Acute kidney injury (AKI) is prevalent and has deleterious effects on postoperative outcomes following liver transplantation (LT). The impact of nonselective beta-blockers (NSBBs) in patients with liver cirrhosis remains controversial. This study investigated the association between preoperative NSBB use and AKI after living donor LT (LDLT).
Patients and MethodsWe evaluated 2,972 adult LDLT recipients between January 2012 and July 2022. The patients were divided into two groups based on the preoperative NSBB use. Propensity score matched (PSM) and inverse probability of treatment weighting (IPTW) analyses were performed to evaluate the association between preoperative NSBB use and postoperative AKI. Multiple logistic regression analyses were also used to identify the risk factors for AKI.
ResultsThe overall incidence of AKI was 1,721 (57.9%) cases. The NSBB group showed a higher incidence of AKI than the non-NSBB group (62.4% vs. 56.7%; P = 0.011). After PSM and IPTW analyses, no significant difference in the incidence of AKI was found between the two groups (Odds ratio, OR 1.13, 95% confidence interval, CI 0.93–1.37, P = 0.230, PSM analysis; OR 1.20, 95% CI 0.99–1.44, P = 0.059, IPTW analysis). In addition, preoperative NSBB use was not associated with AKI after multivariate logistic regression analysis (OR 1.16, 95% CI 0.96–1.40, P = 0.118).
ConclusionsPreoperative NSBB use was not associated with AKI after LDLT. Further studies are needed to validate our results.
Acute kidney injury (AKI) is a frequent complication after liver transplantation (LT), with detrimental effects on patient outcomes. Studies have reported a wide range of incidence rates for post-LT AKI, ranging from 17% to over 90% [1,2]. Additionally, rates for renal replacement therapy have been reported to range from 8 to 20% [3,4]. Post-LT AKI has been consistently shown to impact post-transplant outcomes. Even mild AKI following LT increased the risk of post-LT chronic kidney disease (CKD) and decreased patient and graft survival rates [3,5–7]. Therefore, it would be beneficial to identify and mitigate the risk factors that can deteriorate renal function to improve postoperative outcomes after LT.
Nonselective beta-blockers (NSBBs) have been the mainstay treatment for portal hypertension in patients with liver cirrhosis (LC) [8]. Response to NSBB therapy is associated with a lower risk of portal hypertension-related complications, including variceal rebleeding, ascites, and spontaneous bacterial peritonitis (SBP), as well as improved survival rates [9,10]. However, recent studies have raised concerns about the potential negative impact of NSBB therapy in patients with end-stage liver disease [11–14]. The cardio-inhibitory effects of NSBBs may reduce the cardiac compensatory reserve, which is essential for renal and hepatic perfusion [14,15], leading to renal failure and poor survival in patients with liver cirrhosis with ascites [16–18].
Although the impact of NSBBs on AKI has been investigated in various patient populations [12,13,19,20], there is a lack of research on the influence of preoperative NSBB use on the incidence of postoperative AKI in LT recipients. Therefore, we investigated the association between preoperative NSBB use and postoperative AKI in living donor LT (LDLT) recipients. We hypothesized that preoperative NSBB therapy in LDLT recipients might have a negative impact on renal outcomes after LDLT.
2Patients and methods2.1PatientsThe Institutional Review Board of Asan Medical Center approved this study (protocol number: 2023–0561) and waived the need for informed consent due to the retrospective nature of the study. We reviewed the electronic medical records of all patients who underwent LT at Asan Medical Center between January 2012 and July 2022. This study included adult patients (≥18 years) who underwent LDLT. Patients with a preoperative serum creatinine (sCr) level > 1.4 mg/dL, those diagnosed with CKD or hepatorenal syndrome (HRS), or those receiving hemodialysis at baseline were excluded from the study. The remaining patients were divided into two groups based on their preoperative NSBB use for at least one month. At our center, LT candidates who may benefit from NSBBs are selected by hepatologists and prescribed NSBBs for both primary and secondary prophylaxis against variceal bleeding, as well as for the potential prevention of further decompensation [21–24].
