Los trastornos interiorizados o exteriorizados durante la niñez tienden a persistir cuando no se tratan y conllevan mayor riesgo de consecuencias negativas. El costo social incluye deserción escolar, desempleo, desintegración familiar y abuso de drogas. Las intervenciones preventivas efectivas requieren un enfoque de salud pública. El objetivo de este estudio experimental fue evaluar la eficacia del Programa Infantil Parents Plus (PPCP, por sus siglas en inglés) que se aplicó en contextos comunitarios y escolares por profesionales de servicios básicos de ayuda. A los padres con niños de 6-11 años se les asignó aleatoriamente al Grupo de Tratamiento (n = 44) o Grupo Control (n = 31). La eficacia del tratamiento se evaluó mediante auto-informes. Después del tratamiento se registraron mejoras significativas, con efectos medianos a grandes, en el nivel de estrés relacionado con la crianza de los hijos, los problemas de comportamiento infantil y en la satisfacción de los padres. Los resultados se mantuvieron en un seguimiento a seis meses. Se avala la eficacia del PPCP como intervención comunitaria con potencial para prevenir problemas de conducta infantiles mediante apoyo ofrecido a los padres en la práctica de la crianza antes de que se arraiguen los problemas y se vuelvan críticos.
Childhood internalising and externalising disorders tend to persist when left untreated and place affected individuals at higher risk of compromised outcomes. The social costs include school dropout, unemployment, family breakdown and substance abuse. Effective preventive interventions require a public health approach. The aim of this experimental study was to evaluate the effectiveness of the Parents Plus Children's Programme (PPCP) delivered in community and school contexts by frontline professionals from diverse backgrounds. Participating parents with children aged 6 to 11 were randomly assigned to a Treatment Group (n = 44) or a no treatment Control Group (n = 31). The efficacy of training was assessed using self-report questionnaires completed by participants in both Treatment and Control groups. Significant post treatment improvements were recorded on measures of parenting-related stress, child problem behaviour and parent satisfaction with medium to large effect sizes. Treatment group results were maintained at six-month follow-up. These results support the efficacy of the PPCP as a community led intervention with potential to prevent and interrupt child behaviour problems through supported parenting practice, before problems become critical and entrenched.
The quality of parenting behaviour is thought to shape the emotional climate of the family and to play an important role in children's psychosocial development (Morris, Silk, Myers, & Robinson, 2007). Specifically, harsh parental practice, negativity and rejection have been widely associated with the development of child internalising and externalising behaviours (Berkien, Louwerse, Verhulst, & van der Ende, 2012; Cunningham & Ollendick, 2010; Furlong et al., 2012; Rogosch, Dackis, & Cicchetti, 2011). In fact the quality of the parent-child relationship is more influential than family structure or income in fostering children's social and emotional development (Nixon, 2012). Behaviouor problems are the most common reason for referral to psychological and psychiatric services in childhood (National Institute for Health and Clinical Excelence, NICE, 2006). In particular, associations have been reported between early disruptive behaviours, delinquency and school failure (Dodge, Greenberg, & Malone, 2008; Webster-Stratton, Rinaldi, & Reid, 2011) risk of criminality (Piquero, Farrington, & Blumstein, 2003) substance misuse (Clark, Parker, & Lynch, 1999; Disney, Elkins, McGue, & Iacono, 1999) and accelerated progression to polysubstance use (Mason, Kosterman, Hawkins, Haggerty, & Spoth, 2003). These troubled children have a tenfold risk of school drop-out (Cataldi, Laird, & KewalRamani, 2009) with about half of children identified as difficult at age three continuing to engage in disordered behaviour at age nine (Campbell, 1995). Disruptive problem behaviour in childhood is associated with later increased risks of inter-partner violence and with parenting difficulties (Raudino, Woodward, Fergusson, & Horwood, 2012).
Over time behavioural problems become stable and more difficult to treat (Bierman et al., 1996) and in financial terms cost various public services up to ten times more (Furlong et al., 2012). Predictably, these children with elevated symptoms of depression, general anxiety, fearfulness and social anxiety, find life less satisfying than their peers (Clefberg-Liberman, Altuzarra, Öst, & Ollendick, 2012). Parents of children with emotional and behavioural disorders need extra support to enable them to develop positive parenting strategies. Their experiences often include a greater financial load, interruptions to work, family conflict, fatigue and sadness (Taylor-Richardson, Heflinger, & Brown, 2006). Parent stress is significantly related to child internalising and externalising behaviours (Anthony et al., 2005) with detrimental effects to parent and child mental health (Meltzer, Ford, Goodman, & Vostanis, 2011). For example, Stormshak, Bierman, McMahon, and Lengua (2000) found that parenting practices that included punitive interactions was associated with elevated rates of all child disruptive behaviour. Halpenny, Nixon, and Watson (2010) found greater use of physical punishment among stressed parents. Kiff, Lengua, and Zalewski (2011) also reported evidence of this bidirectional relationship. Children high in irritability and impulsivity were found to be more vulnerable to the adverse effects of negative parenting. In turn, many negative parenting behaviours predicted increases in these characteristics.
