Bowel obstruction secondary to an intramural haematoma is a rare complication and generally arises following abdominal trauma, anticoagulant therapy or haematological diseases.1 Endoscopic biopsy of the duodenum is a very rare cause of intramural haematoma, with only isolated cases published in the literature, mostly in children.2,3 In a series of almost 27,000 procedures conducted over a 12-year period, the incidence of this complication was 1/1922 procedures (2015).
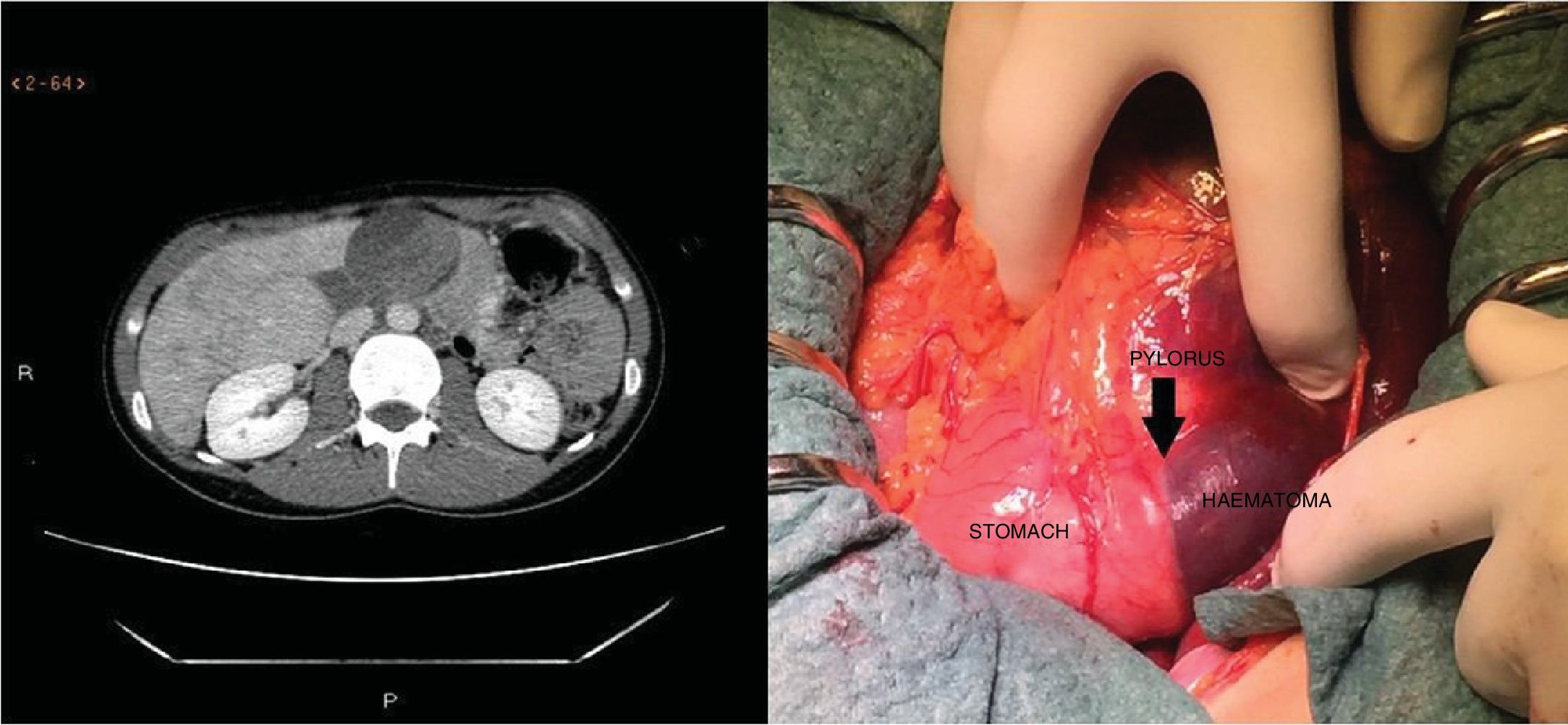
We present the case of a 27-year-old female patient with coeliac disease diagnosed in 2013 due to her family history, HLA-DQ2-positive, anti-tissue transglutaminase antibody levels of 30IU/ml and duodenal biopsies with mild villous atrophy (Marsh 3A). The patient was not following a strict gluten-free diet or undergoing clinical monitoring when she attended the clinic due to asthenia and intermittent diarrhoea, with a BMI of 19. The gastroscopy showed normal duodenal mucosa. Biopsies were obtained using standard forceps. The patient experienced no bleeding during the examination and was discharged asymptomatic. 12h after the examination, she experienced nausea, vomiting and epigastric pain. Upon re-examination, she was found to be afebrile with BP 108/60mmHg, HR 65bpm and abdomen painful upon palpation of the mesogastrium, but without signs of peritoneal irritation. The abdominal X-ray revealed no pneumoperitoneum; Blood test: leukocytes 10.8×103/μl, Hb 11.8g/dl, platelets 222×103/μl, prothrombin time 98%, APTT 29.1s, CRP 1.3mg/dl, GPT 19U/l, GGT 43U/l, AP 55U/l, total bilirubin 0.6mg/dl and amylasaemia 130U/l. Due to the persistent signs of obstruction and intense pain, despite nasogastric suction and analgesia, an abdominal CT scan was performed, which showed a large accumulation measuring 4×8×10cm, AP×LL×CC, in contact with the duodenum, with displacement to the left of the head of pancreas and superior mesenteric artery and vein. The content of the accumulation was heterogeneous, consistent with a duodenal haematoma. Because only a portal-phase CT scan was performed, active bleeding could not be ruled out due to its hyperdense content that could correspond to extravasation of the IV contrast. In light of the above, an exploratory laparotomy was performed.
