Vacunas COVID-19: desarrollo y práctica - COVID-19 vaccines: development and practice
Más datosCOVID-19 is a serious public health problem. Therefore, it is important to vaccinate the community. This study was aimed at examining the reasons for individuals' COVID-19 vaccine hesitations, and decisions that have changed over time.
Material and methodsThis was a prospective longitudinal qualitative study.
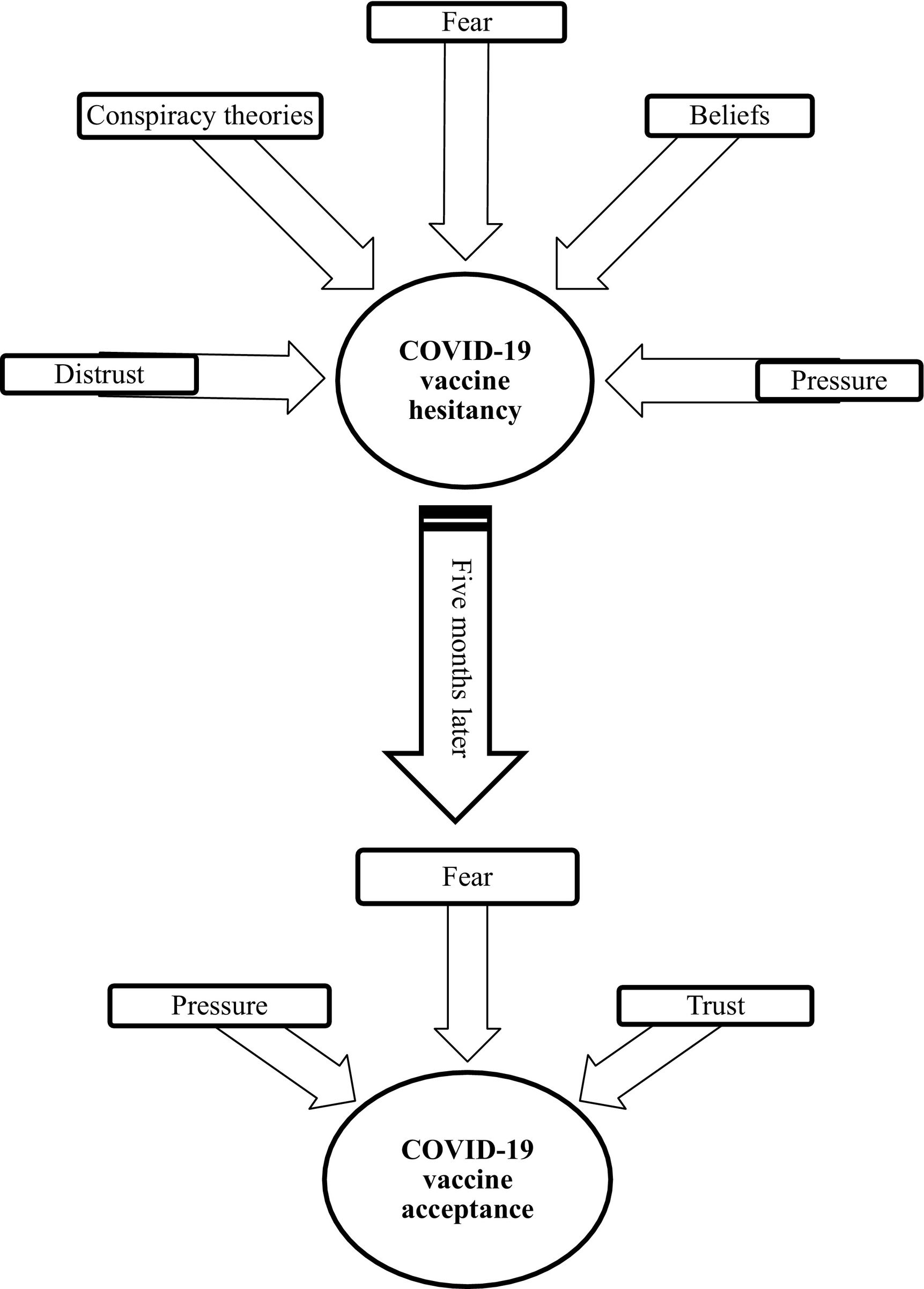
ResultsConfidence, fear, conspiracy theories, belief, and social pressure play a role in vaccine hesitancy. The most important factor in the changing decisions of individuals who are hesitant about vaccination is pressure. Confidence and fear also lead to a change of decision. However, it was remarkable that most of the participants who were vaccinated due to pressure did not want to be revaccinated.