Group-based pa renting programmes significantly reduce childhood behavioural problems, develop parenting competencies, improve parent-child interactions and reduce parental stress (Barlow, Smailagic, Ferriter, Bennett, & Jones, 2012; Barlow, Smailagic, Huband, Roloff, & Bennett, 2012; Finzi-Dottan, Bilu, & Golubchik, 2011; Furlong et al., 2012; Hutchings et al., 2007; Scott & Dadds, 2009). A variety of evidence-based programmes that are effective in the management of early onset conduct problems have been developed (Hahlweg, Heinrichs, Kuschel, Bertram, & Naumann, 2010; Skerketich & Dumas, 1996). For example, a meta-analysis by McCart, Priester, Davies, and Azen (2006) of thirty parent training programmes and forty-one child focused programmes found that for children under twelve, parent training was significantly more effective than child focused programmes. Likewise, a review by Sandler, Schoenfelder, Wolchik, and MacKinnon (2011) of forty-six experimental parenting interventions also reported significant long-term benefits to mental, emotional and developmental health and behavioural competence.
Reaching sufficient numbers of those in need is challenging as some parents view Child and Adolescent Mental Health Services (CAMHS) as stigmatising (Hutchings & Webster-Stratton, 2004; Kilroy Kilroy, Sharry, Flood, & Guerin, 2011; 2011; Rooke Rooke, Thompson, & Day, 2004; 2004). Furthermore international estimates suggest that just 10% of children with problem behaviour access specialist services (Hutchings, 1996). A framework for overcoming these challenges is based on recent evidence validating the effectiveness of community-based parenting programmes (Hand, Ní Raghallaigh, Cuppage, Coyle, & Sharry, 2012; Hutchings, Bywater, Williams, Shakespeare, & Whitaker, 2009; Kilroy et al., 2011; McGilloway et al., 2012). This evidence confirms the utility of parenting programmes in preventing a wide range of problem outcomes while promoting competencies up to twenty years later (Sandler et al., 2011). In this regard, early intervention is key since it is more difficult to influence the developmental trajectory later in childhood (Bayer et al., 2011; Shonkoff & Phillips, 2000).
The Parents Plus Programmes are evidence-based parenting programmes based on social learning principles. There are three versions of the Programmes addressing the needs of parents of preschool (1-6), primary school age (6-11) and adolescents (11+). Several studies substantiate the efficacy of these programmes in reducing child hood behaviour problems and associated parental stress in a variety of contexts (e.g. Behan, Fitzpatrick, Sharry, Carr, & Waldron, 2001; Coughlin, Sharry, Fitzpatrick, Guerin, & Drumm, 2009; Griffin, Guerin, Sharry, & Drum, 2010; Hand et al., 2012; Kilroy et al., 2011; Quinn, Carr, Carroll, & O'Sullivan, 2007; Sharry, Guerin, Griffin, & Drumm, 2005). The current study concerns the Parents Plus Children's Programme (PPCP) (Sharry & Fitzpatrick, 2007). The PPCP equips parents with the skills for non-coercive approaches to parenting and teaches parents how to promote attachment, pro-social behaviour and assist their child with learning. DVD footage of parents who previously participated in the programme provides evidence of the relevance and effectiveness of the ideas. The PPCP is fully manualised and has an established process of facilitator training plus a quality delivery protocol which includes follow-up supervision and support. Weekly session rating forms completed by participants identify parents who may be struggling, keeps course content relevant to participant needs and informs programme adaptations. In a previous evaluation of the PPCP within a clinical setting, Coughlin et al. (2009) reported a significant decrease in child conduct problems and parental stress and an increase in parental confidence and parent-defined goals. Positive changes were maintained over five-months. A follow-up community study by Hand et al. 2012 on the effectiveness of a modified PPCP as an intervention for parents of children with mild intellectual disabilities found similar reductions is clinical range scores.
While the effectiveness of the PPCP as an intervention has been established in clinical settings (e.g. Coughlin et al., 2009; Hand et al., 2012) the literature does not address the effectiveness of the PPCP programme as a community based intervention. The current study aims to addresses this gap by evaluating the effectiveness of the PPCP when delivered to parents of children aged six to eleven in school and community settings by frontline professional staff who underwent facilitator training. Specifically, the study aims to: a) evaluate the effectiveness of the PPCP in this community context; b) determine whether improvements are maintained at six-month follow-up.
Method
Study design
This study employed a Randomised Controlled Trial (RCT) design with parallel-groups. Time (1, 2 and 3) and Group (Treatment and Control) were the independent variables. Pre and post-intervention data were analysed using a series of 2 x 2 mixed factorial ANOVAs conducted on all measures of interest (with alpha set at .05). The Statistical Package SPSS 19 was used to analyse the data. Each analysis compared results between the Control group (CG) and Treatment group (TG) (between subjects). The measures were obtained pre-intervention (Time 1 (T1)), post-intervention (Time 2 (T2)) and at six-month follow-up for the TG (Time 3(T3)) (within subject). The dependent variables included measures of child and parent psychological distress and difficulty.
Participants
Three primary schools were selected to take part in the study and a two day PPCP training was provided to study facilitators including Home School Liaison Teachers and Primary Care professionals. Parents of 125 children aged 6 to 11 years with children attending the schools, were given an open invitation. Families identified by school staff as 'most in need', were also targeted. Participating parents were randomly allocated to a TG (n = 44) or CG (n = 31) by an independent Research Assistant who was not otherwise involved in this research. No exclusionary criteria were applied. Only 10 fathers attended training (13%), out of a participant total of 75. Children of participants were not in receipt of clinical services at the time of the study. Following the 8-week training programme, 63 out of 75 (84%) participating families were successfully followed up (TG = 36 (81%); CG = 27 (87%)). Six months post training 20 out of 44 (45%) TG parents again completed questionnaires. This study was approved by the Ethics Committee at the Mater Hospital, Dublin.
