SARS COV-2 infection is an emerging disease that has become a global pandemic since the beginning of 2020. To reduce transmission, measures have been imposed by governments such as home confinement, the use of masks, social distancing or promotion of hand hygiene. The aim of this study is to determine if the measures adopted to reduce the COVID-19 pandemic have produced a decrease in the incidence of infectious diseases and their complications in the ENT area in our center.
Material and methodsA retrospective descriptive study was carried out in a tertiary hospital of patients aged between 0 and 15 years who required admission due to deep cervical infections, complications derived from acute otitis media (mastoiditis or facial paralysis) or complicated acute sinusitis.
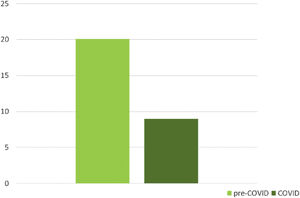
ResultsThere is a notable decrease in the number of global admissions in the COVID period (9) compared to the average of the previous 5 years (20.1). Likewise, there are statistically significant differences in the number of admissions for cervical infections (p value=0.027) and complications derived from acute otitis media (p value=0.029).
Discussion/conclusionA decrease in the number of admissions caused by complications of infections in the ENT area in paediatric patients has been observed after the start of the COVID-19 pandemic in our environment, this fact could be explained by a global decrease in the number of infections of the upper respiratory tract due to the hygienic measures taken by the COVID-19 pandemic.
La infección por SARS COV-2 es una enfermedad emergente que se ha convertido en pandemia mundial desde inicios del año 2020. Para disminuir el contagio se han impuesto medidas por parte de los gobiernos como son el confinamiento domiciliario, el uso de mascarillas, el distanciamiento social o la promoción de la higiene de manos. El objetivo de este estudio es determinar si las medidas adoptadas para frenar la pandemia COVID-19 han producido una disminución de la incidencia de enfermedades infecciosas y sus complicaciones en el área ORL en nuestro medio.
Material y métodosSe realizó un estudio descriptivo retrospectivo en un hospital terciario de pacientes con edades comprendidas entre 0 y 15 años que precisaron ingreso por presentar infecciones cervicales profundas, complicaciones derivadas de otitis media aguda (mastoiditis o parálisis facial) o sinusitis aguda complicada.
ResultadosExiste una disminución reseñable en el número de ingresos globales en el período COVID (9) respecto a la media de los 5 años previos (20,1). Así mismo, existen diferencias estadísticamente significativas en el número de ingresos de infecciones cervicales (pvalor=0,027) y de complicaciones derivadas de otitis media aguda (pvalor=0,029).
Discusión/conclusiónSe ha observado una disminución del número de ingresos provocados por complicaciones de infecciones del área ORL en pacientes pediátricos tras el inicio de la pandemia Covid-19 en nuestro medio, este hecho podría explicarse por una disminución global del número de infecciones de vía respiratoria superior debido a las medidas higiénicas tomadas por la pandemia COVID-19.
SARS COV-2 infection is an emerging disease primarily affecting the respiratory tract and can cause severe acute respiratory syndrome. It became a global pandemic from the beginning of 2020, with enormous health, social, and economic repercussions. Governments around the world imposed various measures in an attempt to curb the pandemic and stop its spread.
These measures decreed in Spain include the lockdown imposed from 14 March to 21 June 2020, the closure of schools, reduction of essential jobs, and restriction of movement over this period; classroom classes did not resume until September 2020. Other measures included the use of face masks, social distancing, and promotion of hand hygiene.
The aforementioned measures have been shown to reduce the transmission of COVID-19, however we know that they also reduce the transmission of other infectious diseases.1
Thus, the measures used to curb the transmission of SARS-COV-2 infection could result in decreased incidence of upper respiratory tract infections. These infections, although normally trivial, can lead to serious diseases such as cervical abscesses, mastoiditis, orbital cellulitis, or even brain abscesses, which require the patient to be admitted for their correct management.
The aim of this study was to determine whether the measures adopted to curb the COVID-19 pandemic have resulted in a decreased incidence of infectious diseases and their complications in the ENT area in our setting.
Material and methodsA retrospective descriptive study was conducted in a tertiary hospital of patients aged 0–15 years who were admitted due to deep cervical infections, complications arising from acute otitis media (AOM) such as mastoiditis or facial paralysis, or complicated acute sinusitis.