2.2Clinical dataClinical data were extracted from an electronic medical records system, including demographic data, donor-related variables, perioperative laboratory results, intraoperative records containing details of anesthetic management and surgical procedures, and postoperative outcomes. The demographic data included preoperative characteristics of recipients, including beta-blocker use, patient age, sex, and body mass index (BMI); comorbidities, such as diabetes mellitus, hypertension, and coronary arterial disease; liver disease characteristics, such as the etiology of LC (hepatitis B virus, hepatitis C virus [HCV], alcoholic LC, and other disease), Model for End-Stage Liver Disease (MELD) score, Child-Pugh-Turcotte score; SBP; intractable ascites; dual donor grafts; and ABO incompatibility (ABOi). Donor-related variables included donor age, sex, and total fatty change. Laboratory data included prothrombin time–international normalized ratio (PT-INR), albumin, total bilirubin, creatinine, and estimated glomerular filtration rate (eGFR). Intraoperative data included severe post-reperfusion syndrome (PRS), volume and type of fluids (crystalloid and colloid), volume of blood components (packed red blood cells [pRBCs] and fresh frozen plasma [FFP]), massive transfusion, inotrope/vasopressor use, urine output, anesthetic time, cold ischemic time, warm ischemic time, total ischemic time, graft-to-recipient weight ratio, bio-pump use, and intraoperative embolization. PRS was defined as a decrease in mean arterial pressure by more than 30% compared to the pre-reperfusion level, persisting for at least 1 min within the initial 5 min following the reperfusion of the liver graft [25]. In addition, PRS was considered severe if there was a requirement for over 30 μg of epinephrine during the reperfusion phase [26]. Massive transfusion was defined as transfusion of ≥10 pRBC units within 24 h, or >4 pRBC units in 1 h [27].
2.3Primary and secondary outcomesThe primary outcome of this study is postoperative AKI, which was diagnosed according to the Kidney Disease Improving Global Outcome criteria. AKI was defined as an increase in sCr by ≥0.3 mg/dL within 48 h postoperatively or an increase in sCr to ≥1.5 times the baseline value within postoperative day 7 [28]; baseline sCr was measured the day before LT as our routine protocol for LDLT recipients [29]. More specifically, stage 1 was defined as an increase in sCr to 1.5–1.9 times baseline or an increase in sCr by ≥0.3 mg/dL. Stage 2 was defined as an increase in sCr to 2.0–2.9 times baseline, while stage 3 was defined as an increase in sCr to 3.0 times baseline or an increase in sCr to ≥4.0 mg/dl, or the initiation of renal replacement therapy [28].
Secondary outcomes include 1-year graft failure and mortality, overall graft failure, and overall mortality. Graft failure was defined as re-transplantation or death. We reviewed electronic medical records and the regularly updated Asan Organ Transplantation Center registry to determine graft failure and mortality incidence.
2.4Statistical analysisContinuous variables are reported as mean ± standard deviation or median with interquartile range (IQR), and categorical variables are reported as frequencies with percentages. According to the use of preoperative NSBBs, patients were divided into the NSBB and non-NSBB groups. Between-group comparisons were conducted using the Student t-test or the Mann–Whitney U test for continuous variables, and the Chi-square test or the Fisher exact test for categorical variables, as appropriate.
Propensity scores (PSs) were calculated to balance confounding variables and reduce selection bias between the NSBB and non-NSBB groups, using logistic regression based on all preoperative data, including demographic variables, donor-related variables, and laboratory variables listed in Table 1. Model discrimination was evaluated using C statistics (c-statistics = 0.650), and calibration was assessed using Hosmer–Lemeshow statistics (P = 0.166). The baseline characteristics of the NSBB group and non-NSBB group were balanced using propensity score matched (PSM) analysis and inverse probability of treatment weighting (IPTW) analyses. However, there were disparities in some important intraoperative variables, such as severe PRS, massive transfusion, and anesthetic time between the NSBB and non-NSBB groups after PS matching. Given that these variables could confound the relationship between preoperative NSBB use and post-LT AKI, we made additional adjustments for these variables in both PSM and IPTW analyses.