Instruments
- The Strengths and Difficulties Questionnaire (SDQ) (Goodman, 1997) is a 25-item screening instrument relevant to the mental health and behaviour of children and adolescents aged 4 to 16 years. It has five subscales: Emotional Problems, Conduct Problems, Hyperactivity, Peer Problems and Pro-social Behaviour. Recently, Goodman and Goodman (2011) reported that SDQ mean total difficulty scores closely predict prevalence of clinical levels of child mental disorder at population level. The psychometric properties of the SDQ are well established (Goodman, 2001). In this study, total difficulty scores above 16 were considered to be borderline-clinical (Goodman, 2001).
- Parenting Stress Index/Short Form (PSI/SF). Parent stress was measured using the PSI/SF, a 36-item self-report instrument with 3 dimensions labelled Difficult Child, Parent Distress, and Parent-Child Dysfunctional Interaction. The instruments 5-point scale ranges from strongly agree to strongly disagree. Higher scale scores indicate greater caregiver stress. PSI/SF scores are stable over time, are internally consistent, and are significantly related to generalised distress (Haskett, Ahern, Ward, & Allaire, 2006; Reitman, Currier, & Sickle, 2002). Scores that were in the 85th percentile or higher were considered clinically meaningful and scores in 81st percentile or higher were judged in the borderline-clinical range as recommended by the developers of the PSI-SF (Abidin, 1995).
- The Kansas Parental Satisfaction Scale (KPS) (James et al., 1985) is a brief 3-item instrument that measures parent satisfaction. Parents respond on a seven-point Likert scale ranging from "extremely dissatisfied" to "extremely satisfied". The scale has good concurrent validity. Significant correlations have been found with the Kansas Marital Satisfaction Scale and the Rosenberg Self Esteem Scale (.23 to .55) (James et al., 1985). Scores of 15 or less indicate low parental satisfaction (DeCato Murphy, Donohue, Azrin, Teichner, & Crum, 2003).
- Parent defined goals. Prior to the intervention parents identified two personal parenting related goals and child related goals, as their desired outcome from the course. Parents were invited to indicate how close they were to achieving their goal by marking on a line from 0 to 10, where 0 represented very far away and 10 represented goal reached (Sharry & Fitzpatrick, 2007). Post training, parents rated their parent and child goals on the same scale.
Procedure
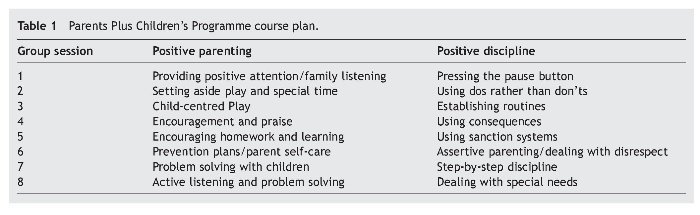
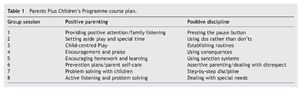
Facilitators, in conjunction with school Principals from 3 Irish Primary schools, sent an information sheet home in the schoolbags of 125 children, inviting parents to attend an information evening. Parents who attended (75/125 = 60%) self-selected to participate in PPCP training. Written informed consent was obtained before inclusion in the study. Parents completed baseline survey measures (Time 1). The same measures were administered on completion of training (Time 2) (63/125=50%). Participants attended 8 weekly 2.5 hour sessions of training. During each training session provided by two trained PPCP facilitators, a positive parenting strategy and a positive discipline topic was introduced, supported by video excerpts, discussion, role play and weekly planning. The PPCP was continuously adapted throughout training, to suit the needs of parents based on feedback received in session rating forms and on the stated goals of parents. Adaptations by facilitators are designed to build on the parents' strengths and feeling of success and aims to model an encouraging style of parenting. A sample course plan is presented in Table 1. CG participants took part in PPCP training following Time 2 data collection. This study follows the editing norms proposed by Hartley (2012).
Results
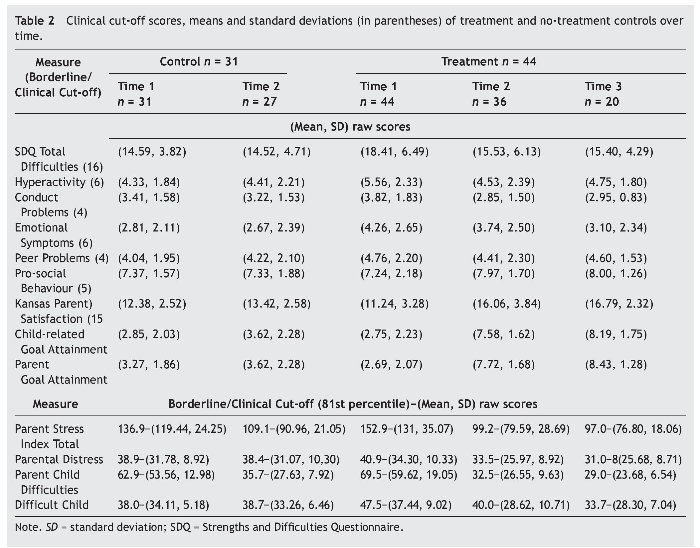
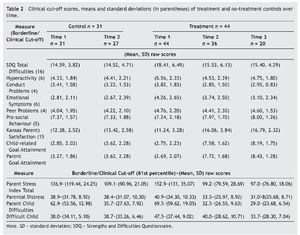
A series of 2 x 2 mixed factorial ANOVAs were conducted on all of the measures of interest (alpha = 0.05). Each analysis compared results between the CG and the TG (between subjects). The measures were repeated for Time 1 (T1) and Time 2 (T2) (within subjects) for the CG and for Time 1(T1), Time 2(T2) and Time 3 (T3) for the TG. Table 2 displays the measures, associated clinical cut-off points (81st percentiles for PSI measures) and the means and standard deviations over time. It is noteworthy that as the stress measures were improved post intervention, the 81st percentile of measures decreased as expected.