We studied all patients who required admission for the reasons described above to the Hospital Universitario y Politécnico La Fe from 1 March 2015 to 1 March 2021, covering a total of 6 years.
The criteria for hospital admission were patients with at least one of the following: airway compromise, intolerance or refusal of oral treatment, sepsis, high suspicion of purulent complications, no improvement after 48h of adequate medical treatment or the need for urgent surgical treatment.
To compare the periods, patients were classified into 12-month periods, taking the month of March of each year as the cut-off date; the month in which the preventive measures against the COVID-19 pandemic began in Spain. Six periods were obtained, classifying as the "COVID" period the 12 months from 1 March 2020 to 1 March 2021 and as the "pre-COVID" period the 5 periods from 2015 to 2020. The objective was to compare the number of infections occurring in the months when prevention measures were maintained with respect to the previous 5 years.
Age, sex, and aetiology according to the International Classification of the World Health Organisation (ICD-10) were the parameters gathered. The aetiologies were classified into three groups: cervical infections, AOM complications, and complicated acute sinusitis. The following diagnoses were included in the cervical infections group: peritonsillar abscess/phlegmon (J36), parapharyngeal abscess/phlegmon (J39.1), retropharyngeal abscess/phlegmon (J39.0), laterocervical abscess (L02.11), and neck abscess (L02.11). The following diagnoses were included in the AOM complications group: facial paralysis (G51.0), acquired facial paralysis (G51.9) + AOM (H66.90), and mastoiditis (H70.90). The following diagnoses were included in the complicated acute sinusitis group: acute pansinusitis (J01.40), sinusitis (J32.9), acute sphenoidal sinusitis (J01.30), acute ethmoidal sinusitis (J01.20), acute frontal sinusitis (J01.10), acute maxillary sinusitis (J01.00).
We analysed the incidence of each group of diseases and of each individual aetiology in each of the periods. The incidence during the "COVID" period was then compared with the "pre-COVID" period for each group and for each individual aetiology. The Wilcoxon test was used for statistical analysis using the R studio programme.
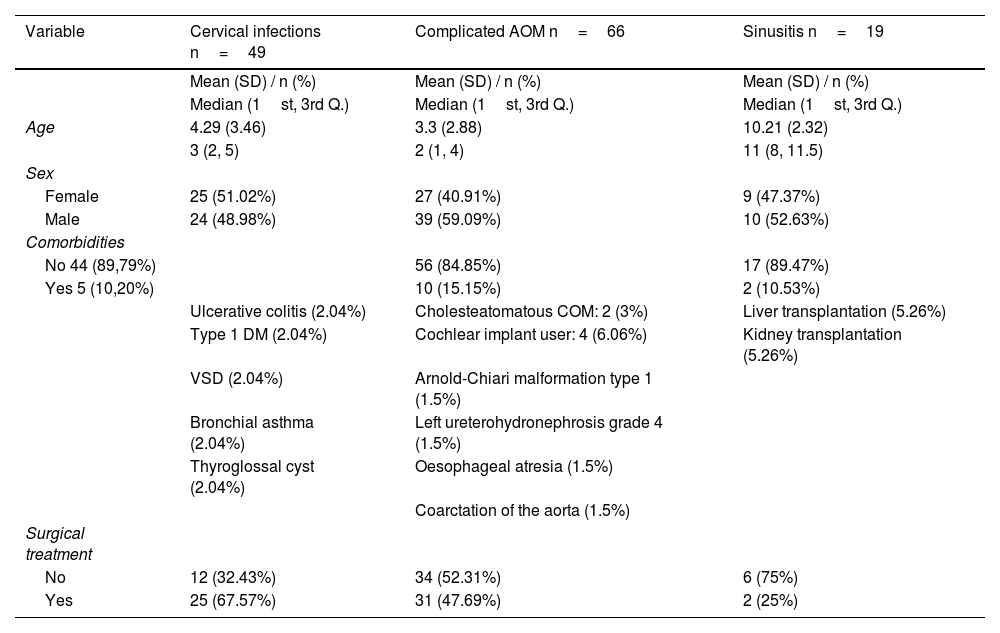
ResultsA total of 134 patients were included in the study, 73 males (54.48%) and 61 females (45.52%). Table 1 details the demographic characteristics and comorbidities of the study population.