ConclusionsGovernments, media, vaccine companies, health professionals, and scientists should act together to increase the vaccination rates of individuals.
El COVID-19 es un grave problema de salud pública. Por lo tanto, es importante vacunar a la comunidad. Este estudio tuvo como objetivo examinar las razones de las dudas y decisiones de las personas sobre la vacuna COVID-19 que han cambiado con el tiempo.
Material y métodosSe trata de un estudio cualitativo longitudinal prospectivo.
ResultadosLa confianza, el miedo, las teorías de conspiración, la creencia y la opresión jugaron un papel en la vacilación de la vacuna. El factor más importante en las decisiones cambiantes de las personas que dudan acerca de la vacunación ha sido la opresión. La confianza y el miedo también llevaron a un cambio de decisión. Sin embargo, fue notable que la mayoría de los participantes que fueron vacunados debido a la opresión no querían ser revacunados.
ConclusionesLos gobiernos, los medios de comunicación, las empresas de vacunas, los profesionales de la salud y los científicos deben actuar juntos para aumentar las tasas de vacunación de las personas.
The cases of COVID-19 detected since the day it appeared and the death rates due to this have reached high levels.1 The World Health Organization (WHO) announced that the total number of cases detected globally by February 21, 2022 was 423.4 million, and the total number of deaths was approximately 5.8 million.1 Many vaccine studies have been conducted to control case and death rates. The WHO has emphasized the importance of these vaccines and vaccination in order to control the pandemic.2 However, the number of fully vaccinated people globally was stated to be approximately 4.2 billion as of February 21, 2022.1
One of the most important reasons why the vaccination rates are not at the desired level is that individuals do not get vaccinated voluntarily.3–6 The reasons for individuals not wanting to be vaccinated are thinking that the COVID-19 outbreak is exaggerated, mistrusting vaccines, lacking knowledge about vaccine efficacy, needing further explanation, and being suspicious of conspiracy theories, country of origin of vaccines, and side effects. There are quantitative and qualitative studies on this topic4,5,7,9, but little is known about how the decisions of individuals with vaccine hesitancy change over time.10,11 Therefore, the aim of this study was to examine the reasons for individuals' COVID-19 vaccine hesitations and decisions that have changed over time.