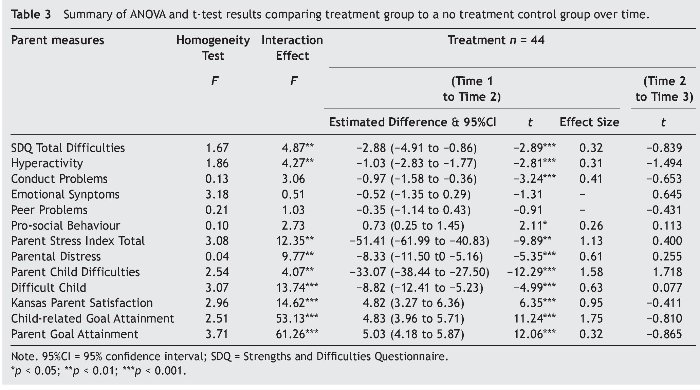
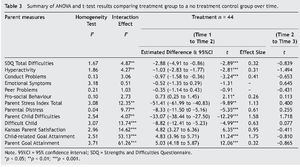
Table 3 displays the F for homogeneity test across groups, F statistic for Time x Group interaction effects and their associated p-values, result for paired sample t-test (T1 to T2 and T2 to T3), associated confidence intervals and effect sizes. TG results are also presented for estimated difference between measurements pre-intervention (T1) and post-intervention (T2). As only T1 and T2 were considered, the assumption of sphericity test is not required.
Strengths and Difficulties Questionnaire
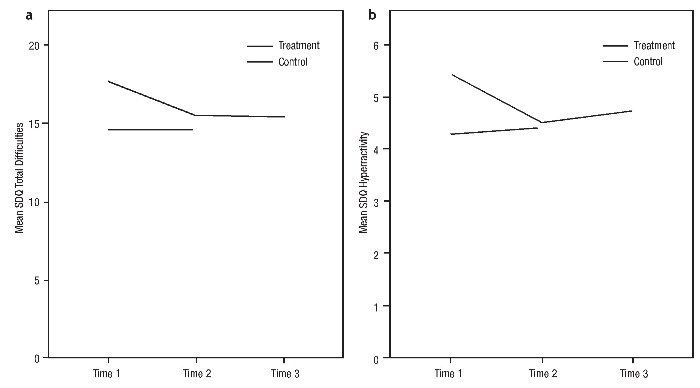
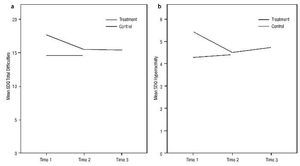
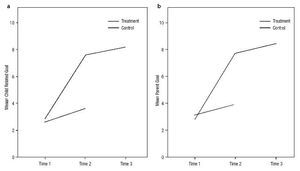
As can be seen from Table 3, there was a significant Time x Group interaction effect observed for the SDQ Total Difficulties (F 2, 25 = 4.87, p < .01) and the Hyperactivity subscales (F 2, 25 = 4.27, p < .01). The interaction effect was not significant for Conduct Problems (F 2, 25 = 3.06, p > .05), Emotional Problems (F 2, 25 =0.51, p > .05), Peer Problems (F 2, 25 =1.03, p > .05) and Pro-social Behaviour (F 2, 27 = 2.73, p > .05). Paired sample t-tests show a significant difference between measures on T1 and T2 for the TG Total Difficulties (t60 = -2.89, p < .001) Hyperactivity (t 60 = -2.81, p < .001) and Conduct Problems (t 60 = -3.24, p < .001) and Pro Social subscales (t 60 = 2.11, p < .05). TG results were maintained at six-month follow-up (T3) on all measures as evidenced by t-test scores presented in Table 3. Figure 1(a) presents the variation in SDQ Hyperactivity scores and Figure 1(b) presents group differences in Total Difficulties pre and post intervention. The CG ceased between T2 and T3 as they were given the PPCP training.
Figure 1 Strengths and Difficulties (SDQ) (a) Hyperactivity score and (b) SDQ) Total score for Treatment and Control groups' pre and post intervention and six-month follow-up.