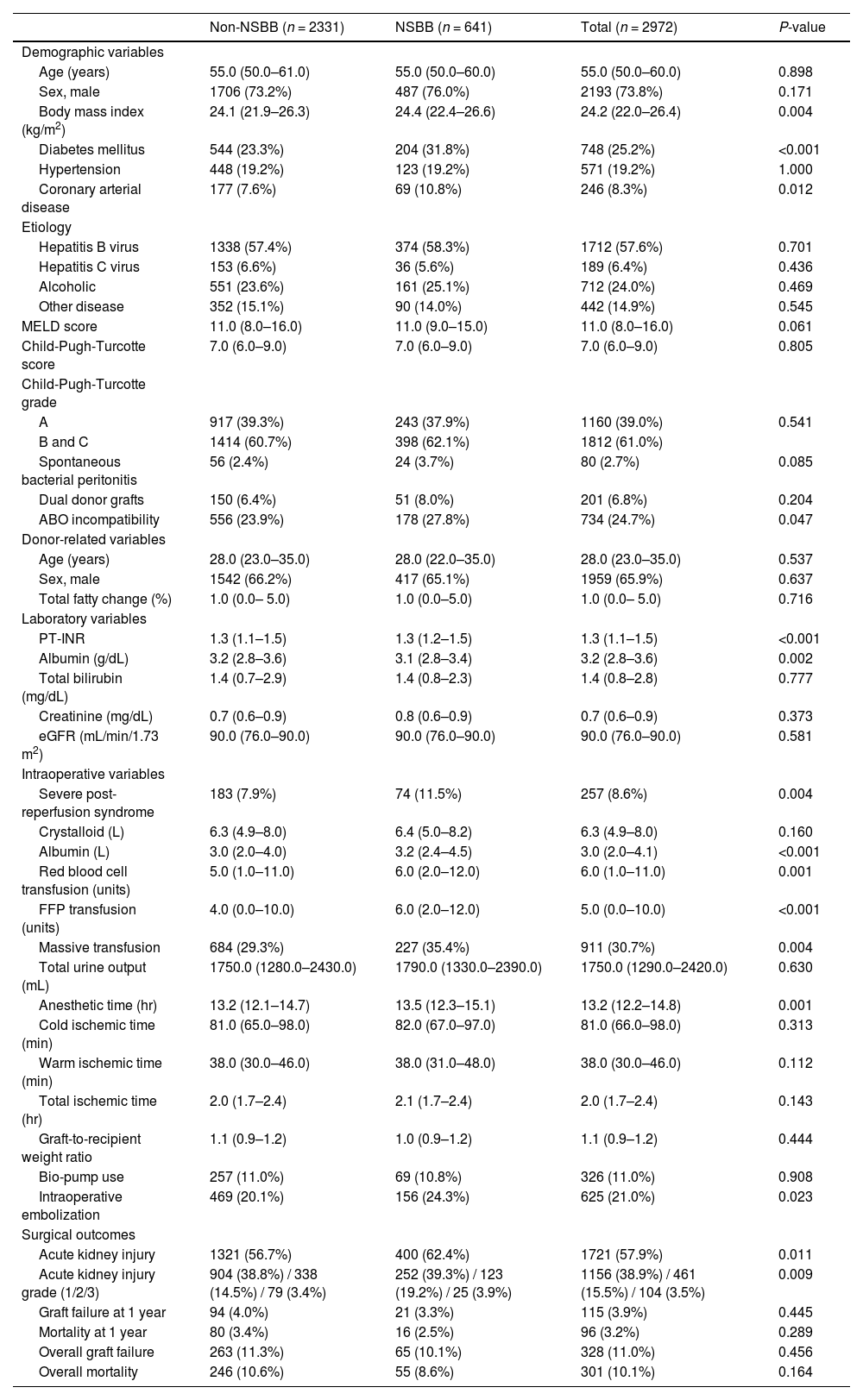
Perioperative characteristics and postoperative outcomes of the study population.
Values are expressed as mean ± standard deviation, median (interquartile range), or number of patients (%), as appropriate. NSBB, Nonselective beta blocker; MELD score, Model for end-stage liver disease score; PT-INR, prothrombin time–international normalized ratio; eGFR, estimated glomerular filtration rate; FFP, fresh frozen plasma.
