (440, 31.68%), ¥4001–6000 (354, 25.49%), ¥6001–8000 (148, 10.66%), ¥8001–10,000 (82, 5.90%), ¥10,001 and above (93, 6.70%). The majority of participants had no experience with unsedated GI endoscopy (1127, 81.14%) or sedation GI endoscopy (1027, 73.94%). Respondent characteristics are shown in Table 1.
Demographic profile of the respondents (n = 1389).
Note. GI, Gastrointestinal Endoscopy.
For the population factors, significant differences exist between respondents with different gender in the three dimensions of “Sedation”, “Examination”, “Psychology” and the total score of the scale (P < 0.01). Women show a higher level of worry according to the total score. All dimensions and the total score are significantly different by age, income, experience with unsedated GI endoscopy, and experience with sedation GI endoscopy (P < 0.05). Regarding the living situation, the significant difference is found in the dimension “Financial and time costs” (P < 0.05), but no significant difference in the other dimensions and the total scale score. Education shows a significant difference with the dimension “Examination” only (P = 0.034). (Table 2)
Differences in worry degree of the demographic.
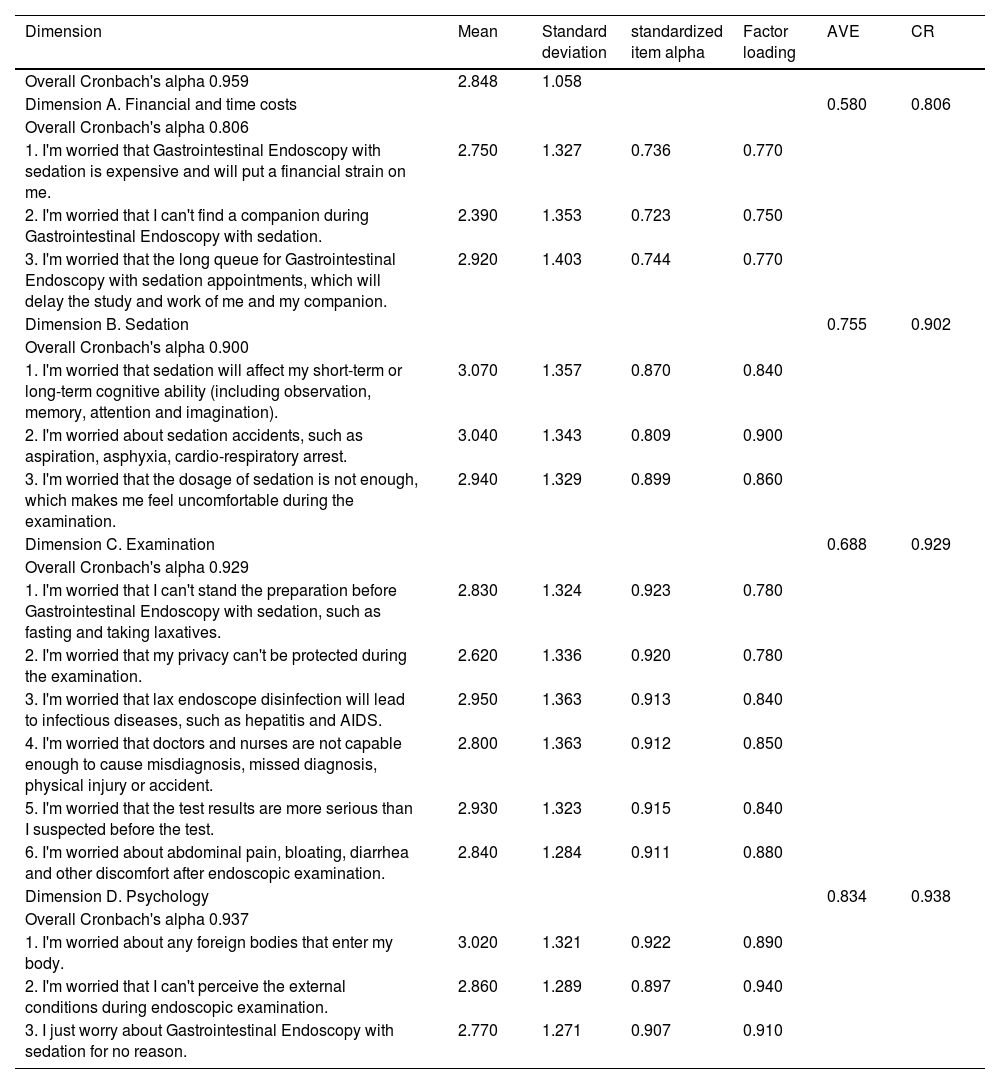
The scale exhibits satisfactory reliability with the value of Cronbach's alpha being 0.959 for the whole scale. The values of Cronbach's alpha for the 4 dimensions are 0.806, 0.900, 0.929, and 0.937, respectively, all of which are >0.80, demonstrating that the scale has good internal consistency (Table 3).
