In December 2019, the first cases of pneumonia of unknown origin were reported in the city of Wuhan (People’s Republic of China).1 The pathogen was identified as a new beta-coronavirus, called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The infection caused by this virus is known as COVID-19 (coronavirus disease 2019). On March 11, 2020, the World Health Organization officially declared the pandemic situation. As of today, there have been more than 2.8 million cases of COVID-19 reported by 185 countries around the world. Spain is one of the most affected countries in terms of absolute number of cases and number of deaths.
Although the potential for transmission of COVID-19 through transplantation is unknown, as early as January 2020 the Spanish healthcare system issued recommendations for the evaluation and selection of organ donors regarding SARS-CoV-22 infection.2 Donation in confirmed COVID-19 cases must be ruled out. In cured patients, individualized and cautious evaluation is recommended, and this should be done a minimum of 21 days after testing negative. As for donors at epidemiological risk (exposure to a confirmed case of COVID-19 or travel/residence in affected areas in the previous 21 days), if the potential donor presents clinical symptoms compatible with COVID-19, donation is rejected even without screening. If the potential donor does not present compatible symptoms, screening for SARS-CoV-2 is performed and donation is not considered if the result is positive. Screening is also mandatory if there is no epidemiological risk but clinical symptoms are compatible, or if lung or intestinal donation is considered. Although the incubation period for COVID-19 is 2–14 days, the recommended safety period in Spain of 21 days is to rule out possible outliers.2 Screening of potential donors must be done by RT-PCR on a sample obtained in the 24 h prior to extraction.2 Said sample can be obtained from the upper or lower respiratory tract, although the latter is preferable due to its greater diagnostic performance, and this sample is required in cases of lung or intestinal donation.
So far, 363 cases of COVID-19 have been reported to the National Transplant Organization in organ transplant patients (227 kidney recipients, 73 liver, 36 cardiac, 21 pulmonary, 5 pancreatic, and one multi-organ). Most have acquired the infection in the community after a median of 56 months post-transplantation. Only 62 cases (14%) of nosocomial infection have been reported. Within the latter, and applying the aforementioned policy, none of the patients had suspected infection derived from the donor.