The association between preoperative NSBB use and post-LT outcomes was evaluated using multivariate logistic regression and Cox proportional hazard regression analyses. Multivariate logistic regression analysis was used to identify the factors associated with post-LT AKI. Variables with P-values <0.1 in the univariate analysis were included in the multivariate analysis. Multivariate Cox regression analysis was used to assess the factors associated with 1-year graft failure and mortality, overall graft failure, and overall mortality. Backward elimination was used to develop the final model, and adjusted odds ratio (OR) or hazard ratio (HR) was calculated.
All P-values <0.05 were considered statistically significant. Data manipulation and statistical analyses were performed using SPSS 22.0 (IBM Corp., Armonk, NY, USA) and R 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).
2.5Ethical statementThe Institutional Review Board of Asan Medical Center approved this study (protocol number: 2023-0561).
3ResultsWe included 2972 adult LDLT recipients in this study, and the median follow-up time was 4.7 years (IQR 2.3–7.5 years). Based on preoperative NSBB use, the 2972 patients were divided into the non-NSBB group (n = 2331) and the NSBB group (n = 641). The duration and dosage for patients in the NSBB group were as follows: For propranolol, the median duration of use was 142 days (IQR 67–456 days) with a median dosage of 40 mg/day (IQR 20–40 mg/day). For carvedilol, the median duration was 93 days (IQR 45–178 days) with a median dosage of 12.5 mg/day (IQR 6.2–13.2 mg/day). Table 1 shows their preoperative and intraoperative data and surgical outcomes. The NSBB group included a higher proportion of patients with diabetes mellitus and coronary arterial disease. They had a higher BMI, a longer PT-INR, and lower albumin levels than the non-NSBB group. Additionally, they were more likely to undergo ABOi LT. Intraoperatively, these patients experienced a higher incidence of severe PRS, required more albumin infusions, had a greater need for pRBC and FFP transfusions, underwent embolization of the remaining portosystemic shunts performed by interventional radiologists more frequently, and had a longer anesthetic time. Among the 2972 LDLT recipients, the incidence of AKI was 57.9% (n = 1721). The incidence of 1-year graft failure and mortality was 3.9% (n = 115) and 3.2% (n = 96), respectively. The graft failure and overall mortality rates were 11.0% (n = 328) and 10.1% (n = 301), respectively. When comparing the incidence of AKI, there was a statistically significant difference between the two groups (62.4% in the NSBB group and 56.7% in the non-NSBB group, P = 0.011). Specifically, in the non-NSBB group, 38.8% (n = 904) patients had AKI stage 1, 14.5% (n = 338) had stage 2, and 3.4% (n = 79) had stage 3. In contrast, the NSBB group had 39.3% (n = 252) cases in Stage 1, 19.2% (n = 123) in Stage 2, and 3.9% (n = 25) in Stage 3 (P = 0.009).