The descrptive figures of 15 items for each of the 4 dimensions of the scale.
Note. AVE, average variance extracted; CR, composite reliability.
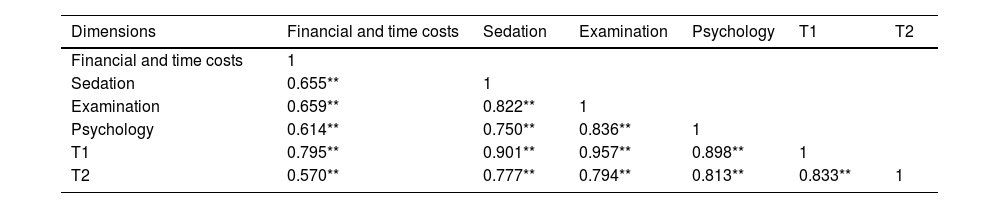
The results of the correlation analysis and CFA indicate acceptable construct validity of the scale. As shown in Table 4, “Financial and time costs”, “Sedation”, “Examination”, “Psychology”, total score of the Worry Level Scale (T1), and total score of the APAIS (T2) are significantly correlated at the α= 0.01 level, with Spearman correlation coefficients of 0.570–0.957. “Financial and time costs”, “Sedation”, “Examination”, “Psychology”, and T1 are 0.795, 0.901, 0.957, and 0.898, respectively, with inter-dimensional correlation coefficients ranging from 0.614 to 0.836, both of which are higher than 0.400 and inter-dimensional correlation coefficients are smaller than dimension-total scores correlation coefficients. APAIS is used as the criterion validity of the formal scale. The correlation coefficient between T1 and T2 is 0.833, and the correlation coefficients between the 4 dimensions and T2 are 0.570, 0.777, 0.794, and 0.813, respectively, which are all higher than 0.400, suggesting good criterion validity. KMO = 0.959, Bartlett's test value = 18,566.076, p < 0.001 indicate that the scale could be subjected to confirmatory factor analysis. Table 5 reports that the model fit of the scale is acceptable. In addition, estimate is 0.750–0.936 (>0.5), and composite reliability (CR) is 0.806–0.938 (>0.6), indicating that the scale has acceptable convergent validity and combined reliability.
Spearman correlations of inter-dimension and dimension-total score.
Note. **The correlation is remarkable at α = 0.01 (double end);T1, Total score of Worry Scale;T2, Total score of Amsterdam preoperative anxiety and information scale.
The assignment of each item can be up to 5 points. Thus, the total score of the Gastrointestinal Endoscopy with Sedation Worry Level Scale could range from 0 to 75. Based on the quartile, patients are classified into 4 levels of worry. 0–18 is minimal, 19–37 is mild, 38–56 is moderate, and 57–75 is severe. According to the total score of the Gastrointestinal Endoscopy with Sedation Worry Level Scale, 10.2% patients represented a minimal level of worry, 26.1% mild worry, 43.8% moderate worry, and 19.9% severe worry.
DiscussionClinically, most patients have reported worry before undergoing GI endoscopy with sedation (Sargın & Uluer, 2020). The worries reduce the willingness and compliance to the procedure, leading to the delay of diagnosis and treatment. Beside, it may even affect the physical condition of patients themselves. Here, we first developed a scale to assess the level of patients' worry about GI endoscopy with sedation. The scale was relatively reasonable and comprehensive, consisting of 4 dimensions (financial and time costs, sedation, examination and psychology) with a total of 15 items. We validated it with a large sample of 1389 respondents and the scale finally exhibited good reliability and validity.