There is little information on the prognostic factors and the evolutionary course of COVID-19 in transplant patients. Given how the endemic coronavirus infection behaves in immunosuppressed patients,3 a higher complication rate is expected,4–6 which has been confirmed in limited case series.7 It is also predictable that the period of viral excretion is longer than in non-transplant recipients, with the risk of ‘superspreading’ the virus, particularly among healthcare professionals.8,9 For this reason, in Spain, screening for SARS-CoV-2 is recommended in the potential recipient prior to transplantation, and the patient is temporarily excluded from the waiting list if the result is positive.2
The greatest problem caused by the COVID-19 epidemic in organ donation and transplantation has been the consequent saturation of the healthcare system and intensive care units. Hospitals have had to expand the capacity of their critical care units, new hospitals have been created to serve seriously ill patients with COVID-19, and hotels have been medicalized to care for non-seriously ill patients requiring isolation. Despite this, medical professionals have had to make complex decisions when allocating critical resources that were insufficient for the population demand during the exponential increase in the number of infections.10
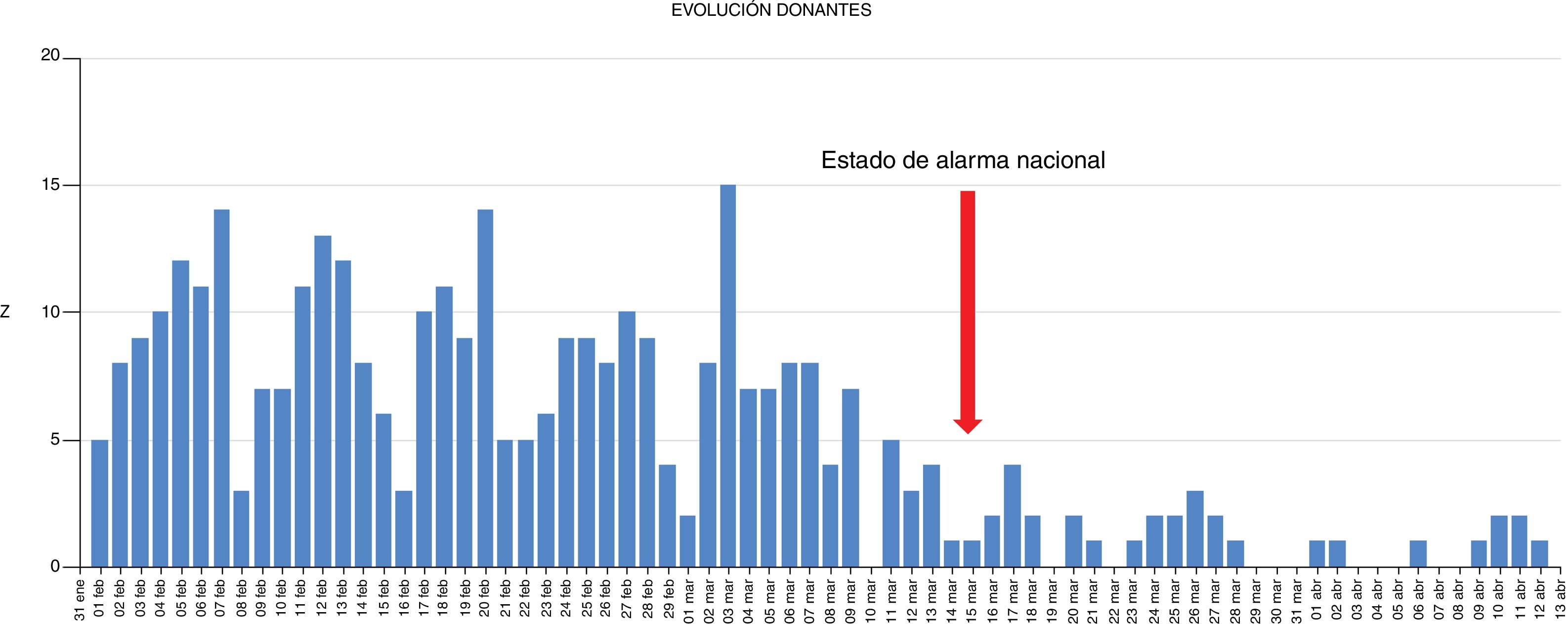
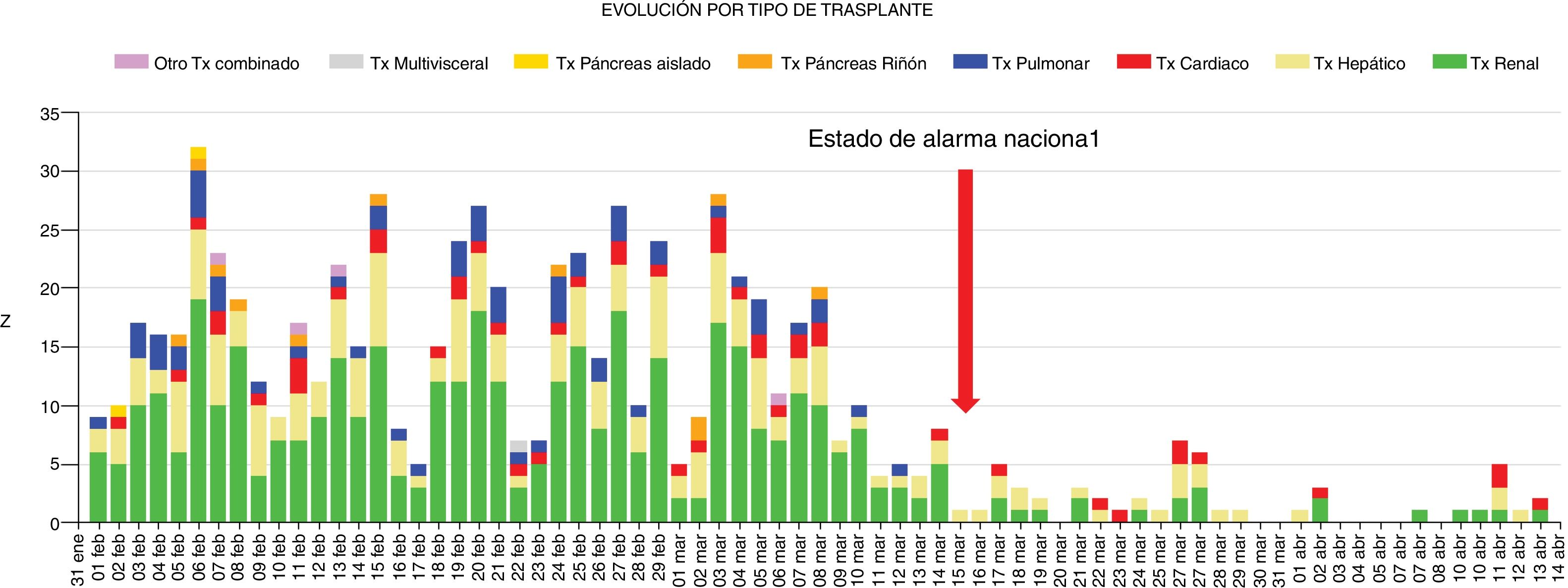
In this context, conducting organ donation and transplantation activities has been extraordinarily complex due to the saturated system and the lack of COVID-19-free areas in hospitals in order to guarantee patient safety after transplantation. Hospitals in highly affected areas have been instructed to make individualized assessments, case by case, of whether to proceed with each donation and transplant process, taking into account the patient’s clinical situation and the circumstances of the hospital.2 In the worst moments, only ideal donors were considered, and transplantation was only performed in patients in emergency situations or those presenting extreme clinical severity, or those who were difficult to transplant. All this has led to a drastic decrease in activity. On March 13, 2020, the national ‘State of Alarm’ status was declared in Spain. Until that date, the mean transplant activity in our country was maintained at 7.2 donors/day and 16.1 transplants/day. After that point, the numbers dropped to 1.1 and 2, respectively (Figs. 1 and 2). Although it is early to evaluate the impact of this reduced transplant activity, it is presumable that, under normal circumstances, the deaths of patients who were on the waiting list could have been avoided — patients who were also direct victims of this terrible pandemic.
We would like to acknowledge medical professionals for their tireless work during the COVID-19 epidemic.
Please cite this article as: Domı´nguez-Gil B, Coll E, Ferrer-Fàbrega J, Briceño J, Ríos A. Drástico impacto de la epidemia de COVID-19 sobre la actividad de donación y trasplante en España. Cir Esp. 2020;98:412–414.