Evidence-based surgery is a tool that has been adopted worldwide by surgeons. As all decisions must be current and have a scientific basis, the approach for performing it must be standardised.
Five important steps are required to perform surgery based on evidence. Convert the need for information into a question that can be answered, finding the best information to answer that question, critical evaluation of the evidence, and its validity, impact and applicability, integrating the evidence with your own experience, and with the evaluation of the patients. This should take into account their biology, values and specific circumstances, as well as to evaluate the effectiveness and efficiency of the execution of steps 1–4 and propose how to improve them.
ConclusionThis article presents the main tools to perform surgery properly based on evidence.
La cirugía basada en la evidencia es una herramienta que ha sido adoptada en todo el mundo por los cirujanos, ya que todas nuestras decisiones deben ser actualizadas, y tener un sustento científico; sin embargo, tenemos que aprender a sistematizar el abordaje para realizarla.
Para llevar a cabo la cirugía basada en la evidencia, se requieren 5 pasos importantes que son: convertir la necesidad de información en una pregunta que pueda responderse; buscar la mejor información con la cual responder esa pregunta; evaluación crítica de esa evidencia y de su validez, impacto y aplicabilidad; integrar la evidencia con la propia experiencia y con la evaluación clínica de nuestros pacientes, en su biología, valores y circunstancias específicas, y evaluar la efectividad y eficiencia de la ejecución de los pasos 1 al 4 y proponer cómo mejorarlos.
ConclusiónEste artículo comparte las herramientas principales para realizar de manera correcta una cirugía basada en la evidencia.
Evidence-based medicine is a movement which, pursuant to Manterola1 was begun by Sackett and Guyatt at McMaster University in 1990. They declared themselves the heirs of observational medicine, which was led by Pierre Louis in the nineteenth century, who was the first to apply a numerical method to compare the results of patients between 2 groups with no differences, which is currently considered the first trial.1,2 Sackett defined evidence-based medicine in 1996 as the “the conscientious, explicit and judicious use of current best evidence in making decisions about the care of the individual patient”.3 The definition has been modified since its adoption, and currently stands as “integrating the best available evidence of research with clinical experience and the patient's values”.4 It has been adopted by multiple specialisms and medical groups, and we are witnessing a transition to where it is now an important element in the decision-making process, not only in clinical practices but also in other related areas such as legal, administrative, research and editorial. Also, it helps to integrate in a simple way a series of convergent disciplines such as epidemiology, biostatistics, critical analysis of biomedical literature, the study of clinical research designs, social sciences applied to health, administration and health management.1
Although this tool is very useful and generates a clinical practice with good reason, it has not been as widely accepted in surgery as in general medicine, internal medicine and its subspecialisms. Surgeons usually oppose evidence-based medicine in surgical practice, and for many reasons.5 There is a general belief that surgeons prefer simple and quick responses to problems, and evidence-based medicine may be considered exactly the opposite. According to Sevdalis and McCulloch, it was McGreevy and Wiebe in an article entitled “A preliminary study of surgical personality”6 who explained that surgeons have personality features with a tendency to action instead of contemplation, intuition instead of calculation and, without a doubt, evidence-based medicine requires taking time, analysing and being critical. The use of evidence-based medicine in surgery or evidence-based surgery is a term that has already been coined, integrated to general surgery and surgical specialisms, and must be part of our daily work, since it helps us make decisions integrated with evidenced scientific grounds, which is highly valuable, especially as our performance is always more exposed, not only to the communication media and social networks, but also legal medicine.7
The goal of this work is to share the knowledge and basic steps to develop it.
The 5 basic components of evidence-based surgeryTo carry out evidence-based surgery, there are 5 important steps: (1) Converting the need for information into a question that can be answered. (2) Searching for the best information to answer that question. (3) Making a critical assessment of that evidence and its validity, impact and applicability. (4) Integrating evidence with experience and the clinical assessment of our patients, their biology, values and specific circumstances. (5) Evaluating the effectiveness and efficiency of the execution of steps 1–4, and proposing how to improve them.
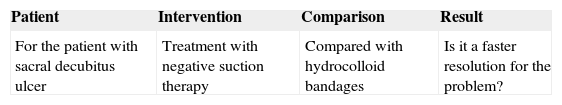
Converting the need for information into a question that can be answeredThe first step is knowing exactly what we are looking for. If we cannot convert our doubt into a question that can be answered, we can hardly find the answer. The research question may be within one of these 4 main areas: diagnosis, risk, prognosis or treatment.8 We must generate keywords for this question to make the search for internet databases easier.9 There is a strategy to define the problem and turn it into an initial question. It is called PICO strategy; the initials of the word make reference to: problem of the patient (defines the population of interest), intervention considered (what are the interventions to be considered as alternatives?), comparison with the standard intervention (which is the treatment we are considering, as usual or standard?) and outcome in English, or results (what are the results we are interested in?).10 For instance, if we were ready to treat a patient with sacral decubitus ulcer with hydrocolloid, but we would like to consider solving it faster with negative suction therapy, we could ask the question in Table 1.