Demographic characteristics and comorbidities of the sample.
| Variable | Cervical infections n=49 | Complicated AOM n=66 | Sinusitis n=19 |
|---|---|---|---|
| Mean (SD) / n (%) | Mean (SD) / n (%) | Mean (SD) / n (%) | |
| Median (1st, 3rd Q.) | Median (1st, 3rd Q.) | Median (1st, 3rd Q.) | |
| Age | 4.29 (3.46) | 3.3 (2.88) | 10.21 (2.32) |
| 3 (2, 5) | 2 (1, 4) | 11 (8, 11.5) | |
| Sex | |||
| Female | 25 (51.02%) | 27 (40.91%) | 9 (47.37%) |
| Male | 24 (48.98%) | 39 (59.09%) | 10 (52.63%) |
| Comorbidities | |||
| No 44 (89,79%) | 56 (84.85%) | 17 (89.47%) | |
| Yes 5 (10,20%) | 10 (15.15%) | 2 (10.53%) | |
| Ulcerative colitis (2.04%) | Cholesteatomatous COM: 2 (3%) | Liver transplantation (5.26%) | |
| Type 1 DM (2.04%) | Cochlear implant user: 4 (6.06%) | Kidney transplantation (5.26%) | |
| VSD (2.04%) | Arnold-Chiari malformation type 1 (1.5%) | ||
| Bronchial asthma (2.04%) | Left ureterohydronephrosis grade 4 (1.5%) | ||
| Thyroglossal cyst (2.04%) | Oesophageal atresia (1.5%) | ||