Materials and methodsDesignThis study is based on prospective longitudinal qualitative study methodology. Longitudinal qualitative methodology focuses on understanding behavior change over time. It is often used to understand changes in health behavior. In this methodology, data are collected by conducting 2 or more sessions that involve a qualitative data collection method.12
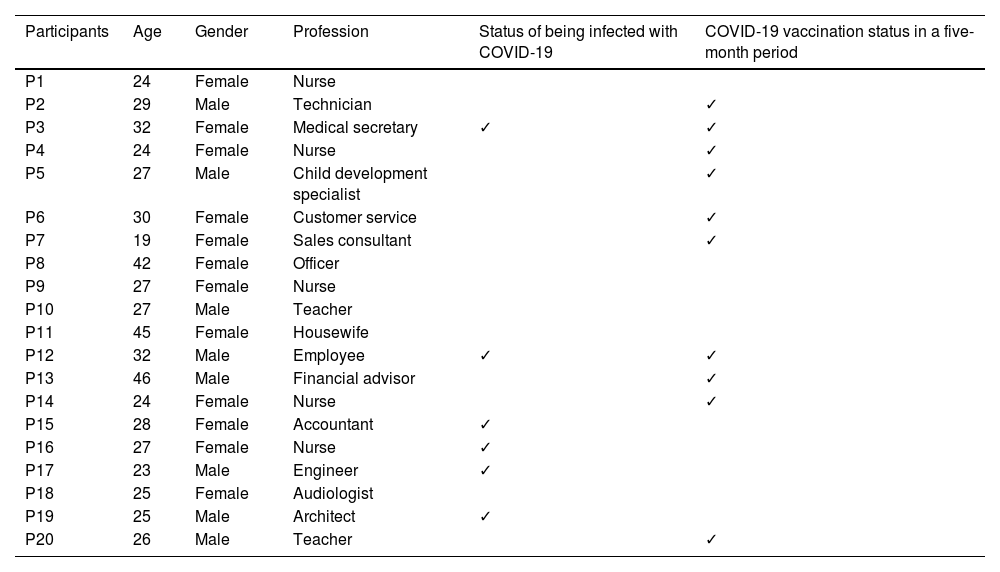
Recruitment and samplingThe individuals included in this study were aged 18 and over, not vaccinated against COVID-19 and non-hearing impaired. The individuals were accessed by snowball sampling. The first interviews were conducted in October and November 2021 and were completed with 20 participants. Five months after the initial interviews, the participants were asked whether they had been vaccinated. The second interviews were conducted in February 2022 with the vaccinated participants, and completed with 11 participants. Sample size was as recommended in the literature about qualitative research13,14, and interviews were continued until no new information was obtained.
Data collectionData were collected through semi-structured interviews. Three forms were used for data collection: a Participants Information Form, Semi-Structured Interview Form-1, and Semi-Structured Interview Form-2. The Participant's Information Form composed of questions about about sociodemographic characteristics such as age and income. Semi-Structured Interview Form-1 included the questions “What do you think about the COVID-19 vaccines?” and “What are your reasons for not wanting to get vaccinated?”. Semi-Structured Interview Form-2 included the questions, “Why did you decide to get vaccinated?” and “What changed your decision?” The individuals who were accessed were informed about the aim of the study, voice-recording of interviews, and confidentiality of obtained data. They were assured that participation in the study was voluntary and that they could leave the study whenever they wanted. Individuals who agreed to participate in the study were informed again after the beginning of the audio recordings and their consent was obtained. Voice recordings and transcriptions were kept on password-protected computer files. The interviews lasted between 20 and 48 min.
AnalysisContent analysis was used for data analysis as described by Graneheim and Lundman. Voice recordings of the interviews were transcribed verbatim and documented. The data were analyzed independently by 2 researchers, then the code and the differences in the categories were compared, and the final themes and categories were created.15 The participants were assigned numbers in the form of P1, P2,… P20 in the documents to keep their identities confidential.
ResultsParticipants' demographic characteristicsThe mean age of the participants was 28.6 ± 7.53, and 55% of the participants were vaccinated within 5 months after the first interview (Table 1).
Participants characteristic
| Participants | Age | Gender | Profession | Status of being infected with COVID-19 | COVID-19 vaccination status in a five-month period |
|---|---|---|---|---|---|
| P1 | 24 | Female | Nurse | ||
| P2 | 29 | Male | Technician | ✓ | |
| P3 | 32 | Female | Medical secretary | ✓ | ✓ |
| P4 | 24 | Female | Nurse | ✓ | |
| P5 | 27 | Male | Child development specialist | ✓ | |
| P6 | 30 | Female | Customer service | ✓ | |
| P7 | 19 | Female | Sales consultant | ✓ | |
| P8 | 42 | Female | Officer | ||
| P9 | 27 | Female | Nurse | ||
| P10 | 27 | Male | Teacher | ||
| P11 | 45 | Female | Housewife | ||
| P12 | 32 | Male | Employee | ✓ | ✓ |
| P13 | 46 | Male | Financial advisor | ✓ | |
| P14 | 24 | Female | Nurse | ✓ | |
| P15 | 28 | Female | Accountant | ✓ | |
| P16 | 27 | Female | Nurse | ✓ | |
| P17 | 23 | Male | Engineer | ✓ | |
| P18 | 25 | Female | Audiologist | ||
| P19 | 25 | Male | Architect | ✓ | |
| P20 | 26 | Male | Teacher | ✓ |
✓: Yes.