According to the previous study, 73.3% patients considered cost as a critical factor when deciding whether to undergo GI endoscopy with sedation (Zhou et al., 2021). In addition, the increased demand for GI endoscopy will prolong the waiting time for patients (Aljebreen et al., 2013). Therefore, we used financial and time costs as a dimension. Studies assessing patients' anxiety in relation to GI endoscopy have shown that patients are worried about sedation (Lauriola et al., 2019; Yang et al., 2018). Sedation is a drug-induced suppression of consciousness. While the use of sedation can reduce the pain and discomfort for patients, it can also lead to adverse events such as hypotension and respiratory depression (Early et al., 2018; Goudra et al., 2020), as well as inadequate doses of sedation. For the third dimension, examination, abundant studies demonstrated the support for this finding (Lauriola et al., 2019; Taylor et al., 2003). We evaluated it in three aspects: before, during, and after the procedure. Endoscopy is a highly stressful procedure and is strongly associated with psychological cues (Brandt, 2001). Therefore, we assessed psychology as one dimension. In addition, The scale was developed smoothly. With slight adjustment of dimensions and items, the scale showed good reliability and validity, which may be attributed to our large sample size. Additionally, the CMIN/df in construct validity is relatively large, which could also be explained by the sample size.
The scale can help physicians further concretize patients' worries into specific items, and determining which dimension patients are more worried about. This will contribute to take personalized measures to alleviate the worries. For example, patients who are more worried about the examination process can use Virtual reality technology to decrease their worries (Chen et al., 2021). If patients are more worried about the anesthesia of GI endoscopy with sedation, a detailed explanation about anesthesia is necessary. Moreover, degree of worry may also guide clinicians to choose appropriate measures. For patients with minimal worry, slight intervention, such as oral comfort from medical staff may alleviate their worries. However, for patients who are severely worried, more frequent and effective interventions are needed to truly achieve the purpose of alleviating the worry degree. We believe that the scale can accurately assess the worry level of patients undergoing sedation GI endoscopy. It is hoped that our study can instruct personalized interventions to decrease the worry level. This is also the direction we need to research and explore in the future.
Patients' emotion not only affect themselves but also interfere with the physician's judgment and performance. It is recommended that the worry scale needs to be completed by patients prior to the procedure so that physicians can better understand patients' worry level and further take appropriate measures to alleviate it. The diagnosis and treatment are involved in cooperation between physicians and the patients. Physicians' worries also can impact patients. Therefore, in the follow-up research, we intend to develop a worry scale for physicians and then form a systemic scale to provide more references for clinical practice.
There are several limitations in this study. First, GI endoscopy includes many categories, such as gastroscopy, sigmoidoscopy, small bowel endoscopy, and ultrasound endoscopy. However, We have used a broad concept rather than a detailed classification. More studies are needed to explore the worry level of patients about different GI endoscopes. Secondly, our study was conducted at a single institution, which places some limitations on the generalizability of the scale. For better application in clinical practice, the reliability and validity of the scale should be tested in more healthcare institutions in the future. Additionally, more comparison should be conducted in practice between this scale and other mature anxiety-depression scales for further improvement. Thirdly, there is some controversy about the use of Cronbach's alpha because of its overly rigid assumptions and almost always violated. Also, its value may be affected by the sample size. Nevertheless, Cronbach's alpha is the most commonly used reliability index currently.
In conclusion, this study developed a scale to measure patients' worry level about GI endoscopy with sedation. The scale consists of 4 dimensions with 15 items and has high reliability and validity. It is a valid tool for studying the worry level and further guiding physicians and medical institutions to take appropriate measures to reduce patients' worries.
Author conflict of interest/study supportGuarantor of the article: Li Tian
Specific author contributionsXiaoyu Yu: research idea, study design, data acquisition, data analysis, and interpretation and drafting the manuscript. Haijun Deng: research idea, study design, supervision and mentorship, and critical revision of the manuscript. Ziyi Xiong: data analysis, and interpretation and drafting the manuscript. Pan Gong, Mingmei Ye, Tao Liu, Xiuyan Long: patient inclusion, data acquisition and interpretation. Li Tian: research idea, study design, supervision and mentorship, and critical revision of the manuscript. Each author contributed important intellectual content during manuscript drafting or revision and approved the final draft.
FundingThis work was supported by the Natural Science Foundation of Hunan Province (2021JJ31021) and the Scientific Research Program of Human Administration Bureau of Chinese Medicine (D2022026), China.
Potential competing interestsNone.