| Coarctation of the aorta (1.5%) | |||
| Surgical treatment | |||
| No | 12 (32.43%) | 34 (52.31%) | 6 (75%) |
| Yes | 25 (67.57%) | 31 (47.69%) | 2 (25%) |
Nine patients were included in the “COVID” period, 5 males (55.56%) and 4 females (44.44%), with a mean age of 5.52 years. During assessment in the emergency department and prior to hospital admission, a study of SARS-Cov-2 infection was performed by PCR nasopharyngeal swab, which was negative in all cases.
A total of 125 patients were included in the "pre-COVID" period, 68 males (54.4%) and 57 females (45.6%), with a mean age of 4.58 years.
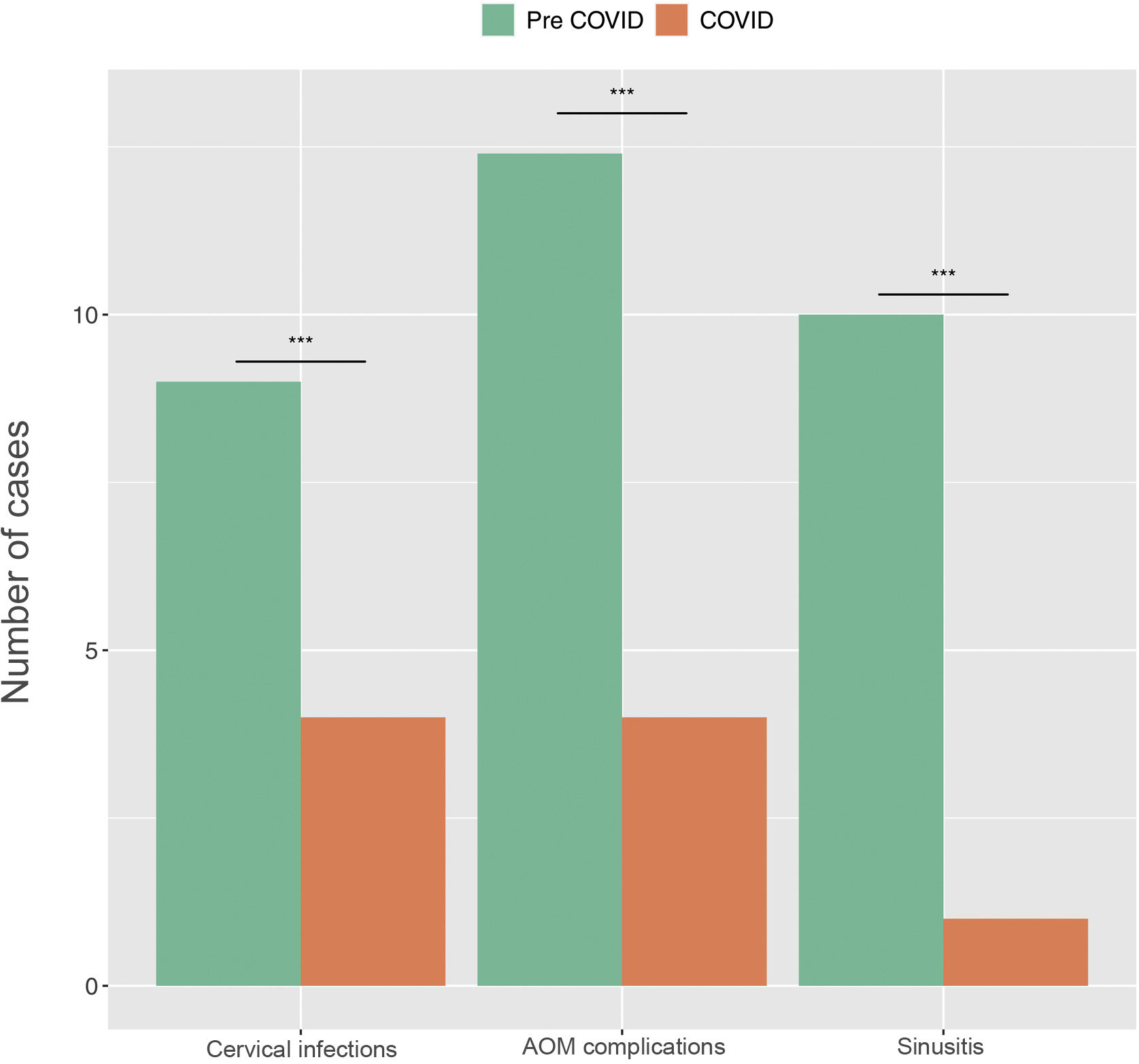
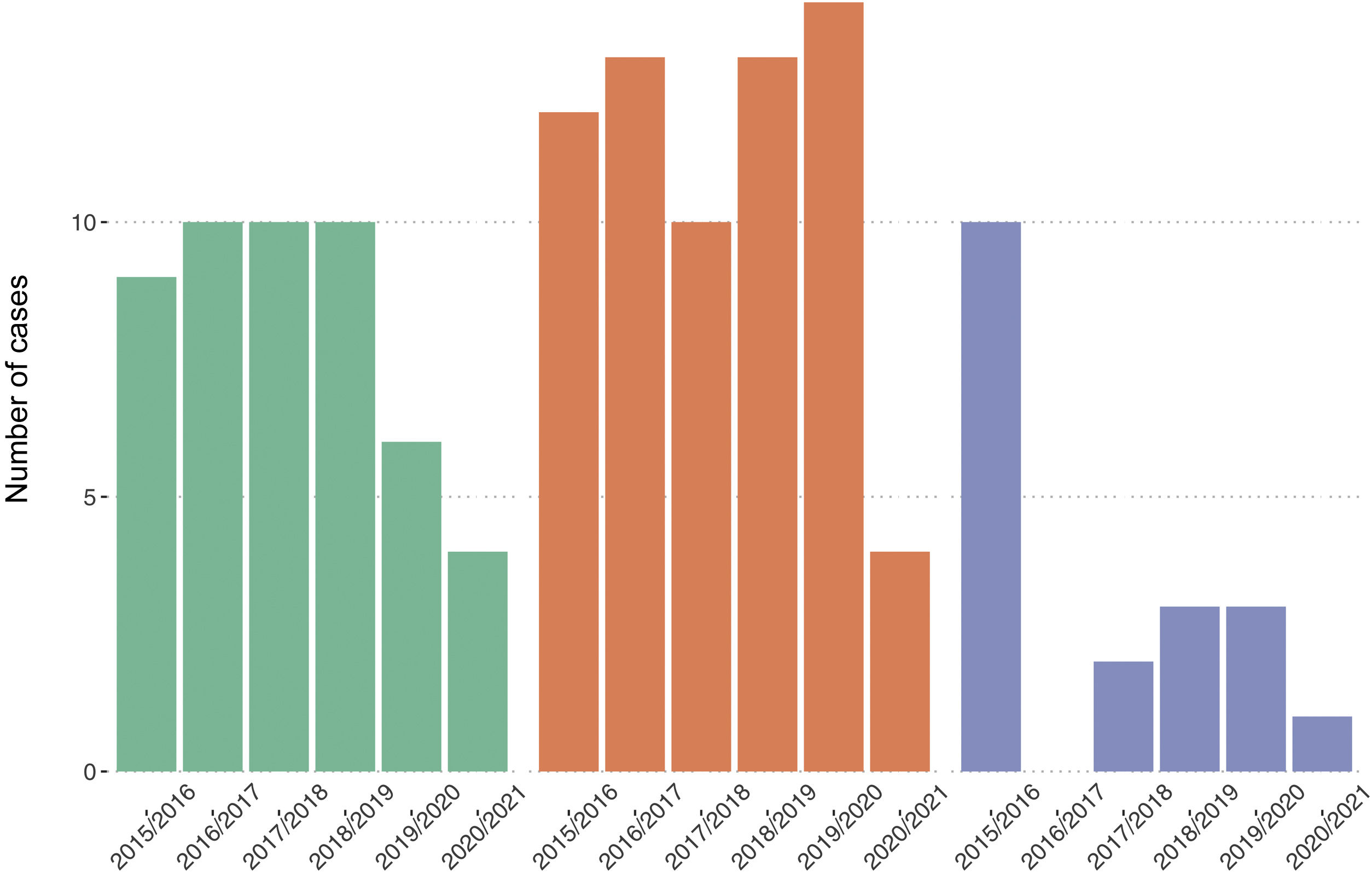
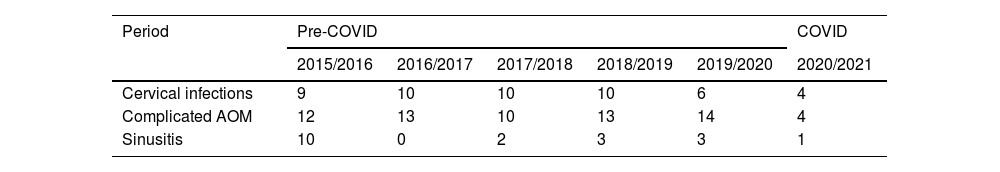
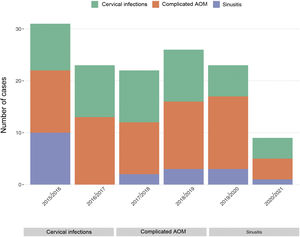
In the "COVID" period we found 4 admissions for cervical infections, 4 for complicated AOM, and 1 for complicated acute sinusitis (Fig. 1). In the "pre-COVID" period we found 45 admissions for cervical infections, 62 for complicated AOM, and 18 for complicated acute sinusitis (Fig. 1).