This way we manage to have a question with which we can begin our search through the various internet databases.
Search for the best informationUnfortunately the concept of “search for information on books to be updated” is increasingly obsolete. Any current surgical treatment book is as updated as its more recent reference and, at least, most are already outdated before being published, or recommend 5 to 6-year treatments after efficacy has been proved. Also, they would technically have to be systematic reviews. However, most books are opinions of experts (the lowest of evidences in hierarchy scales), and therefore we would have to turn to scientific magazines.4,11 The times when we would go to a library to search in “index medicus” catalogues and sat to write references with pen and paper, and then search in printed magazines, is over. Technology must be considered an ally, and today more than ever we have access to the whole world. We have to know which are the most practical, reliable and useful sources of information to answer the question. Today there is a huge amount of information to filter and evaluate on the Internet, so much that it is hard to chose.12 If we add the fact that many surgeons are still not familiar with technology, this is a major problem. Surgeons should feel as confident with a scalpel as with a digital tablet to access relevant and critical information.7 And if we do not, someone else will. Currently many patients attend the doctor's surgery with a certain degree of information (erroneous or correct, but lacking criteria) regarding their condition and treatment options. Thus, our decisions are questioned based on the information they have obtained, and we cannot simply turn our backs on them or ignore them.
The search for the best information requires a proper question that can be answered and, later, it requires conducting an efficient search on the internet, knowing with precision how to handle keywords and Boolean operators (AND, NOT, AND NOT, OR)13 and identify the best databases were we can obtain reliable information, and not simply internet blog sites. Some of the main databases where we can obtain reliable scientific information: Google Scholar, PubMed and OVID. Another of the best ones is Cochrane Database of Systematic Reviews. This is the result of a collaborative effort to which only systematic reviews and meta-analysis of the currently best evidence available are provided on the various subjects and specialisms, which provides us the most select and best quality information. Although we will not always obtain information on very specific subjects, it is also worth reviewing it.14
Without a doubt, the best studies are those which let us obtain truthful information with conclusions that not only have a well-established basis but are also applicable to our patients and the socio-economic environment. Systematic reviews and meta-analysis are conclusions generally derived from randomised clinical trials, which are currently the ones with the most methodological weight, and the ones we should prefer as compared to studies derived from the experience of only one surgeon or description of cases.
There is another criterion on selecting the best works. It is a trend that has been widely accepted by the most respected international magazines, which consists in systematising the preparation, development and content of scientific works through guidelines, in such a way that the same language is used consistently and the information transmitted is transparent, and that there are no omissions, misinterpretations or errors. This has been achieved through the publication and follow-up of guidelines to unify the report of different kinds of studies, such as CONSORT for randomised clinical trials, PRISMA for systematic reviews and meta-analysis, STROBE for observational studies and others.15–17 To consult them fully, we suggest visiting the EQUATOR site, which is a compilation of current guidelines (http://www.equator-network.org). When we opt for works following these guidelines, it is clear that the report of the study development, which decreases bias, and validity are easily identified, which makes it even simpler to obtain the relevant information to answer our question.
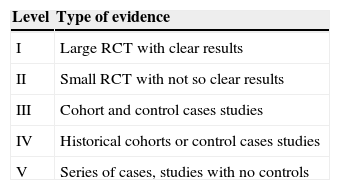
Critical evaluation of validity, impact and applicabilityOnce the articles have been obtained, we need to know how to differentiate those with proper methodological weight to take the responsibility of varying our treatment and take it as a basis. To help us choose, there is what we call a hierarchy or levels of evidence, which provide a frame to classify information on health interventions and indicate which studies shall be given more importance when they answer the same question using different kinds of designs.18,19 These levels of evidence have been modified on many occasions, but there is currently no universal consensus. Classifications of evidence according to SIGN, NICE, OCEBM, USPSTF and CTFPHC are mentioned in many publications3 and only talk about a lack of consensus to unify a hierarchy that is not unique. The simplest hierarchisation is found in Sackett's levels of evidence10 (Table 2).