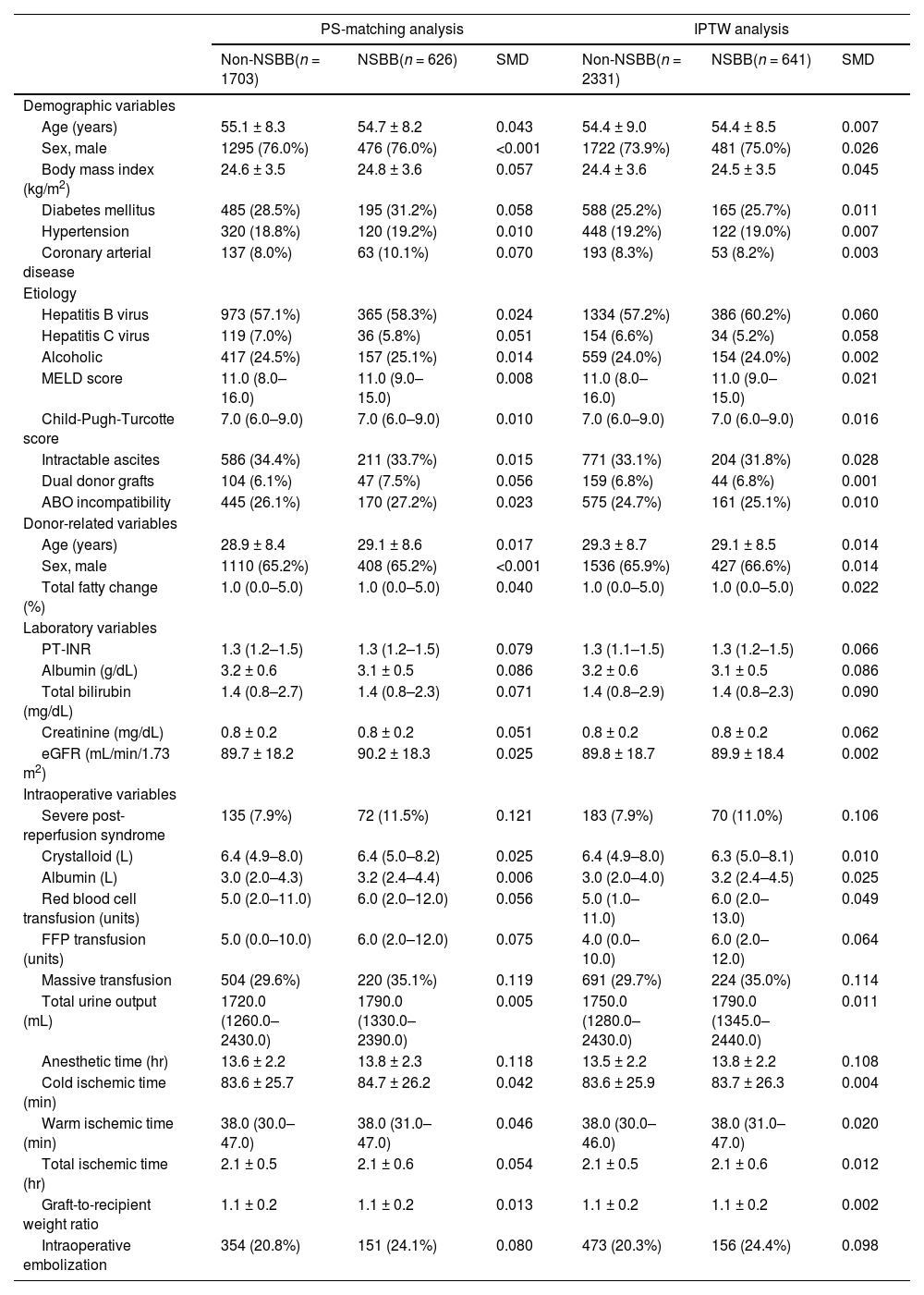
Table 2 shows preoperative and intraoperative characteristics of PSM patients (1:1 to 1:3 matched set, n = 2329 total set, n = 1703 in non-NSBB group and n = 626 in NSBB group). After PS matching, no significant differences were observed in demographic, donor-related, and preoperative laboratory variables between NSBB and non-NSBB groups. The incidence of post-LT AKI was 62.5% (n = 391) in the NSBB group and 57.8% (n = 984) in the non-NSBB group after PSM analysis.
Perioperative characteristics of the study population after PS-matching and IPTW analysis.
Values are expressed as mean ± standard deviation, median (interquartile range), or number of patients (%), as appropriate. PS, propensity score; IPTW analysis, inverse probability of treatment weighted analysis; NSBB, Nonselective beta blocker; SMD, standardized mean difference; MELD score, Model for end-stage liver disease score; PT-INR, prothrombin time–international normalized ratio; eGFR, estimated glomerular filtration rate; FFP, fresh frozen plasma.
