Urinary tract infection is a rare condition in young men with no predisposing factors. In contrast, sexually transmitted infections (STI) are becoming more common and, with many having an acute onset (haematuria, dysuria, haemospermia, testicular inflammation and/or epididymitis, etc), these patients often seek help from emergency departments. Various studies suggest that STI play a central role in the origin of sterile pyuria in young men1,2, and our aim in this study was to find out if this was true in our environment.
From May 2014 to July 2017, we looked for microorganisms related to STI in samples sent from the Accident and Emergency department (A&E) from men aged 15–59 with sterile pyuria of unknown cause. We used urine samples with >14 leukocytes/μl (Sysmex UF-1000i analyser) which had been sent for urine culture and been negative, and the detection of STI-causative pathogens was performed by PCR (STI-7, Seegene, Seoul, South Korea). In cases with severe pyuria, the urine was also spread on chocolate agar (to rule out gonococcus and other bacteria which do not grow in the media usually used for urine culture) and in others, studies were carried out for herpes simplex (LightMix®, Roche, Berlin, Germany) and adenovirus (in-house PCR).
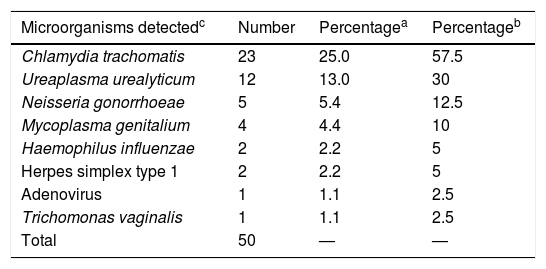
We studied the urine of 92 patients with 15 to 6123 leukocytes/μl (median: 76). Previously undiagnosed infections were detected in 40 patients (43%) aged from 17 to 59 (median: 32), with a total of 50 genitourinary infection-causing microorganisms, chief amongst which was Chlamydia trachomatis (n=23), representing 57.5% of positive cases (Table 1). No urethral exudate samples were collected from any of the patients in A&E. The results were reported to the patients and/or the doctors they had been referred to. Of the 40 patients, 38 were contacted and 28 (70%) attended the microbiology clinic (it was not possible to inform two patients, both with Ureaplasma urealyticum infection). New urine samples (first-void urine) were obtained from 27 patients and 22 (79%) had leucocyturia. A urethral swab was obtained from 25 patients, with leukocytes being found in 15 (60%).
Microorganisms detected in 92 males aged 15 to 59 with sterile pyuria.
| Microorganisms detectedc | Number | Percentagea | Percentageb |
|---|---|---|---|
| Chlamydia trachomatis | 23 | 25.0 | 57.5 |
| Ureaplasma urealyticum | 12 | 13.0 | 30 |
| Neisseria gonorrhoeae | 5 | 5.4 | 12.5 |
| Mycoplasma genitalium | 4 | 4.4 | 10 |
| Haemophilus influenzae | 2 | 2.2 | 5 |
| Herpes simplex type 1 | 2 | 2.2 | 5 |
| Adenovirus | 1 | 1.1 | 2.5 |
| Trichomonas vaginalis | 1 | 1.1 | 2.5 |
| Total | 50 | — | — |
Epididymo-orchitis was diagnosed in 22/40 patients (55%). Testicular involvement was detected in 15 of 23 patients infected by C. trachomatis and one of the five with gonorrhoea. In two patients (aged 42 and 44), Haemophilus influenzae was isolated after spreading their urine samples on chocolate agar (both had been appropriately treated with ciprofloxacin). In the remaining 18/40 patients (45%) the final diagnosis was urethritis (Chlamydia trachomatis was involved in eight and gonococcal infection in four). Three of the cases of urethritis were associated with additional clinical conditions: balanopreputial lesions due to herpes simplex type 1; conjunctivitis due to adenovirus; and simultaneous oral and genital primary herpes simplex type 1 infection. A pharyngeal swab was taken from 20 patients, with four (20%) positives (Neisseria gonorrhoeae [n=2], U. urealyticum [n=1] and adenovirus [n=1]). An anal swab was taken from two patients, with N. gonorrhoeae detected in one, and a conjunctival swab was taken from one patient, detecting adenovirus.
As a result of the expanded analysis, changes to treatment were made in 35 patients (88%): 30 patients had an antibiotic replaced, added or withdrawn due to inadequate empirical treatment, and another five not previously treated were prescribed an antibiotic. Ciprofloxacin was the antibiotic most inappropriately prescribed (22 occasions).
In conclusion, the urine collected for urine culture from males aged 15–59 with sterile pyuria treated in Accident and Emergency was very useful for the diagnosis of other previously unsuspected infections, with a yield of 43%. C. trachomatis was the most common pathogen (25% of the urine samples studied and 57.5% of those positive). The definitive diagnosis required changes in the treatment of most of the patients with positive results (88%). It is important to remember how uncommon cystitis in young men is without underlying disease and to suspect an STI for the choice of treatment, even if no urethral discharge is observed and prior unprotected sexual relations cannot be confirmed. The microbiological diagnosis provides confirmation of the pathogen and allows changes to be made to the empirical treatment, if necessary, and subsequent and necessary study of sexual contacts. The application of protocols for the empirical treatment of epididymo-orchitis in young patients, covering C. trachomatis and gonococcus3, improves therapeutic success.
FundingThis study did not receive funding of any type.
Please cite this article as: Idigoras P, de la Caba I, Grandioso D, Gomariz M. Recuperación de Chlamydia trachomatis y otros patógenos en la orina de varones con piuria estéril atendidos en urgencias. Enferm Infecc Microbiol Clin. 2020;38:507–508.