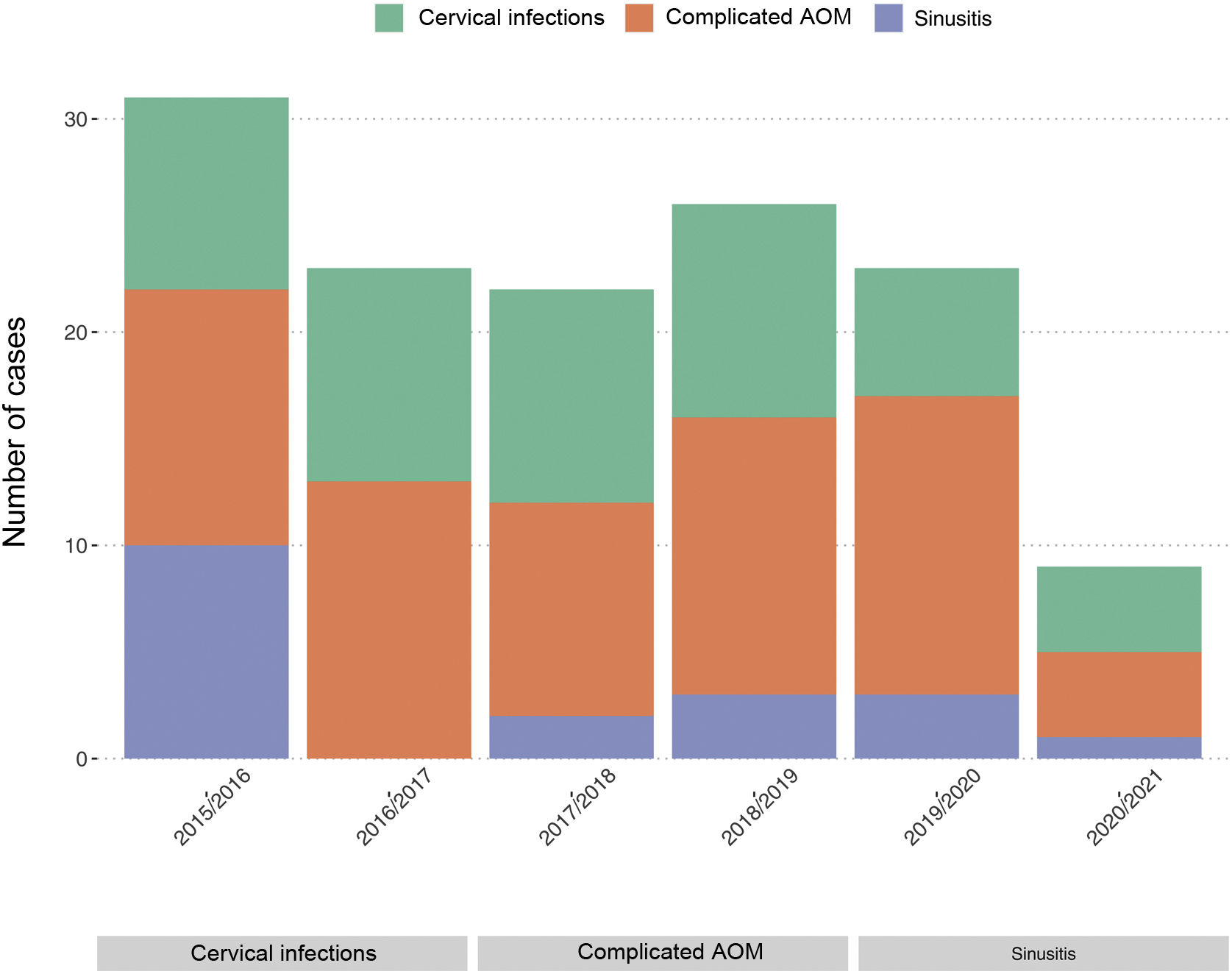
Table 2 shows the number of admissions distributed by group in the 6 periods studied. No readmissions were recorded in any of the periods.
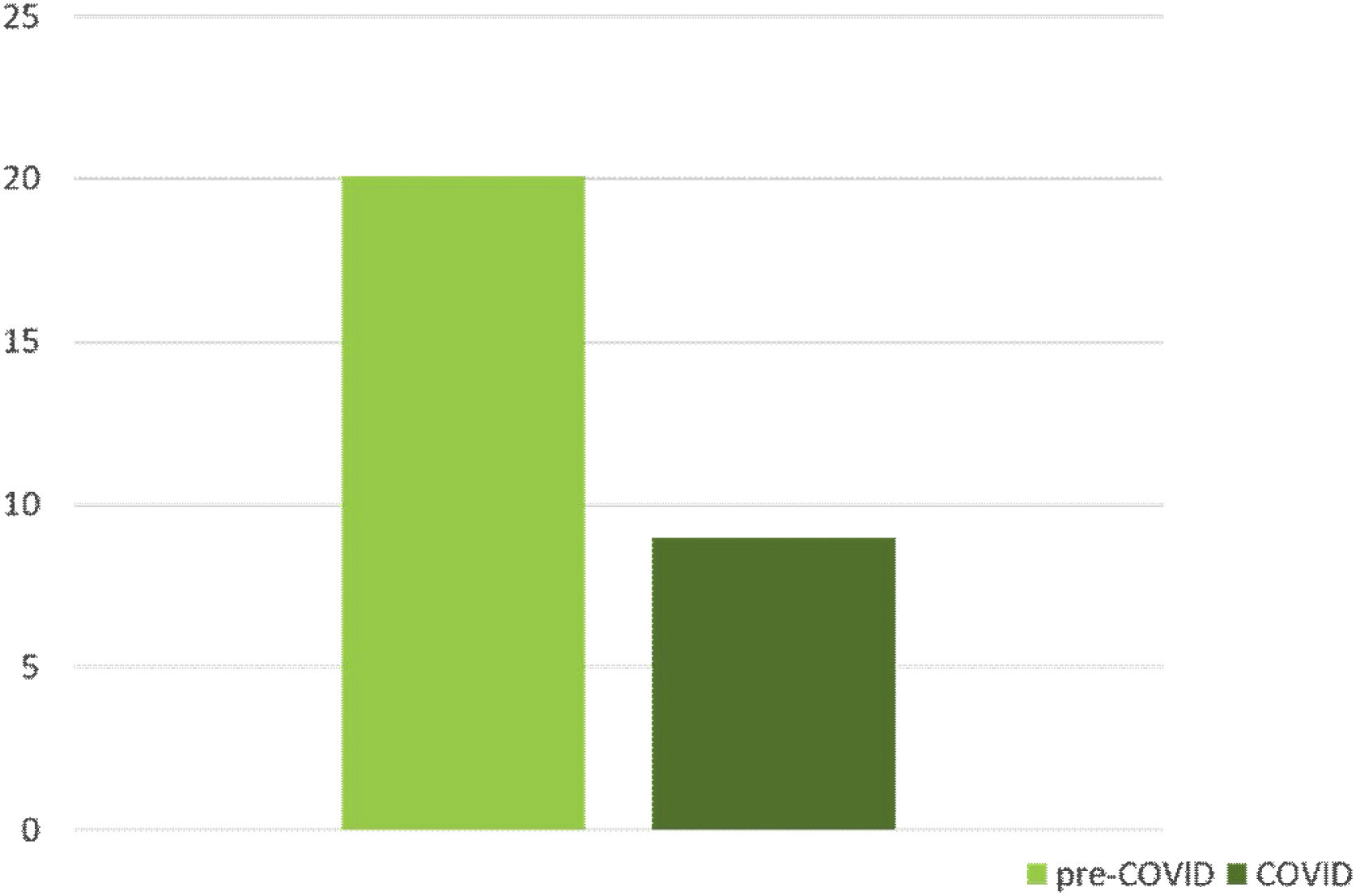
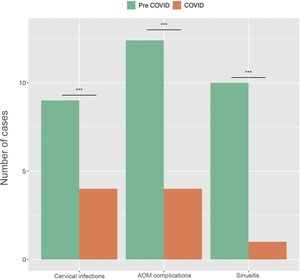
When we compared the total number of admissions in both periods, we found that in the "COVID" period there are a total of 9 admissions and in the pre-COVID period there are a total of 125 admissions (Fig. 2), the annual average being 20.1 admissions, which is a relevant decrease in the total number of infections.
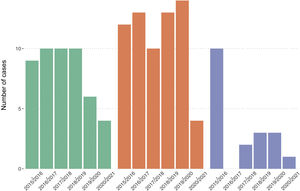
The number of admissions per annual period in each group within the "pre-COVID" period was analysed for any notable annual differences (Figs. 3 and 4). In the case of cervical infections and AOM complications, (Fig. 4) there is no significant annual variation in the number of admissions in the pre-COVID period. However, there was in the group of sinusitis complications (Fig. 4), with 10 admissions in some years and 0 in others. Therefore, the average number of admissions per year in the "pre-COVID" period was established as a parameter for comparison with the number of cases in the "COVID" period.
Comparing by groups we observe that in the COVID period there were a total of 4 admissions for cervical infections, compared to an annual average of 9 admissions in the "pre-COVID" period, and there are statistically significant differences between the two periods (p-value=.027 (<.05).
The same is true for AOM complications. There were 4 admissions for this reason during the "COVID" period, and an annual average of 12.4 admissions during the "pre-COVID" period, finding a statistically significant difference (p-value=.029 (<.05))
Finally, in the sinusitis group, there was 1 admission during the “COVID” period, and an annual average of 12.4 admissions during the “pre-COVID” period, no statistically significant difference was found (p-value=.067 (>.05)) which could be due to the inter-annual variability of the period studied, although from a clinical point of view the difference between 1 and 3.6 has a clearly significant value.
DiscussionThe effect of lockdown was a decrease in the number of consultations in paediatric emergency departments in different countries around the world.2–4 The total number of consultations decreased but the number of infectious diseases decreased more markedly than others.4 Different hypotheses have been proposed in this respect, such as: decreased contact between children and, therefore, a decrease in the contagion of infectious-contagious diseases; fear of going to health centres due to the possibility of becoming infected there,5 the desire not to increase demand in a health system already saturated by the pandemic, and less pressure on parents for work-related reasons, since teleworking took precedence over this period.2 This was also observed in Spain,6 with a decrease in the demand for urgent paediatric care over the period of lockdown.