Parent Stress Index
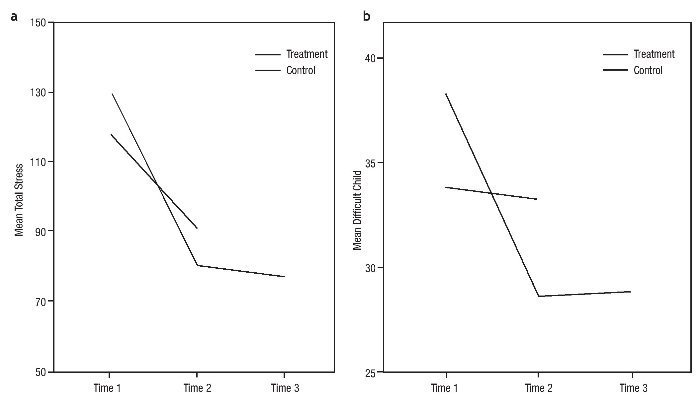
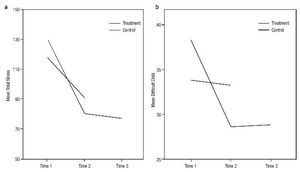
A significant interaction effect was observed on the PSI Total score (F2, 25 = 12.35, p < .01). The interaction effect was also significant for Parent Distress (F2, 25 = 9.77, p < .01), Parent Child Interaction Difficulties (F 2, 25 = -4.07, p < .01) and Difficult Child (F 2, 25 = 13.74, p < .001). Further analysis shown in Table 3 reveals that the Time effect was significant for the PSI Total score (t60 = -0.89, p < .001), Parent Distress (t 60 = -5.35, p < .001), Parent Child Interaction Difficulties (t60 = -12.29, p < .001) and Difficult Child (t60 = -4.99, p < .001), for the TG. TG improvements in scores were maintained at six-month follow-up as shown in Table 3. Figure 2(a) presents Treatment and Control group scores on the PSI Total and Figure 2(b) PSI Difficult Child at T1, T2, and T3. The CG ceased between T2 and T3 as they availed of the intervention.
Figure 2 Parent Stress Index (a) Total Score (b) Difficult Child for Treatment and Control groups' pre and post intervention and six-month follow-up.
The Kansas Parent Satisfaction Scale
The interaction effect was significant for the KPS Total score (F 2, 27 = 14.62, p < .001). There was a significant Time effect for the treatment group (t60 = 6.35, p < .001) and treatment gains were maintained at six-month follow-up (see Table 3).
Goals
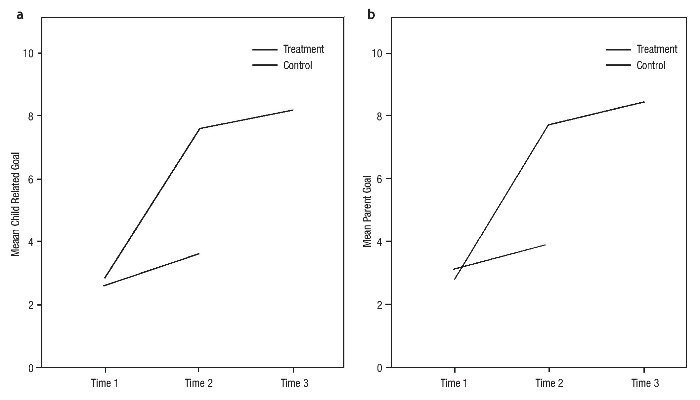
There was a significant Time x Group interaction effect observed for child related goals (F2, 25 = 53.13, p < 0.001) (see Table 3). The paired-samples t-test results displayed in Table 3 shows a significant Time effect from T1 to T2 (t60 = 11.24, p < .001) for the Treatment group. Figure 3(a) presents the variation in scores between Treatment and Control groups across time. There was a significant Time x Group interaction effect observed for Parent personal Goal (F2, 25 = 61.26, p < .001) as shown in Table 3. Paired-samples t-tests presented in Table 3 shows a significant Time effect for the TG from T1 to T2 (t60 =12.06, p < .001). Figure 3(b) displays Goal attainment for pre and post intervention and at six-month follow-up. In summary, significant Time x Group interaction effects were observed for: SDQ Total difficulties and Hyperactivity; PSI Total, Parent Distress, Parent Child Interaction Difficulties and Difficult Child subscales; Kansas Parent Satisfaction; and both the Child-related and Parent Goal attainment scales. While the pattern of results between T1 and T2 were similar, significant differences were observed for the TG only. Treatment group results were maintained at six-month follow-up.
Figure 3 (a) Child related Goal attainment (b) Parent personal Goal attainment for Treatment and Control groups' pre and post intervention and six-month follow-up.
Discussion
The PPCP is designed to enhance the skills of parents of children aged 6 to 11. The aim of the current study was to evaluate the effectiveness of the PPCP when delivered in community settings. No exclusionary criteria were applied. At baseline there was no significant difference between participants in the Treatment and Control groups on measures indicating that randomisation procedures were effective. The first study hypothesis was that delivery of the PPCP by varied professionals within different community settings would significantly benefit TG participants compared to a no treatment CG. This hypothesis was supported. The second hypothesis was that TG benefits would be maintained at six-month follow-up. This hypothesis was also supported. Significant TG improvements were evident on measures of child behaviour (SDQ), parental stress (PSI-SF), Parent Satisfaction (KPS) and parent and child related Goal attainment. Effect sizes for the significant post programme changes were moderate to large, indicating a practical application for the findings. These results suggest that the PPCP could be suitable as a preventative and supportive intervention for the parents of a majority of children delivered by a broad range of professionals in real world settings and to varied populations.
The SDQ was used to assess parent perception of child conduct. Compared to the CG, parents in the TG achieved significant improvements on the SDQ Total, Hyperactivity, Conduct Problems and Pro-social subscales post intervention. Importantly, mean scores post-treatment were in the (low-need) non-clinical range. Treatment gains were maintained at six-month follow-up. These results replicate post-treatment gains achieved in a clinical setting (Coughlin et al., 2009) and with parents of children with disabilities in a community setting (Hand et al., 2012). Not unexpectedly, baseline scores were in the SDQ 'some need' range, lower than in previous studies (Coughlin et al., 2009; Griffin et al., 2010; Hand et al., 2012) suggesting Borderline/Pre-Clinical problem levels for this group. This outcome provides initial evidence for the preventative and treatment potential of PPCP as a community based programme capable of addressing child conduct problems before they escalate to clinical levels.