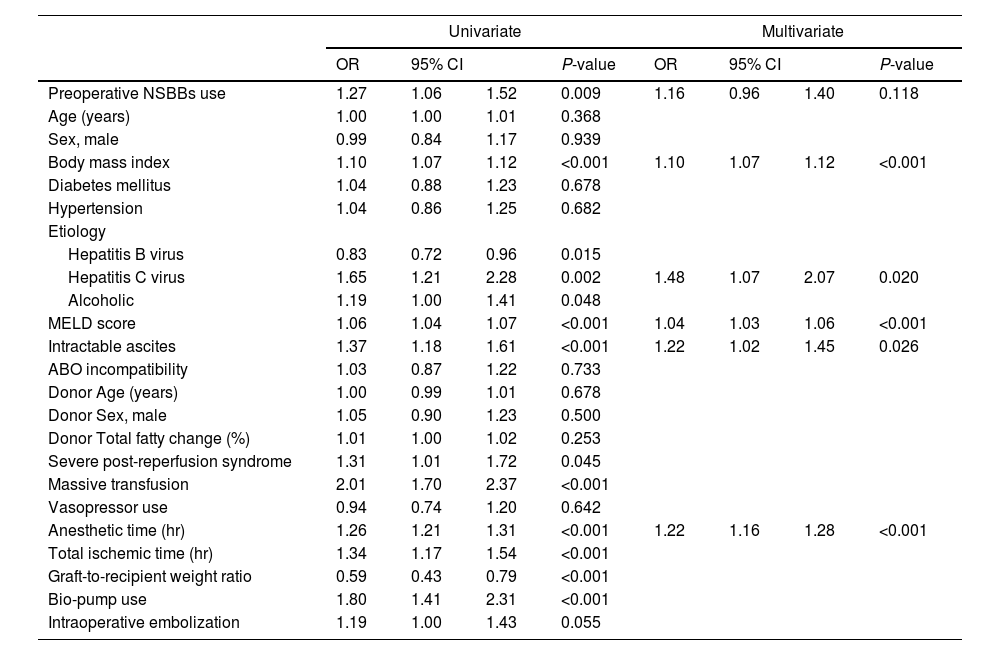
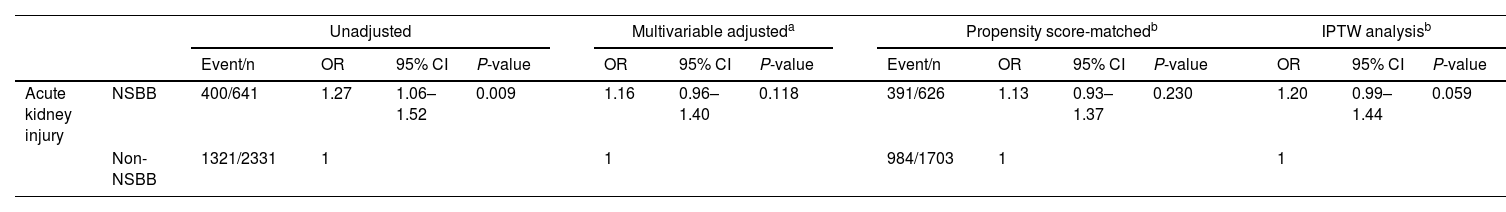
In the univariate logistic regression analysis, preoperative NSBB use was associated with post-LT AKI (OR 1.27, 95% confidence interval, CI 1.06–1.52, P = 0.009) (Table 3). However, after adjusting variables related to AKI, preoperative NSBB use was not associated with post-LT AKI (OR 1.16, 95% CI 0.96–1.40, P = 0.118). However, BMI (OR 1.10, 95% CI 1.07–1.12, P < 0.001), HCV (OR 1.48, 95% CI 1.07–2.07, P = 0.020), MELD score (OR 1.04, 95% CI 1.03–1.06, P < 0.001), intractable ascites (OR 1.22, 95% CI 1.02–1.45, P = 0.026), and anesthetic time (OR 1.22, 95% CI 1.16–1.28, P < 0.001) were associated with post-LT AKI. Furthermore, preoperative NSBB use was not significantly associated with post-LT AKI in PSM analysis (OR 1.13, 95% CI 0.93–1.37, P = 0.230) and IPTW analysis (OR 1.20, 95% CI 0.99–1.44, P = 0.059) (Table 4).
Multivariate logistic regression analysis for acute kidney injury after living donor liver transplantation.
NSBBs, Nonselective beta-blockers; MELD score, Model for end-stage liver disease score; OR, odds ratio; CI, confidence interval.