The examination revealed a duodenal haematoma with involvement from the pylorus and which dissected the first portion of the duodenum and initial part of the second, with no evidence of transmural perforation. The haematoma was drained with evacuation of clots, leaving the gastrostomy tube in place. After the operation, total parenteral nutrition was started together with IV antibiotic therapy. The patient recovered without complications and was discharged 28 days after the procedure on an oral diet.
The histological study of the duodenal biopsies showed increased intraepithelial lymphocytes without villous atrophy (Marsh 1).
The coagulation study was normal (platelet count, prothrombin time and APTT); more targeted studies were not performed (Fig. 1).
Bowel obstruction secondary to duodenal haematoma is a very rare endoscopy-related complication, with only isolated cases published in the literature, mostly in healthy children.2,3 Endoscopic biopsies may entail a greater risk for patients with haematological disorders. Although there is very little information available,4 the indication for biopsy must be thoroughly justified in these patients.
Our patient did not exhibit any coagulation disorder that could have contributed to the development of a haematoma. Despite a normal platelet count, prothrombin time and APTT, this patient may nonetheless have been susceptible to a greater risk of bleeding secondary to platelet dysfunction or another coagulation disorder associated with the underlying disease. However, no platelet aggregation studies were performed or fibrinogen or D-dimer levels assessed that could be of use. The only procedure undertaken was the mucosal biopsies obtained with standard forceps. As such, the haematoma appears to have been caused solely by the vascular lesion arising from the trauma inflicted by the biopsy forceps, similar to other cases reported in the literature of children with no haematological disease or underlying coagulopathy that could have explained the onset of this complication. Although relative retroperitoneal fixation of the duodenum and a rich submucosal vascularisation are factors that could explain the increased susceptibility of children and adults of thin build, the BMI of our patient was normal. We do not know if biopsy after biopsy was taken, with lesion of a submucosal vessel, which could explain the development of the haematoma. However, Sahn et al.1 did not find any correlation between haematoma incidence, number of biopsies or histological findings and the histological review only showed an increase in intraepithelial lymphocytes (Marsh 1), with no evidence of vascular lacerations.
Its clinical manifestation consists of abdominal pain around the time of the procedure and, depending on the extension of the haematoma, vomiting due to duodenal obstruction. Jaundice and acute pancreatitis have also been reported in cases of papilla of Vater (major duodenal papilla) involvement by the haematoma.
Conservative treatment is the standard of care. Most patients with an intramural duodenal haematoma respond well to treatment with nasogastric suction, discontinuation of anticoagulation therapy and/or correction of coagulation if necessary, fluid and electrolyte replacement and/or parenteral nutrition, with gradual resolution of obstructive symptoms in a few days.1,3 However, surgery or endoscopy may be necessary in cases of complicated haematoma with compression of the bile duct together with jaundice or pancreatitis, signs of bleeding, infarction, peritonitis or persistent bowel obstruction treated with conservative therapy.2,5 In our patient, due to the rapid progression and severity of clinical symptoms, with abdominal pain and very intense vomiting 12h after the procedure, and the fact that persistent bleeding could not be ruled out due to the observation of hyperdense material inside the haematoma (only a portal phase CT was performed, with no arterial or venous phase CT to effectively classify the bleeding), surgery was conducted.
In conclusion, intramural duodenal haematoma is a potential complication of endoscopic biopsy that endoscopists should be aware of and recognise in order to ensure early diagnosis and appropriate management.
Please cite this article as: Mego M, Lugo N, Roura J, Saperas E. Obstrucción duodenal por hematoma intramural como complicación de la biopsia endoscópica. Gastroenterol Hepatol. 2019;42:381;382.