The PSI-SF was administered to assess parent stress levels. Significant decreases in all scores was observed post-treatment for the TG with results maintained at six-month follow-up. Results were consistent with findings of Coughlin et al. (2009) and Hand et al. (2012). Interestingly, a decrease in scores was observed for CG, however improvements were significant for the TG only. It is possible that these positive changes within the CG were prompted by identifying their own parenting goals. Pre-intervention measures of Parent Satisfaction were low. This would suggest that parents who self-select to attend parent training have an insight into their own parenting needs. Post training, TG scores had significantly improved and were maintained at six-month follow-up, while CG scores decreased slightly. On measures of parent and child related goal attainment, parents in the TG showed significantly greater goal attainment. Gains were maintained at six-month follow-up.
These preliminary findings, while encouraging, must be considered in the context of some limitations. The conclusions rely solely on self report, as no observation data or teacher ratings were collected. The study is also limited by low participation rates of fathers (13%). In a previous study of the Parents Plus Programme, targeted at parents of older children, the attendance rate of fathers was 43 percent (Behan et al., 2001). In this study it is possible that daytime scheduling of training may have favoured mothers. Another limitation was the low numbers with data collected at the six month follow up. This was caused by practical limitations and lack of resources. Future studies would be strengthened by more complete data at follow-up. The question of whether parents of more troubled children or with more limited resources benefit to the same extent from programme intervention is important. It is possible that parents in more challenging situations may not have the time, resources or enthusiasm for participation. For some participants, these added challenges may undermine the potential of the programme. These preliminary, but positive results provide a compelling justification for a study replication.
The results of this study build on research by Coughlin et al. (2009) and Hand et al. (2012) providing initial indications for the utility of the PPCP as a preventative model of parent training, when delivered by varied professionals. The significant improvement in parent satisfaction and reductions in stress and child problem scores are important achievements over a relatively short intervention period. As the first community led trial this initiative provides evidence of the preventative potential within a new delivery framework. Quality of parenting is believed to shape the emotional environment of the family and play a critical role in children's psychosocial development (Morris et al., 2007) yet availability of parent training is for the most part constrained to clinical settings. Within the clinical context delivery is limited and more costly. This is compounded by reports suggesting that many of the most needy families do not seek referral (Hutchings & Webster-Stratton, 2004; Kilroy et al., 2011). Reaching sufficient numbers of parents in need with widely available, empirically supported parenting interventions requires a community led approach. The current study indicates that such an approach could have a positive public health impact, preventing and interrupting problems before they become critical. Relieving parent and child stress is likely to lead to reduced demand for clinical services, interrupt injurious developmental trajectories, and in the long run reduce intervention costs. It is anticipated that future research will clarify whether those with clinical versus non clinical scorers benefit equally from this type of community based training.
*Corresponding author at:
Mater CAMHS, James Joyce St. Dublin, Ireland.
E-mail address:jsharry@mater.ie (J. Sharry).
Received November 20, 2012;
accepted March 19, 2013
References
Abidin, R. R. (1995). Parenting stress index short form: Test manual. Charlottesville, VA: Paediatric Psychology Press.
Anthony, L. G., Anthony, B. J., Glanville, D. N., Naiman, D. Q., Waanders, C., & Shaffer, S. (2005). The relationships between parenting stress, parenting behaviour and preschoolers' social competence and behaviour problems in the classroom. Infant and Child Development, 14, 133-154.
Barlow, J., Smailagic, N., Ferriter, M., Bennett, C., & Jones, H. (2012). Group-based parent-training programmes for improving emotional and behavioural adjustment in children from birth to three years old (Review). Cochrane Database of Systematic Reviews, 6, 1-95.
Barlow, J., Smailagic, N., Huband, N., Roloff, V., & Bennett, C. (2012). Group-based parent training programmes for improving parental psychosocial health (Review). The Cochrane Collaboration, 6, 1-200.
Bayer, J. K., Rapee, R. M., Hiscock, H., Ukoumunne, O. C., Mihalopoulos, C., Clifford, S., & Wake, M. (2011).The Cool Little Kids randomised controlled trial: Population-level early prevention for anxiety disorders. BMC Public Health, 11, 1-9.
Behan, J., Fitzpatrick, C., Sharry, J., Carr, A., & Waldron, B. (2001). Evaluation of the Parents Programme. The Irish Journal of Psychology, 22, 238-256.
Berkien, M., Louwerse, A., Verhulst, F., & van der Ende, J. (2012). Children's perceptions of dissimilarity in parenting styles are associated with internalizing and externalizing behaviour. European Child and Adolescent Psychiatry, 21, 79-85.
Bierman, K. L., Coie, J. D., Dodge, K. A., Greenberg, M. T., Lochman, J. E., & McMahon, R. J. (1996). Integrating social-skills training interventions with parent training and family-focused support to prevent conduct disorder in high-risk populations: The fast track multisite demonstration project. Understanding Aggressive Behaviour in Children, 113, 99-128.
