Introduction
Drug dependence is a primary care problem that has yet to be solved. Drug use habits are changing, and certain drugs are now perceived as «normal» (e.g., alcohol, synthetic drugs and cannabis), while others are still considered unacceptable (e.g., heroin). Moreover, the age of initiation of drug addiction continues to fall. These factors lead to a user profile that clearly differs from the archetype of the «drug addict:» dependent on intravenous heroin, marginalized, extremely precarious lifestyle characterized by serious judicial and health problems,1 etc. The «new drug addict» has begun to turn to health and social services which are assumed to be nonspecific, standardized, and able to solve the patient's problem. The role of primary care is therefore indispensable, inasmuch as consumers of the «new drugs» fail to use specific services specialized in helping drug dependent persons who are in poor physical health and whose problems have become chronic.2,3
The «classical» drug dependent population comprises a varied group of individuals in which there is little relationship between intravenous drug users and persons who use other routes of administration,4,5 between those who are actively consuming drugs and those who are in rehabilitation, and between those receiving treatment with opiate agonists and those taking part in drug-free programs. As a result, different studies have reported results that are generally not comparable simply because the populations selected are different.
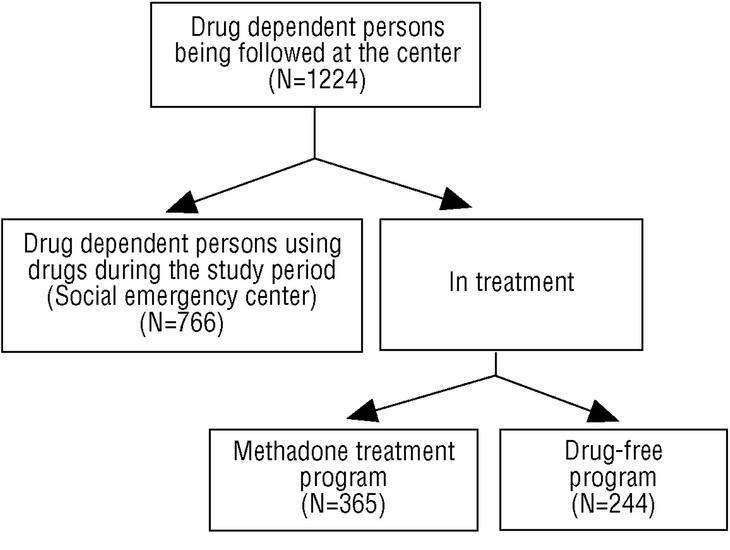
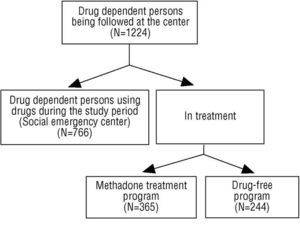
A variety of resources are available for persons with drug dependence. Social emergency centers (SEC) are available for drug dependent persons who are actively using drugs. The services these centers provide aim to reduce the damage without requiring abstinence as a condition, e.g., needle exchange, rest, personal hygiene, health care and heath educational.6 Methadone maintenance programs (MMP), offered as a low-commitment resource,7,8 are offered for heroin dependent persons, and are usually used by persons whose problems have become chronic. Drug-free programs (DFP), in contrast, are high-commitment programs that are usually aimed at persons whose personal and social circumstances are more favorable.
The hypothesis we studied was that there would be differences in demographic and health characteristics and in drug use patterns between different groups of drug dependent persons.
Methods
We retrospectively reviewed the medical records of drug dependent persons who were participating in different programs (SEC for users who were actively consuming drugs, MMP and DRP for users in treatment) between 1 January 2000 and 20 June 2002. Information was recorded for the following variables: main program the user was participating in, sex, age, age at the start of drug use, main drug, route of administration, serological findings for human immunodeficiency (HIV), hepatitis A (HAV) and hepatitis B (HBV) virus infection (antiHBc antibodies or HBs antigen was considered a positive test result), hepatitis C (HCV) virus infection and tuberculosis infection (PPD+). For tuberculosis, a wheal larger than 5 mm in the Mantoux test or larger than 15 mm in patients with BCG vaccination was considered a positive test result. We also noted whether the results of the tests for these infectious diseases were included in the patient's medical record.
Statistical analysis
Quantitative variables that showed a normal distribution were reported as mean values, which were compared with Student's t test. Variables that did not show a normal distribution were compared with the Mann-Whitney U test. Associations between qualitative variables were identified with the *2 test. The level of statistical significance was set at P<.05. All statistical tests were done with version 6 of the Epi Info program.