In the interviews, the causes of vaccine hesitancy of individuals were collected under 5 main themes. These were distrust/trust, conspiracy theories, fear, beliefs, and pressure (Fig. 1).
Distrust/TrustIn the first interviews, all participants reported that the main reason for not wanting to be vaccinated was the lack of confidence in vaccines. Participants stated that inadequate, inconsistent, biased, and insistent statements about vaccines in the media created distrust. It has been seen that the negative information and news especially in the social media, are effective in creating mistrust towards the vaccine. “A doctor comes out and says something. Another doctor says the opposite. In fact, according to the news presented to us, vaccination is a good thing, but the situation is very different in the social media part of the work, in the part of those who are not talked about… So that's why it's not reliable.” (P17).
Nearly half of the participants stated that they did not have confidence because the vaccines were produced quickly and not all phase studies were completed, and people were used as test subjects. “I think I am a mouse subjected to this forced experiment. That's why I want to escape from this lab.” (P9).
Almost half of the participants said that having to sign a consent form before getting vaccinated lowered their trust in the vaccine. “A document is presented to you and you are requested to sign it because you are asked to take full responsibility for the vaccine, including death. They already say there, this vaccine is not reliable, anything can happen to you.” (P16).
Another reason for distrust among the participants was stated as not knowing the contents of the vaccines. “What is in the vaccine, how was it produced? There is uncertainty regarding these.” (P10).
Some participants stated that they could only rely on the national vaccine because they thought that only the national vaccine would not harm them. For this reason, they waited for the Turkish vaccine to come out to be vaccinated. “The Turkish vaccine makes more sense to me. I don't think our country wants to cause any permanent damage or harm to its own citizens.” (P5).
Trust in the national vaccine has been effective in changing the vaccine decision positively. One participant who had been vaccinated before due to pressure stated that would get the Turkish vaccine when he was revaccinated because he trusted the national vaccine. “The Turkish vaccine is out. When I get revaccination, I'm thinking of getting the Turkish vaccine. Not that I know anything, but I trust the Turkish vaccine.” (P2).
One participant, who had been vaccinated before due to pressure, stated that she would not be revaccinated because she did not know its contents. “Why would I be revaccinated right now? Why? Are they reinjecting the same thing? I don't know what that is.” (P14).
In the first interviews, some participants mentioned conspiracy theories about biological warfare (such as population reduction policy, genetic modification, collection of personal data) or economic warfare (such as the idea that there is an artificial virus and a vaccine made in the laboratory to make money) as reasons for vaccine hesitation. “I think that there is no war with guns and rifles any more, war has started in a more scientific direction, and guns and rifles are things that will do harm like viruses and cause complete massacre.” (P9).
In the formation of conspiracy theories, the news about the drugs remembered in the media due to their side effects and the news that there were studies showing that people's personal data were accessed without their knowledge had an effect. “There are cases where children were born without legs, hands or arms due to a newly released pill used by pregnant women in the past.” (P4).
In the first interviews, almost all of the participants stated that they did not want to be vaccinated because they were afraid of the side effects of the vaccine. The most frequently feared side effects were the vaccine causing death and infertility, damaging the heart muscle and brain, and infecting the person with COVID-19. The fear of infertility was mostly expressed by people who were young and had not yet had children. “I fear it will damage the spinal cord, brain or some part of the body.” (P11).
The basis of the participants' fears arising from side effects was the unknown long-term side effects of the vaccine and hearing negative stories about its side effects. “A young friend of ours lost his wife. The expressions he used were as follows: My wife is not a person who has been to the hospital before or even taken painkillers. After the COVID-19 vaccine, my wife had arm pain for two days, then severe chest pain and died of a heart attack. He said things like that.” (P17).