However, this does not include all the special characteristics of the questions that must be answered in each specialism. Most surgical associations accept a scale of levels of evidence derived from the original by Sackett, but modified. In 2009, Oñate and Ochoa in Mexico proposed8 the GRADE system for the classification of evidence, which not only includes the level of evidence but also the strength of recommendation. In Colorado in 2010, a consensus was reached among leading plastic surgeons, dermatologists, otorhinolaryngologists and ophthalmologists, as well as editors of various related magazines, and it was agreed to assign levels of evidence to publications based on the question that needs to be solved.20 That is to say, if a diagnosis, therapeutic or prognosis/risk study is involved, the type of design varies based on the question that needs to be answered, and so also the levels of hierarchies.19 There are two aspects that almost all scales of evidence have in common. The first is that which assigns a higher evidence value to studies with the best possible design, generally, though not always, randomised clinical trials. Examples of this exception in plastic surgery are the following: for a diagnosis question, the best would generally be a multicentre cohort study validating a gold-standard pattern test or systematic reviews of this kind of studies. In the case of prognosis/risk it will be a multicentre prospective study with proper power or prospective cohort systematic reviews. And in the case of treatment, randomised clinical trials with proper quality or systematic reviews of randomised clinical trials of the same quality.19 And the second aspect in common is that almost all take expert opinions and clinical case reports as the lowest level in the hierarchy. This does not mean that the opinion of experts or clinical cases’ reports are not useful, but, as for the evidence they provide, they are deficient, and therefore those with the lowest weight. Even more, in evidence-based surgery, obtaining an excellent article of a proper randomised clinical trial will not be enough16; the results of this study have to be confronted with the reality of the patient and the hospital system the patient will attend.
Integrating the clinical assessmentObtaining information will not always provide us the exact results of the question we are trying to answer, or the results will not always be the most useful and applicable. The experience of the surgeon is key, and one of the pillars of evidence-based surgery. This judgement is always required, for instance in the teaching of trainee surgeons, and makes a difference between carrying out a world-renowned surgery and a different one that will specifically work in our patient. However, all surgical decisions will sooner or later have to evolve and be modified or changed based on scientific and technological advances. Surgery in any of its branches is no exception. And although having an experienced surgeon is good, it is best to have an experienced surgeon who grows with the help of evidence-based surgery. It is not only desirable, but it should be an ethical obligation.7 It is a known and studied problem that most surgeons believe they are up to date and even consider ourselves opinion leaders in their field. It is a critical and delicate point, since we would be surprised to evaluate how many of our decisions are indicated by custom or teaching, but actually have very little evidence of the need or success of their use.21 Another example is the risk of trying to blindly impose a clinical practice guideline without the judgement of the surgeon, which is equivalent to imposing a cooking recipe regardless of the availability of ingredients and the taste of the guest, which reduces the autonomy of the surgeon and the patient's individuality. The evidence cannot by itself answer clinical questions on patients specifically: the surgeon's judgement and experience are necessary.22,23 But a surgeon without up-to-date knowledge and the framework provided by evidence-based surgery is also like the blind leading the blind. Both evidence-based surgery and experience must mutually guide one another.
We also sometimes disregard the patient's values, which have increased their importance in the subsequent definitions of evidence-based medicine. There is a mismatch between what the patient needs and what the doctors perceive as relevant,24 mainly in the field of research, but also in clinical assistance. There has to be a consensus between what the patient wants and what the surgeon knows the patient needs. There are situations when religious, economic or social beliefs do not go hand in hand with the procedures to be carried out and we are “forced” to respect the patient's decision, changing what we consider the best option. It is here that evidence-based surgery helps us, providing options that may work as well as our first option. Taking our patient into consideration in the treatments to be performed is of vital importance, especially from the legal standpoint. The patient becomes increasingly involved in the decision-making process, and directing the patient towards the election of the treatment the patient needs, among effective options, will give us the benefit of making the patient co-responsible for the results; this is the basis of informed consent.7,12,25 However, an informed surgeon may guide the patient through different treatment options which have also proved to be useful.
Evaluating effectivenessThis last process is a review, a recap of what has already been done. The surgeon has to make a personal critical judgement and evaluate errors and choices made during the process of evidence-based surgery. From selecting the question and its formulation, to the Internet search using appropriate keywords. Later, the surgeon will evaluate the problems faced in the selection of the huge amount of information in the search engine and in obtaining the necessary and relevant articles.26 The surgeon will also review what are the challenges faced by choosing among those systematic reviews, meta-analysis or randomised clinical trials, or the best evidence available, and also how that surgeon decided which treatment applied to their patients. Lastly, the surgeon will consider the challenges faced by presenting them to patients by informing them of the risks and benefits of any intervention.
The goal of this recap is to improve and accelerate the process, whether by eliminating the difficulties by asking help from experts, to make it easier the next time.
ConclusionThis article shares the main tools to properly carry out an evidence-based surgery. Without a doubt, this change is necessary, since it is an ethical obligation do to our work and evidence-based surgery is a tool providing order and systematising the search for the best available information, based on the surgeon's experience, so that together we can chose the best option for our patients. This implies a learning process, to know how to make the right question and obtain the information, as well as the clinical application and critical assessment of the process. This is an invitation for all surgeons to learn more from it and apply it in all areas, not only the clinical area, but also teaching of future consultants and research, to orient them to carry out works with more methodological weight. Many of us were not instructed in this, but without a doubt today we have the chance to learn to use this practical tool, which can become a powerful ally to improve our skills.
Conflicts of interestNone declared.
Please cite this article as: Duran-Vega HC. Cirugía basada en la evidencia. Una herramienta necesaria. Cir Cir. 2015;83:265–70.