Obsessive-compulsive disorder (OCD) is a chronic psychiatric illness with a lifetime prevalence of 1–3%.1 A complex interaction between genetic and environmental factors has been implicated in the etiopathogenesis of OCD.2 Obsessive-compulsive symptoms can also be associated with various neurological illnesses, including mass lesions or infarcts, particularly in the striatum, frontal or temporal lobes, infection, closed head injury or neurodegenerative disorders.3,4
Dysembryoplastic neuroepithelial tumours (DNET) are uncommon, benign, mixed neuronal-glial tumours which usually present with seizures, headache or focal neurological deficits.5 We report a rare clinical association of DNET with obsessive-compulsive symptoms in a 37-year-old lady, which improved after surgical resection.
Case reportMrs A, a 37-year-old married lady, presented to the psychiatry outpatient department with two months history of repetitive, intrusive blasphemous thoughts, pathological doubts, and intrusive mental images of wild animals and snakes, which used to cause her a lot of distress. It was associated with compulsive checking, reassurance seeking and cognitive compulsions by substituting distressing images. Since early childhood, she had high myopia and was diagnosed with hypothyroidism two years prior. Family history is significant for major depression in her mother. Mental status examination revealed ego-dystonic blasphemous thoughts, intrusive imagery, compulsive checking, ideas of helplessness, and anxious affect. She was diagnosed with OCD with mixed obsessional thoughts and acts as per the International Classification of Diseases, 10th edition. The patient was started on 5 mg of Escitalopram, which was planned to increase to 20 mg daily gradually and 0.5 mg of Clonazepam. An endocrinology consultation was sought for hypothyroidism, and she was advised to continue 50 mg of Thyroxine.
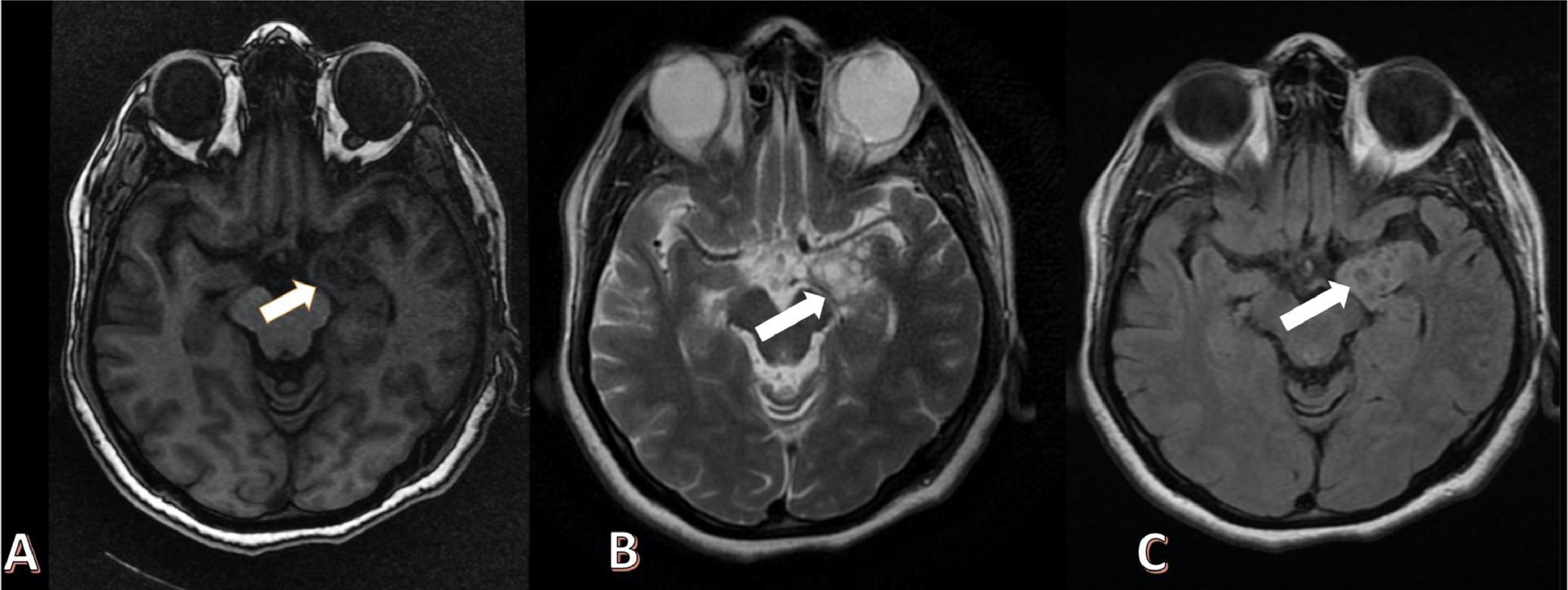
A week later, the patient presented to the emergency department with complaints of sudden onset of slurring speech, headache, difficulty walking, tremors of both upper and lower limbs, confusion, disorientation, and visual hallucinations. Electroencephalogram was suggestive of mild encephalopathy. Magnetic Resonance Imaging (MRI) of the brain revealed a well-defined, intra-axial lesion measuring 2.8 × 3.1 × 4.2 cm involving the left hippocampus. The lesion was heterogeneously hypointense on T1 weighted images and heterogeneously hyperintense on T2 images with a characteristic “bubbly appearance”, with no blooming, no restriction on diffusion sequences and showing rim enhancement (Fig. 1 A-C). The patient was then referred to Neurosurgery. Left anterior temporal lobectomy and hippocampectomy with complete lesion removal was performed. Histopathological examination showed features suggestive of DNET. A month later, the patient reported significant improvement in intrusive imagery, blasphemous thoughts, pathological doubts, compulsive behavior and the associated distress. The scores on the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) before and after the surgery were 22 and 10, respectively. She had repetitive doubts about her health status with mild distress, so 5 mg of Escitalopram was continued. Six months after the surgery, she had persistent anxiety about her health, and there was a significant improvement in other obsessive-compulsive symptoms. A neuropsychological assessment revealed deficits in sustained attention, verbal fluency, and verbal episodic memory. Escitalopram was increased to 15 mg per day, and applied relaxation techniques and home-based cognitive rehabilitation strategies were taught to the patient. There has been significant improvement in her functioning.
DiscussionOur report illustrates the association between obsessive-compulsive symptoms and left temporal DNET and the psychiatric outcome after surgical resection. Many structural and functional neuroimaging studies have demonstrated alterations in the cortico-striato-thalamo-cortical (CSTC) circuits implicated in cognitive, behavioral and motivational processes in OCD.6 With its afferent and efferent connections with the orbitofrontal cortex, medial prefrontal cortex and ventral striatum, the temporal lobe forms an integral part of neuroanatomical correlates of OCD.6 Temporal lobe atrophy has been implicated in the compulsive behaviors observed in frontotemporal dementia.7 Similarly, temporal lobe epilepsy is another condition associated with obsessive-compulsive symptoms.8 Owing to the high prevalence of refractory epilepsy in patients with temporal lobe DNET, inter-ictal psychiatric disorders are common in these patients.9 There have been reports of DNET presenting with atypical features like major depressive and schizophreniform features.9,10 Our case highlights a novel association between temporal lobe DNET and OCD.
Ethical considerationsWritten informed consent was taken from the patient for publishing this report.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
None.