Results
We identified a total of 1224 users (predominantly male). Almost half of whom were current or former multiple intravenous substance abusers (Table 1).
Table 2 shows the prevalence of the infections we recorded (HIV, HAV, HBV, HCV and tuberculosis) and the percentage of users for whom the results of the laboratory test for AIDS, hepatitis or tuberculosis were known. The data are shown for all participants and for each program separately.
Mean age of the user population was younger in women (32.6 vs 33.6 years, P<.001), but there was no significant difference between the sexes in mean age at the start of drug use. Intravenous drug users were older than users of different routes of administration, and the former were younger when they first started to use drugs (P<.001). Drug dependent persons on the DFP were younger and had started using drugs at a later age (and had therefore been using drugs for less time) in comparison to active drug users (SEC) (P<.001) or users on the MMP (P=.001). Users with viral infections (HIV and hepatitis) and tuberculosis were generally older and had started using drugs at a younger age, with the exception of HAV carriers and users with a positive PPD test for tuberculosis, who started drug use at significantly older ages (P<.001). During the study period we found no differences in current age or age at the start of drug use among users in different treatment programs.
Intravenous drug use was more frequent among men (52.8%) than among women (35.1%; P<.001). The sex ratio in different treatment programs differed: although men were more numerous in all programs, the difference between men and women was greatest in the DFP.
There were no differences between men and women in the prevalence of viral infection, but the prevalence of tuberculosis infection was greater in men (44% vs 31.3%; P<.001). The distribution of these infectious diseases between men and women did not vary during the study period.
Users who were consuming drugs during the 30-month study period were most often those who used injection drugs (P<.001). Among persons under treatment during the study period, intravenous drug use was more frequent among participants in the MMP than among those in the DFP (P<.001). During the preceding two years we found no changes in the types of drug use. The prevalence of HIV, HVB and HVC infection was significantly higher among injection drug users than in other users. Moreover, we noted an association between tuberculosis infection and injection drug addiction, but no differences the prevalence of HAV infection between users of different routes of administration (P<.001).
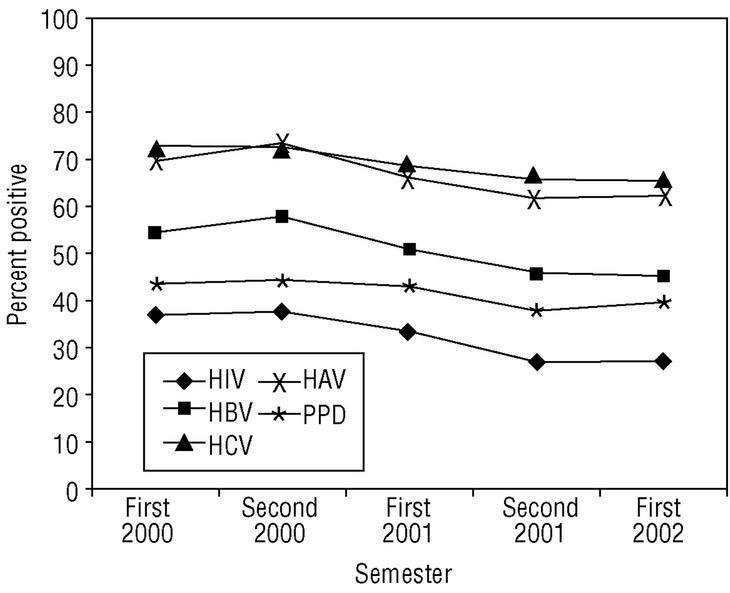
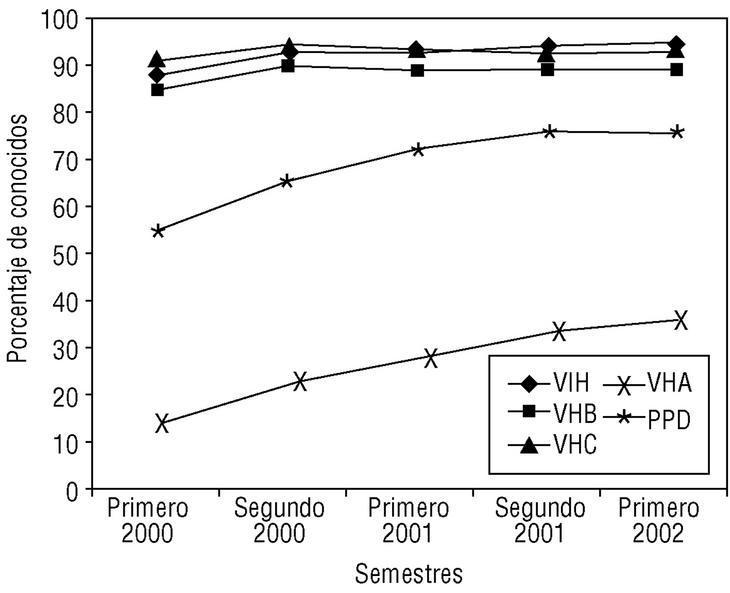
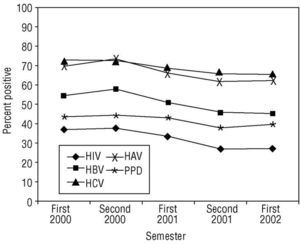
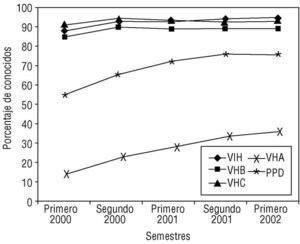
The prevalence of different infections is shown in Table 2. Figures 1 and 2 illustrate the changes with time in the prevalence of different infections and in the percentage of patients in each program and in each semester for whom information on these infections was available.