In the second interviews, the fear of being infected with COVID-19 and infecting others due to the increase in the number of COVID-19 cases led to acceptance of the vaccine. “The number of unvaccinated patients in intensive care began to increase. Almost no patients are vaccinated. The number of cases started to increase too. I saw these, I got scared, I got vaccinated.” (P4).
“There are a lot of old people in my family and I always together with them. I afraid of harming them. That's one reason why I'm vaccinated.” (P7).
BeliefsIn the first interviews, it seemed that beliefs had an important place in the vaccine hesitancy of the participants. The belief that COVID-19 was exaggerated, that the vaccine was not protective, and that people's bodies become immune over time led to vaccine hesitancy. “Despite three doses of vaccine, the wife of one of my closest friends caught it…. If this vaccine isn't going to protect us, why are we getting vaccinated? Why would I want to be vaccinated?” (P12).
In the second interviews, it was revealed that belief was an obstacle to revaccination. This belief was that the vaccine was not protective. “I don't plan on getting revaccinated. Because I don't think the vaccine is protective. In order for revaccination, they need to show my immunity before and after the vaccination.” (P14).
Most of the participants stated that they were uncomfortable with the social and political pressure on them. Some participants stated that pressure creates resistance to being vaccinated. “Everyone around me is actually putting pressure on me. They say “Haven't you been vaccinated yet?” (P3).
One participant stated that the hospital administration pressured her to be vaccinated and that she was not vaccinated in response to this pressure: “When we told you to test the patients you sent and send them like that or do antibody tests, none of you did. Now you are telling me to get vaccinated. Did you do what I wanted now I will do what you want?” (P1).
Although pressure has created resistance to the vaccine in some people, it has enabled some people who had not been vaccinated before to be vaccinated. This pressure was exerted by society, the workplace, and family members who had been vaccinated. “I got vaccinated because of pressure. The bosses of big workplaces said that those who were not vaccinated should find a new job, so I had to.” (P20). “Those who are vaccinated force those who are not vaccinated to get vaccinated. They are even insulting. The person feels bad and alienated. That's why I got vaccinated.” (P2).
“I went to the mall with my wife. They were vaccinating there. My wife forcibly took me there. I was vaccinated because of her pressure.” (P12).
One participant said that when she got vaccinated, she felt relieved of pressure. “They were constantly asked who had not been vaccinated. This was nerve-wracking. I have completed both doses and have felt relieved of pressure.” (P14).
Some participants who were vaccinated due to pressure stated that being vaccinated made them feel bad. “I felt bad while I was getting vaccinated because I didn't want to be vaccinated.” (P7).
Participants who were vaccinated under pressure stated that they would not be vaccinated again or would be vaccinated if they were forced. “At work, they asked if I had been vaccinated again. I made an excuse. I will not get revaccinated.” (P12).
In this study, it was determined that the feeling of trust is important in vaccine hesitancy and acceptance. In the first interviews, it was found that the country of origin of the vaccine, its content not being known, rapid production and incomplete phase studies, insufficient, inconsistent, biased and insistent statements about vaccines, the thought that people are used as experimental subjects, and especially negative news and information on social media had affected the formation of mistrust against the vaccine. In previous studies also, it has been reported that insecurity affects the formation of hesitation about getting a COVID-19 vaccine.4,9,16,17–19 In this study unlike in previous studies, it was shown that signing the pre-vaccination informed consent form affects vaccine hesitancy. The participants thought that the informed consent form was requested because it was not reliable. In the second interviews, it was determined that the trust in the national vaccine affected revaccination. This result revealed that a sense of trust can be created in an individual who is hesitant about vaccination. For this reason, clear and consistent explanations about vaccines by experts, especially through the media, and providing sufficient information to individuals before informed consent by healthcare personnel can increase individuals' confidence in being vaccinated and thus their willingness to be vaccinated.