Predictive value of preoperative NSBBs for acute kidney injury after living donor liver transplantation.
| Unadjusted | Multivariable adjusteda | Propensity score-matchedb | IPTW analysisb | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Event/n | OR | 95% CI | P-value | OR | 95% CI | P-value | Event/n | OR | 95% CI | P-value | OR | 95% CI | P-value | ||||||
| Acute kidney injury | NSBB | 400/641 | 1.27 | 1.06–1.52 | 0.009 | 1.16 | 0.96–1.40 | 0.118 | 391/626 | 1.13 | 0.93–1.37 | 0.230 | 1.20 | 0.99–1.44 | 0.059 | ||||
| Non-NSBB | 1321/2331 | 1 | 1 | 984/1703 | 1 | 1 | |||||||||||||
No significant difference was observed in the incidence of 1-year graft failure and mortality, overall graft failure, or overall mortality between the NSBB group and the non-NSBB group (all P-values >0.05) (Table 1). Cox proportional regression analysis revealed that preoperative NSBB use was not associated with 1-year graft failure and mortality, overall graft failure, or overall mortality (HR 0.81, 95% CI 0.50–1.30, P = 0.373; HR 0.72, 95% CI 0.42–1.23, P = 0.233; HR 0.86, 95% CI 0.66–1.13, P = 0.283; HR 0.77, 95% CI 0.58–1.04, P = 0.085, respectively). In PSM analysis, preoperative NSBB use was not associated with 1-year graft failure and mortality, overall graft failure, or overall mortality (HR 0.78, 95% CI 0.48–1.27, P = 0.315; HR 0.69, 95% CI 0.39–1.20, P = 0.186; HR 0.85, 95% CI 0.64–1.13, P = 0.264; HR 0.76, 95 % CI 0.56–1.03, P = 0.076, respectively). In IPTW analysis, preoperative NSBB use was not associated with 1-year graft failure and mortality, overall graft failure, or overall mortality (HR 0.68, 95% CI 0.42–1.12, P = 0.133; HR 0.60, 95% CI 0.35–1.06, P = 0.078; HR 0.86, 95% CI 0.64–1.14, P = 0.288; HR 0.76, 95% CI 0.56–1.03, P = 0.080).
4DiscussionLDLT recipients who used NSBBs preoperatively had a higher incidence of post-LT AKI than those who did not. However, no significant association was found between preoperative NSBB use and post-LT AKI in multivariate, PSM, and IPTW analyses. In addition, no significant association was found between preoperative NSBB use and 1-year graft failure and mortality, overall graft failure, or overall mortality.
NSBBs have played a fundamental role in preventing portal hypertension-related complications in patients with cirrhosis for decades. LT candidates benefit from NSBBs for both primary and secondary prophylaxis against variceal bleeding, as well as for the potential prevention of further decompensation and death [21–24]. However, NSBBs may be harmful, particularly in patients with decompensated LC [11,30,31]. Mechanically, in decompensated LC, activation of the sympathetic nervous system leads to increased left ventricle systolic function, as an adaptive mechanism to maintain renal perfusion. Beta-blockade may blunt this sympathetic overdrive, lowering cardiodynamic reserve and renal perfusion pressure, resulting in impaired renal function [16–18,32]. Although AKI frequently occurs after LT and has deleterious effects on long-term outcomes [1–3,5–7], the impact of preoperative NSBB use on post-LT AKI has not been evaluated.
Studies have reported conflicting results about the effects of NSBBs on renal function in patients with LC. A retrospective cohort study reported that NSBB use was neither associated with a deterioration of renal function nor an increase in AKI incidence in patients with LC with gastroesophageal varices [20]. Their findings are consistent with ours, but their study mostly included patients with compensated LC. Another retrospective study reported that NSBBs increased the risk for HRS and AKI in patients with cirrhosis and SBP [13]. However, the association was assessed only through Pearson's chi-square test. In addition, a nested case-control study of LT candidates reported that NSBBs significantly increased AKI in patients with ascites while they decreased AKI in patients without ascites [19]. However, their case and control groups were matched using a limited set of variables: age, sCr, MELD-Na scores at baseline, and follow-up duration. All these mentioned studies focused on patients with LC prior to their operations. However, the development of post-LT AKI is influenced not only by preoperative factors but also by the factors encountered during the surgical process. Therefore, our research carries clinical significance as the first to investigate the association between preoperative NSBBs use and post-LT AKI in LDLT recipients. We used multivariate, PSM, and IPTW analyses to adjust for a wide range of preoperative and intraoperative variables to assess the association between preoperative NSBB use and the development of AKI after LT.