In addition to the above, the lockdown also had a beneficial effect on other ENT diseases such as serous otitis media and tonsillar hypertrophy.7–9 Studies conducted over the lockdown period have shown a reduction in the prevalence of serous otitis media and an increase in the resolution of chronic conditions.7,9 In the case of tonsillar hypertrophy, Gelardi et al. demonstrated a reduction in associated symptoms and pathology.8
There is evidence in the literature10 that school closures can have a substantial impact on the spread of an emerging infectious disease that is transmitted through close contact. Heymann et al.11 found in their study a reduction in the number of diagnoses of respiratory infections and a decrease in medical consultations with school closures. Therefore, school closure measures during the pandemic reduced the spread of SARS-COV-2 but also influenced the spread of other infectious diseases, as was the case in our study population.
The results of our study show that the measures used to slow the progression of the COVID-19 pandemic resulted in a decrease in the number of hospital admissions of paediatric patients for complications of infectious diseases in the ENT area; both in the overall number of admissions and in complications of acute otitis media and deep cervical infections. In this regard, although it is true that emergency department consultations decreased in general, it is to be expected that practically all patients presenting with ENT infectious pathology with poor progression and susceptible to hospital admission would request assessment in the emergency department. Therefore, we consider it unlikely that the number of admissions has been substantially modified by the reduction in emergency consultations. The decrease in admissions for ENT infectious complications is probably due to an overall decrease in the number of ENT infections in paediatric patients.
Because we studied a 12-month period that includes months of lockdown and months with the opening of schools and recovery of normal activity, we argue that the observed effect on the decrease in cases is not solely due to the period of lockdown. Nor can it be attributed exclusively to the closure of schools, as there was no substantial increase in admissions with their opening.
Several studies have demonstrated the efficacy of the use of surgical or FPP2 masks in reducing aerosol-borne infections,12,13 including upper airway infections, the main cause of the complications analysed in our study. Furthermore, hand washing has been shown throughout the history of medicine to be a cost-effective measure in the control of infectious diseases.14,15 When we differentiate between possible hygiene measures, we find that the use of masks is essential for the reduction of respiratory infections transmitted by aerosols,4,13,16 Seto et al. demonstrate that both hand washing and the use of masks prevent contagion; however, the use of masks alone is the only measure that has proven useful in the hospital setting.12 Another study observes that both measures together are useful in enterovirus transmission but when the effect of hand washing is analysed in isolation, its contribution to the prevention of transmission is small.16 Chiu et al. show that the use of masks, hand washing, and social distancing are useful measures for reducing COVID-19 transmission but also contributed to reducing the incidence of other viruses such as influenza, enterovirus, and pneumonia,4 however, the individual effects of each measure are not known and their causal relationship should be studied in further studies.
In our study, we did not analyse separately the different measures adopted to curb infection, therefore we cannot know which measure has the greatest impact on reducing infections in our setting. In the literature we found studies focusing on periods of lockdown, where they observed a reduction in visits to the emergency department for infectious diseases.2,3 However as we did not study longer periods we cannot evaluate the isolated effect of other prevention measures. Mathematical models have been used to assess the effect of lockdown, school closures and social distancing in the work environment and the result is that all three measures together provide greater protection, but they cannot determine which of the three measures is more effective when used individually.17
In contrast to the findings of our study, Enrique et al. observed an increase in the incidence of complicated mastoiditis and deep cervical infections with complications during 2020. However, the number of patients hospitalised for ENT infections did not vary significantly from previous years.18
A possible limitation of the study was not to divide the period into sub-periods, analysing lockdown or school closures separately compared to the rest of the year. However, this subdivision was not possible due to the small number of admissions over the period under study. To overcome this limitation, in future studies, multi-centre analyses could be conducted to increase the sample. They would also be useful to determine whether the results obtained occurred exclusively in our setting or whether they can be extrapolated to the Spanish population.
ConclusionA decrease in the number of admissions caused by complications of ENT infections in paediatric patients was observed after the onset of the COVID-19 pandemic in our setting. This could be explained by an overall decrease in the number of upper respiratory tract infections due to the hygienic measures taken due to the COVID-19 pandemic, such as hand hygiene, the use of masks, or social distancing. Likewise, these results open the discussion as to whether in other periods of respiratory infectious disease epidemics generated by other viruses it would be useful to use masks for limited periods of time and in limited places.
FundingThis research study received no specific support from public sector agencies, commercial sector or not-for-profit organisations.
Conflict of interestThe authors have no conflict of interests to declare.