Gastric antral vascular ectasia (GAVE) is a rare cause of upper gastrointestinal bleeding. It causes approximately 4% of upper gastrointestinal bleeding not associated with esophageal varices,1–5 predominantly in women aged 60–70 years.1–3
It can present as hidden bleeding associated with iron-deficiency anemia or, more rarely, as acute bleeding.1,2,5,6 Some 60%-70% of patients require periodic blood transfusions despite chronic iron supplementation.3 The etiology is uncertain, although it is closely related to systemic diseases, such as cirrhosis of the liver (up to 30%).1–5,7
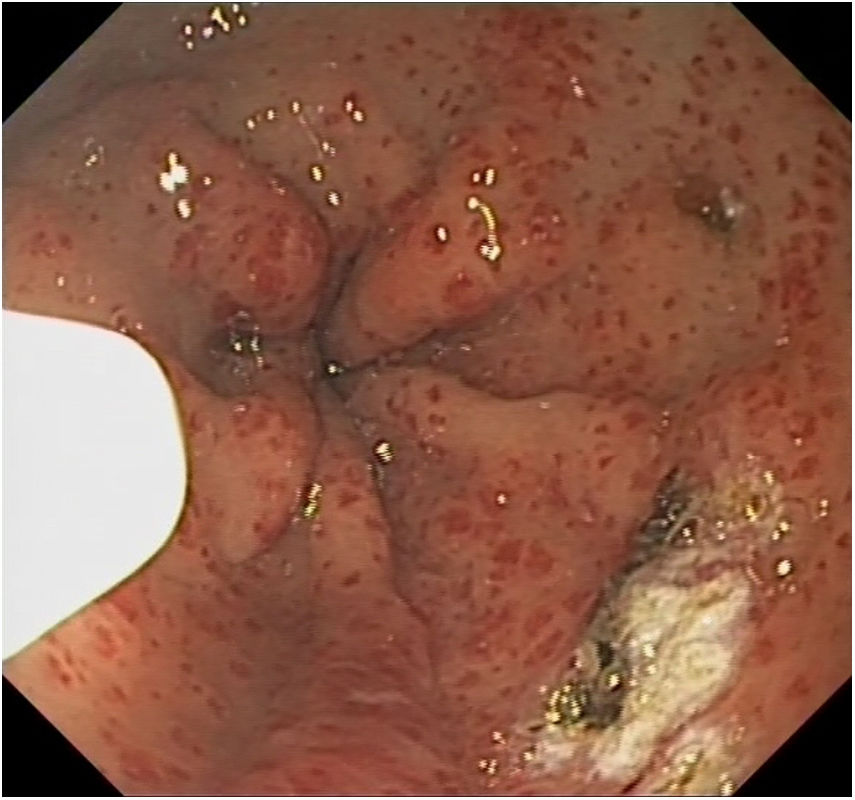
The diagnosis is made based on characteristic endoscopic findings, showing 2 well-differentiated GAVE patterns: diffuse stippling, or ‘honeycomb stomach’; and linear dots, or ‘watermelon stomach’.1,4,6,7
It is important to make a correct differential diagnosis with portal hypertensive gastropathy and chronic antral gastritis because their management is very different.7 Portal hypertensive gastropathy usually affects the fundus and the gastric body. It is more frequent in men with liver cirrhosis, and its treatment (unlike GAVE) is effective with measures that reduce portal pressure.1,2,5,7 A pathology study is important in these cases because, while not pathognomonic, characteristic findings of GAVE include: vascular ectasia of the capillaries, intraluminal hyaline thrombi and spindle cell proliferation, without signs of inflammation.1,3,7
Symptomatic treatment consists of fluid resuscitation and blood transfusions to correct blood loss, either acute or chronic, in addition to appropriate iron supplementation.1,5 There is not sufficient scientific evidence about medical treatment with estrogen/progestogen, tranexamic acid, thalidomide, or octreotide, so these are only recommended if endoscopic treatment has failed to control blood loss.1–3,5–7
The gold-standard treatment options for this disease include endoscopic ablation with YAG laser or argon-plasma coagulation. The latter provides the best benefit–cost ratio and lowest complication rate, although multiple sessions are necessary to reduce bleeding and reliance on transfusions for continued blood loss.1,2,5–7 Other endoscopic treatments, such as band ligation, have been proposed in recent years, but more studies are needed before providing a definitive conclusion regarding their use.2,4
Surgery is an uncommon therapeutic option. Antrectomy should be reserved for refractory cases4 that, despite medical and endoscopic treatment, present recurrent bleeding and severe anemia.6 Given the higher morbidity and mortality rates of these patients,1–3,5,7 surgery is the only curative treatment.3
Liver transplantation should be considered in cases of associated liver cirrhosis if the patient is a candidate.