Campbell, S. B. (1995). Behaviour problems in preschool children: A review of recent research. Journal of Child Psychology and Psychiatry, 36, 113-149.
Cataldi, E. F., Laird, J., & KewalRamani, A. (2009). High school dropout and completion rates in the United States: 2007 (NCES 2009-064). Washington, DC: National Centre for Education Statistics.
Clark, J. D., Parker, A. M., & Lynch K. G. (1999). Psychopathology and substance-related problems during early adolescence: A survival analysis. Journal of Clinical child Psychology, 28, 333-341.
Clefberg-Liberman, L., Altuzarra, M. P., Öst, L. G., & Ollendick, T. (2012). How I feel about things: Psychometric data from a sample of Spanish-speaking children. International Journal of Clinical and Health Psychology, 12, 419-433.
Coughlin, M., Sharry, J., Fitzpatrick, C., Guerin, S., & Drumm, M. (2009). A controlled evaluation of the Parents Plus Children's Programme: A video-based programme for parents of children aged 6-11 years with behavioural and developmental problems. Clinical Child Psychology and Psychiatry, 14, 541-558.
Cunningham, N. R., & Ollendick, T. H. (2010). Comorbidity of anxiety and conduct problems in children: Implications for clinical research and practice. Clinical Child and Family PsychologyReview, 13, 333-347.
DeCato Murphy, L., Donohue, B., Azrin, N., Teichner, G., & Crum T. (2003). Adolescents and their parents: A critical review of measures to assess their satisfaction with one another. Clinical Psychology Review, 23, 129-170.
Disney, E. R., Elkins, I. J., McGue, M., & Iacono, W. G. (1999). Effects of ADHD, conduct disorder, and gender on substance use and abuse in adolescence. American Journal of Psychiatry, 156, 1515-1521.
Dodge, K. A., Greenberg, M. T., & Malone, P. S. (2008). Testing an idealised dynamic cascade model of the development of serious violence in adolescence. Child Development, 79, 1907-1927.
Finzi-Dottan, R., Bilu, R., & Golubchik, P. (2011). Aggression and conduct disorder in 1 former Soviet Union immigrant adolescents: The role of parenting style and ego identity. Children and Youth Services Review, 33, 918-926.
Furlong, M., McGilloway, S., Bywater, T., Hutchings, J., Smith, S. M., & Donnelly, M. (2012). Behavioural and cognitive-behavioural group-based parenting programmes for early-onset conduct problems in children aged 3 to 12 years (Review). The Cochrane Collaboration 2, 1-357.
Goodman, A., & Goodman, R. (2011). Population mean scores predict child mental disorder rates: Validating SDQ prevalence estimators in Britain. Journal of Child Psychology and Psychiatry, 52, 100-108.
Goodman, R. (1997). The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38, 581-586.
Goodman, R. (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of American Academy of Child Adolescent Psychiatry, 40, 1337-1345.
Griffin, C., Guerin, S., Sharry, J., & Drumm, M. (2010). A multicentre controlled study of an early intervention parenting programme for young children with behavioural and developmental difficulties. International Journal of Clinical and Health Psychology, 10, 279-294.
Hahlweg, K., Heinrichs, N., Kuschel, A., Bertram, H., & Naumann, S. (2010). Longterm outcome of a randomized controlled universal prevention trial through a positive parenting program: Is it worth the effort? Child and Adolescent Psychiatry and Mental Health, 4, 1-14.
Halpenny, A. M., Nixon, E., & Watson, D. (2010). Children's perspectives on parenting styles and discipline: A developmental approach. Dublin: Office of the Minister for Children and Youth Affairs. Dublin: The Stationery Office.
Hand, A., Ní Raghallaigh, C., Cuppage , J., Coyle, S., & Sharry, J. (2012). A controlled clinical evaluation of the Parents Plus Children's Programme for parents of children aged 6-12 with mild intellectual disability in a school setting. Clinical Child Psychology and Psychiatry. doi:10.1177/1359104512460861.
Hartley, J. (2012). New ways of making academic articles easier to read. International Journal of Clinical and Health Psychology, 12, 143-160.
Haskett, M. E., Ahern, L. S., Ward, C. S., & Allaire, J. C. (2006). Factor structure and validity of the Parenting Stress Index/ Short Form. Journal of Clinical Child and Adolescent Psychology, 35, 302-312.
Hutchings, J., Bywater, T., Daley, D., Gardner, F., Whitaker, C., Jones, K., & Edwards, R. T. (2007). Parenting intervention in Sure Start services for children at risk of developing conduct disorder: Pragmatic randomised controlled trial. British Medical Journal, 334, 678-682.
Hutchings, J., Bywater, T., Williams, M. E., Shakespeare, M. K., & Whitaker, C. (2009). Evidence for the extended School Aged Incredible Years parent programme with parents of high-risk 8 to 16 year olds. Bangor: Bangor University.
Hutchings, J., & Webster-Stratton, C. (2004). Community-based support for parents. In M. Hoghughi, & N. Long (Eds.), Handbook of parenting: Theory and research for practice (pp. 334-351). London: Sage Publications.
Hutchings, J. M. (1996). Evaluating a behaviourally based parent training group: Outcomes for parents, children and health visitors. Behavioural and Cognitive Psychotherapy, 24, 150-171.
James, D. E., Schumm, W. R., Kennedy, C. E., Grigsby, C. C., Shectman, K. L., & Nichols, C. W. (1985). Characteristics of the Kansas Parental Satisfaction Scale among two samples of married parents. Psychological Reports, 57, 163-169.