Conspiracy theories are a factor that reduces vaccine willingness.8 It is known that as the belief in conspiracy theories increases, people's intention to be vaccinated decreases.5 One study revealed that it was thought that the vaccine had been around for a long time, but it had been kept secret by pharmaceutical companies.6 Even though previous studies carried out by the quantitative method have for this reason brought a certain amount of clarity to conspiracy theories, they limit the understanding of the real reasons and the emergence of different thoughts. In this study, which was conducted using a qualitative method, it was seen that conspiracy theories were one of the reasons for vaccine reluctance. Unlike previous studies, in this study conspiracy theories and their causes have been explained better. It has been revealed that some individuals think of the vaccine as a product of economic warfare (the idea of a virus and vaccine developed in a lab for financial gain) and/or biological warfare (population reduction policies, genetic modification, collection of personal data, etc.). News in the media regarding pharmaceuticals that were recalled owing to negative effects in the past, as well as news that studies were undertaken in which individuals' personal data was obtained without their knowledge, were major factors that strengthen people's belief in conspiracy theories.
Studies have shown that fear of side effects affects vaccine willingness.9,11,20–22 In the first interviews of this study, it was determined that fears of side effects (death, getting COVID, infertility, etc.) were an important reason for hesitation in being vaccinated. In addition, unlike previous studies, it was seen that the negative stories about the side effects of the vaccine and the fact that the long-term side effects of the vaccine were not known fed these fears. In the second interviews, catching COVID-19 due to increasing case rates and fear of infecting relatives with COVID-19 caused vaccine acceptance. When the reasons for accepting vaccines of the participants who were vaccinated due to fear between the two interviews were examined, the importance of explaining the effects of COVID-19 and presenting the case rates to the public became evident. Although fear was an unwanted emotion, it was a triggering emotion to be protected from a serious infectious disease. It was thought that the participants experienced a sense of dread as they realized the seriousness of COVID-19.
In this study, it was determined that beliefs affected vaccination. The fact that those who were already vaccinated in the first interviews also became sick and that the virus had mutated negatively affected the belief in the protection of the vaccine. Some participants did not want to be vaccinated because they believed that they had acquired natural immunity. In previous studies, it was determined that negative beliefs about the protection and efficacy of the vaccine were among the reasons for hesitation in getting the vaccine.4,23 In the second interviews, it was revealed that belief did not cause vaccine acceptance, but continued to cause vaccine hesitancy.
In this study, unlike previous studies, it was determined that social and political pressure to have the vaccination negatively affected people who did not want to be vaccinated, and some individuals resisted vaccination in response to pressure. However, in the second interviews, it was determined that over time, workplace, social, and family pressure caused vaccine acceptance. The fact that the individuals who have been vaccinated due to pressure do not want to be revaccinated shows that the pressure should be eliminated. In order for these participants to be revaccinated, pressure needs to be removed and persuasion used.
ConclusionIt was revealed that distrust of vaccines, belief in conspiracy theories, fears of side effects, negative beliefs about Covid-19 vaccines, and pressure create reluctance to be vaccinated. Governments, media, vaccine companies, health professionals, and scientists should act together to increase the vaccination rates of individuals. Although pressure positively affected the decision of some people to be vaccinated over time, it was revealed that people who were vaccinated due to pressure did not want to be vaccinated again. The belief that the vaccine is not protective was an obstacle for people to be revaccinated.
Declarations of InterestEthical approval was obtained from the COVID-19 Research Evaluation Committee of the Turkish Ministry of Health and the Medical Ethics Committee of a university in the western part of Turkey (E-60116787-020-113,991). This study was conducted in accordance with the Declaration of Helsinki.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statementDicle Filiz Yıldırım: Conceptualization, Methodology, Formal analysis, Investigation, Visualization, Writing – original draft. Pınar Serçekuş: Conceptualization, Methodology, Formal analysis, Writing – review & editing. Sevgi Özkan: Writing – review & editing.