We report the case of a 67-year-old woman with a history of poorly controlled type 2 diabetes, high blood pressure and long-term iron-deficiency anemia treated with high doses of oral iron, who required hospitalization for dyspnea on minimal exertion associated with severe anemia (Hb 7.7 mg/dL). For this reason, lower gastrointestinal endoscopy was conducted, during which colon polyps were observed. Findings from the upper gastrointestinal endoscopy were consistent with chronic antral gastritis.
After diagnosis, significant anemia persisted despite therapy, so outpatient treatment was initiated with intravenous iron, in addition to requiring multiple blood transfusions. For this reason, and due to suspected gastrointestinal blood loss, the study was completed with capsule endoscopy, which revealed GAVE and showed signs of recent bleeding. The diagnosis of ‘watermelon stomach’ GAVE was confirmed by upper gastrointestinal endoscopy (Fig. 1), and endoscopic treatment was initiated with argon-plasma coagulation for 6 sessions.
Despite the endoscopic treatment and the association of octreotide, as well as an experimental treatment in a hyperbaric chamber, the need for transfusion continued to be high (3–4 units of packed red blood cells per week), and the patient remained highly symptomatic.
As the condition was refractory to treatment, a surgical approach assisted by intraoperative endoscopy was proposed to obtain the most effective resection possible, performing antrectomy with laparoscopic Roux-en-Y reconstruction.
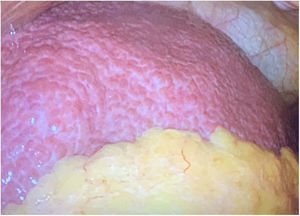
During surgery, we observed a previously unknown micronodular cirrhotic liver (Fig. 2), despite having carried out a preoperative study using thoracoabdominal CT scan, serologies, autoimmunity, tumor markers, laboratory analyses with liver function tests, respiratory function tests and transthoracic echocardiogram, all of which were normal.
The postoperative period progressed favorably, except for poor glycemic control, and the patient was discharged on the eighth day.
In the follow-up visits after 1, 3 and 6 months, the absence of GAVE was confirmed by endoscopy and anemia testing. In addition, the chronic liver disease study was completed, which provided the diagnosis of Child-Pugh stage A liver cirrhosis, probably caused by steatosis.
The pathological study of the surgical specimen reported the presence of focal ulceration of the mucosa and vascular congestion with fibrin thrombi in the lamina propria in the absence of inflammation, all of which were compatible with GAVE.
Our case highlights the importance of a good differential diagnosis with portal hypertensive gastropathy and chronic antral gastritis due to their different management, the frequent association of this disease with liver cirrhosis and the need for surgical treatment in cases that are refractory to endoscopic and pharmacological treatment, since, despite there being no cases reported in the literature, this is the only curative treatment.
Please cite this article as: Pérez Martín B, Rodríguez Martínez E, Baamonde de la Torre I, Suárez Pazos N, Díaz Tie M. Ectasia vascular gástrica antral refractaria a tratamiento endoscópico. Cir Esp. 2020;98:416–418.