Kiff, C. J., Lengua, L. J., & Zalewski, M. (2011). Nature and nurturing: Parenting in the context of child temperament. Clinical Child and Family Psychology Review, 14, 251-301.
Kilroy, S., Sharry, J., Flood, C., & Guerin, S. (2011). Parent training in the community: Linking process to outcome. Clinical Child Psychology and Psychiatry, 16, 459-473.
Mason, W. A., Kosterman, R., Hawkins, J. D., Haggerty, K. P., & Spoth, R. (2003). Reducing adolescents' growth in substance use and delinquency: Randomized trial effects of a preventive parent-training intervention. Prevention Science, 4, 203-213.
McCart, M. R., Priester, P., Davies, W. H., & Azen, R. (2006). Differential effectiveness of cognitive- behavioural therapy and behavioural parent-training for antisocial youth: A meta-analysis. Journal of Abnormal Child Psychology, 3, 527-543.
McGilloway, S., Ni Mahille, G., Bywater, T., Furlong, M., Lecky, Y., Kelly, P., Comiskey, C, & Donnelly, M. (2012). A parenting intervention for childhood behavioural problems: A randomized controlled trial in disadvantaged community-based settings. Journal of Consulting and Clinical Psychology, 80, 116-127.
Meltzer, H., Ford, T., Goodman, R., & Vostanis, P. (2011). The burden of caring for children with emotional or conduct disorders. International Journal of Family Medicine, 1-8.
Morris, A. S., Silk, J. S., Myers, S. S., & Robinson, L. R. (2007). The role of the family context in the development of emotion regulation. Social Development, 16, 361-388.
National Institute for Health and Clinical Excellence, NICE (2006). Parent-training/education programmes in the management of children with conduct disorders. Available from: http://www.nice.org.uk/nicemedia/live/11584/33426/33426.pdf [retrieved 3 Nov 3 2012].
Nixon, E. (2012). Growing up in Ireland: National Longitudinal Study of Children: How families matter for social and emotional outcomes of 9-year-old children. Dublin: Government Publications.
Piquero, A. R., Farrington, D. P., & Blumstein, A. (2003). The criminal career paradigm. In M. H. Tonry (Ed.), Crime and justice: A review of research (pp. 359-506). Chicago, IL: University of Chicago.
Quinn, M., Carr, A., Carroll, L., & O'Sullivan, D. (2007). Parents Plus Programme 1. Evaluation of its effectiveness for preschool children with developmental disabilities and behavioural problems. Journal of Applied Research in Intellectual Disabilities, 22, 345-359.
Raudino, A., Woodward, L. J., Fergusson, D. M., & Horwood, L. J. (2012). Childhood conduct problems are associated with increased partnership and parenting difficulties in adulthood. Journal of Abnormal Child Psychology, 40, 251-263.
Reitman, D., Currier, R. O., & Stickle, T. R. (2002). A critical evaluation of the Parenting Stress Index- Short Form (PSI-SF) in a head start population. Journal of Clinical Child and Adolescent Psychology, 31, 384-392.
Rogosch, F. A., Dackis, M. N., & Cicchetti, D. (2011). Child maltreatment and allostatic load: Consequences for physical and mental health in children from low-income families. Development and Psychopathology, 3, 1107-1124.
Rooke, O., Thompson, M., & Day, C. (2004). School-based open access parenting programmes: Factors relating to uptake. Child and Adolescent Mental Health, 9, 130-138.
Sandler, I. N., Schoenfelder, E. N., Wolchik, S. A., & MacKinnon, D. P. (2011). Long-term impact of prevention programs to promote effective parenting: Lasting effects but uncertain processes. Annual Review of Psychology, 62, 299-329.
Scott, S., & Dadds, M. R. (2009). Practitioner review: When parent training doesn't work: Theory-driven clinical strategies. Journal of Child Psychology and Psychiatry, 50, 1441-1450.
Serketich, W. J., & Dumas, J. E. (1996). The effectiveness of behavioural parent training to modify antisocial behaviour in children: A meta-analysis. Behaviour Therapy, 27, 171-186.
Sharry, J., & Fitzpatrick, C. (2007). Parents Plus Children's Programme: A video-based parenting guide to managing behaviour problems and promoting learning in children aged six to eleven. Dublin: Mater Hospital.
Sharry, J., Guerin, S., Griffin, C., & Drumm, M. (2005). An evaluation of the Parents Plus Early Years Programme: A video based early intervention for parent of pre-school children with behavioural and developmental disabilities. Clinical Child Psychology and Psychiatry, 10, 319-336.
Shonkoff, J. P., & Phillips, D. A. (2000). From neurons to neighbourhoods: The science of early childhood development. Washington, DC: National Academy Press.
Stormshak, E., Bierman, K., McMahon, R., & Lengua, L. (2000). Parenting practices and child disruptive behaviour problems in early elementary school. Journal of Clinical Child Psychology, 29, 17-29.
Taylor-Richardson, K. D., Heflinger, C. A., & Brown, T. N. (2006). Experience of strain among types of caregivers responsible for children with serious emotional and behavioural disorders. Journal of Emotional and Behavioural Disorders, 14, 157-168.
Webster-Stratton, C., Rinaldi, J., &. Reid, J. M. (2011). Long-term outcomes of Incredible Years Parenting Program: Predictors of adolescent adjustment. Child and Adolescent Mental Health, 16, 38-46.