Among users who were consuming drugs during the study period, the prevalence of HIV, HBV and HCV infection was significantly higher than among drug dependent persons in rehabilitation. In the former group some figures were as much as threefold as high as in users who were receiving treatment.
Among drug dependent persons in the MMP, the prevalence of HIV, HBV and HCV was much higher than among participants in the DFP.
There were no differences in the prevalence of tuberculosis infection or HAV infection between any of the groups.
With regard to the information available about infectious diseases, the results were satisfactory in all programs for the diagnosis of HIV, HBV and HCV infection, which had been tested for in more than 90% of the users. However, the results were worse for tuberculosis: in more than 30% of the drug dependent persons whose records we reviewed, no information was given regarding this disease. The results for HAV infection reflect the recent implementation of a program aimed specifically at detecting antiHAV antibodies in SEC programs. In general, information on infectious diseases tended to be available for a larger percentage of users in rehabilitation than for users who were not participating in any treatment program during the study period.
We also noted a slight tendency for the prevalence of all infections to decrease during the study period; this tendency was significant for HIV and HBV (P=.003). We also noted an increase during the study period in the number of users for whom test results for these diseases were recorded. Significant improvements were seen in the number of users with HIV, HAV and tuberculosis infection (P<.001), and nonsignificant improvements were seen for HBV and HCV infection.
Discussion
There were clear differences in the demographic, drug use and health characteristics of our users. We found that drug dependent persons who were consuming drugs during the study period were older, had begun to use drugs at a younger age, and more often used injection drugs. The sex ratio for active consumers was closer to 1 than in the other groups we studied, and the prevalence of chronic infectious diseases was higher in this group.
In contrast, users in the DFP were usually younger, had used drugs for shorter periods, used mainly inhalation drugs, and were in better general heath.
Users in the MMP showed intermediate characteristics.9 The sex ratio was similar to that in the group of active drug users. The prevalence of infectious diseases was between that in other the two groups, although it was closer to the figure for persons who were using drugs.
The >60% prevalence of antiHAV antibodies in all subgroups appears to support the usefulness of prevaccination testing in all drug dependent individuals to identify those who may benefit from anti-hepatitis A vaccination.10
We found no differences in the prevalence of tuberculosis infection between the different groups of drug users. In general, the prevalence was lower than in other studies.11 In an earlier (unpublished) report by our group, we concluded that the number of expected cases of tuberculosis for the year 2000 among drug dependent persons who were seen at the SEC was 8.6; this figure illustrates the importance of programs designed to actively seek and identify persons with tuberculosis in order to treat latent infections.12
In addition to these differences, we found that the types of service that required greater commitment on the part of the drug user, i.e., those that provided care for users in better physical health, tested for and diagnosed infectious diseases in larger percentages of patients. In contrast, programs that provided care for drug dependent persons who were using drugs and who were in worse health tested for and documented infectious disease status in a lower proportion of users. We can therefore expect the rate of chronic infectious disease to remain considerable among these users.
To summarize, users who were not in rehabilitation were in worse health, and were less frequently diagnosed at primary care centers as having infectious diseases. We observed a slight improvement during the study period in the health of these users, and a tendency for primary care health interventions to improve.
New approaches to therapy (for example, prescriptions for heroin)13 may allow us to provide care for those substance abusers whom current programs still fail to reach.
Acknowledgments
We thank María Gutiérrez-Cortines and the staff of the Association for Aid to Drug Dependent Persons (Asociación de Ayuda al Drogodependiente, ACLAD) in Valladolid.