Patients undergoing various surgeries have shown inconsistent outcomes on the impact of preoperative beta blockers (BBs) on postoperative AKI. A large multicenter cohort study found no significant association between preoperative BBs within 24 h of elective coronary artery bypass surgery and perioperative outcomes, including renal failure in PSM analysis [33]. In another study including ASA 1–2 patients undergoing non-cardiac surgery, preoperative BBs were significantly associated with postoperative AKI in univariate analysis but not in multivariate analysis [34]. Acute BBs use independently predicted postoperative AKI in hypertensive patients undergoing non-suprainguinal vascular surgery, likely due to kidney ischemic injury from global perioperative hypotension [35]. Lastly, regular preoperative use of anti-adrenergic agents (alpha and/or beta-blockers) was independently associated with the development of AKI after non-cardiac surgeries in both multivariate and PSM analyses [36]. However, these studies reported the incidence rates of postoperative AKI to be 2–6%, significantly lower than the 17–90% observed in LT recipients. This discrepancy can be attributed to the unique circumstances associated with LC patients, often complicated by cirrhotic cardiomyopathy. Furthermore, the large intraoperative hemodynamic fluctuations that can occur during LT due to factors such as inferior vena cava clamping, PRS, massive bleeding, or massive transfusions may contribute to this discrepancy. Therefore, findings from other surgeries may not be directly applicable to LT recipients.
Post-LT AKI has been reported to be related to MELD, BMI, HCV, intractable ascites, and anesthetic time [37–40]. Therefore, our findings of the factors associated with post-LT AKI in the multivariate analysis are consistent with those of previous studies. Meanwhile, no significant differences were observed between preoperative NSBB use and 1-year graft failure and mortality, overall graft failure, or overall mortality in our study. Many studies have explored the impact of NSBBs on survival in patients with LC with conflicting results [11,13,30,41,42]. Furthermore, a recent study reported that the incidences of graft failure were 8.7%, 14.2%, 19.4%, and 42.0% for adult LDLT, and the incidences of mortality were 7.8%, 13.3%, 18.6%, and 35.9% for adult LT at 1,3,5, and 10 years, respectively [43]. Notably, our results showed a lower incidence of postoperative graft failure and mortality, suggesting that a larger sample size may be needed for more robust conclusions.
Our study has several limitations. First, its retrospective nature may introduce confounding factors and selection bias. We used multivariate, PSM, and IPTW analyses to mitigate these issues. Second, this research was conducted in a single center, one of the world's leading LT institutions, with an experienced surgical and perioperative management team, which may have affected postoperative outcomes, including AKI. Therefore, care should be given when generalizing our findings. Therefore, while this study provides valuable insights, further multicenter, prospective research is needed to confirm and expand upon our findings.
5ConclusionsIn conclusion, no significant association between preoperative NSBB use and postoperative AKI was observed after multivariate, PSM, and IPTW analyses in LDLT. These results suggest that preoperative NSBB use is not a significant risk factor for AKI following LDLT.
Author contributionsConceptualization: HWJ, JGS, GSH. Data curation: HWJ, JGS, JHK, SBH, HMK, IGJ. Formal analysis: HWJ, JGS, JHK, SBH, HMK, IGJ. Funding acquisition: did not receive any specific. grant. Investigation: HWJ, JGS. Methodology: HWJ, JGS. Project administration: HWJ, JGS. Resources: HWJ, JGS, GSH. Software: HWJ, JGS. Supervision: HWJ, JGS, GSH. Validation: HWJ, JGS. Visualization: HWJ, JGS. Writing - original draft: HWJ, JGS. Writing - review & editing: HWJ, JGS,GSH. All the authors have read and approved the final manuscript.