To demonstrate the effect of acupuncture on the Hypertension Groove (HG) auricular acupoint located in both the left and right ear on pulse transit time (PTT) in healthy subjects.
DesignA cross-sectional experimental study.
SettingClínica de Acupuntura, Unidad Iztapalapa, Universidad Autónoma Metropolitana, Ciudad de México, México.
ParticipantsThirty healthy university students aged 26.4±4.9 years (mean±SD).
InterventionsThe study consisted of two sessions of auricular acupuncture in the HG acupoint: first, in the right ear, and after seven days of washout period, in the left ear.
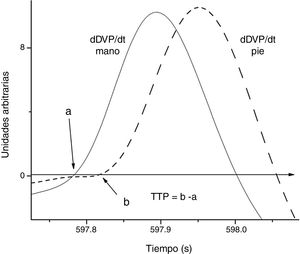
Main measurementsDigital volume pulse (DVP) was recorded by photoplethysmography simultaneously in the hand and toe in each subject. PTT was estimated as the difference between the beginning of the DVP in the index finger of the hand and the second toe. The HG auricular acupoints in either ear were stimulated by manual acupuncture. PTT was calculated for basal and post-acupuncture conditions.
ResultsThe PTT was significantly increased by acupuncture in HG in both ears when comparing the pre- and post-acupuncture values. In the total sample, the Pearson correlation coefficients between basal values of PTT and the differences elicited through auriculopuncture showed a non-significantly positive correlation for the right ear, and significantly negative for the left ear.
ConclusionsResults indicate that each one of HG auricular acupoints has differentiated effects on the PTT of healthy subjects. Moreover, the effect of this acupoint depends on the basal state of PTT.
Demostrar el efecto de la acupuntura en el punto auricular Surco Hipertensor (HG), localizado tanto en la oreja izquierda o derecha, sobre el tiempo de tránsito de pulso (PTT) en sujetos sanos.
DiseñoEstudio experimental transversal.
CentroClínica de Acupuntura, Unidad Iztapalapa, Universidad Autónoma Metropolitana, Ciudad de México, México.
ParticipantesTreinta estudiantes universitarios sanos con edades de 26,4±4,9 años (media±DE).
IntervencionesEl estudio consistió en dos sesiones de acupuntura auricular en el punto HG: primeramente en la oreja derecha y, tras siete días de periodo de periodo de lavado, en la oreja derecha.
Principales medidasSe registró el pulso de volumen digital (DVP) mediante fotopletismografía simultáneamente en la mano y pie de cada sujeto. Se calculó PTT como la diferencia entre el inicio del DVP en el dedo índice de la mano y el segundo dedo del pie. Se estimularon los acupuntos auriculares HG en cada oreja mediante acupuntura manual. Dicho PTT se calculó para condiciones basales y post-acupuntura.
ResultadosEl PTT incrementó significativamente mediante acupuntura en HG en ambas orejas, al comparar los valores pre y post-acupuntura. En la muestra total, los coeficientes de correlación de Pearson entre los valores basales de PTT y las diferencias obtenidas reflejaron una correlación positiva no significativa para la oreja derecha, y negativa significativa para la izquierda.
ConclusionesLos resultados indican que cada uno de los puntos auriculares HG tiene efectos diferenciados en el PTT de los sujetos sanos. Además, el efecto de este punto depende del estado basal de PTT.
Arterial stiffness seemed to be present in subjects with abnormal circadian patterns and young hypertensives.1 Stiffness of large arteries has emerged as an independent predictor of cardiovascular risk.2 Photoplethysmography (PPG) is the measurement of the changes in tissue light absorption, which originates from the cardiac-induced blood volume changes in the small arteries in the tissue. The PPG yields a low-noise signal, which enables accurate determination of its minimum, i.e., the arrival time of pressure pulse. Two PPG probes along two sites in an artery let to calculate the PTT consequently assess the pulse wave velocity along the arterial system.3 Therefore, PTT is a reliable noninvasive method for the experimental assessment of arterial stiffness.4,5
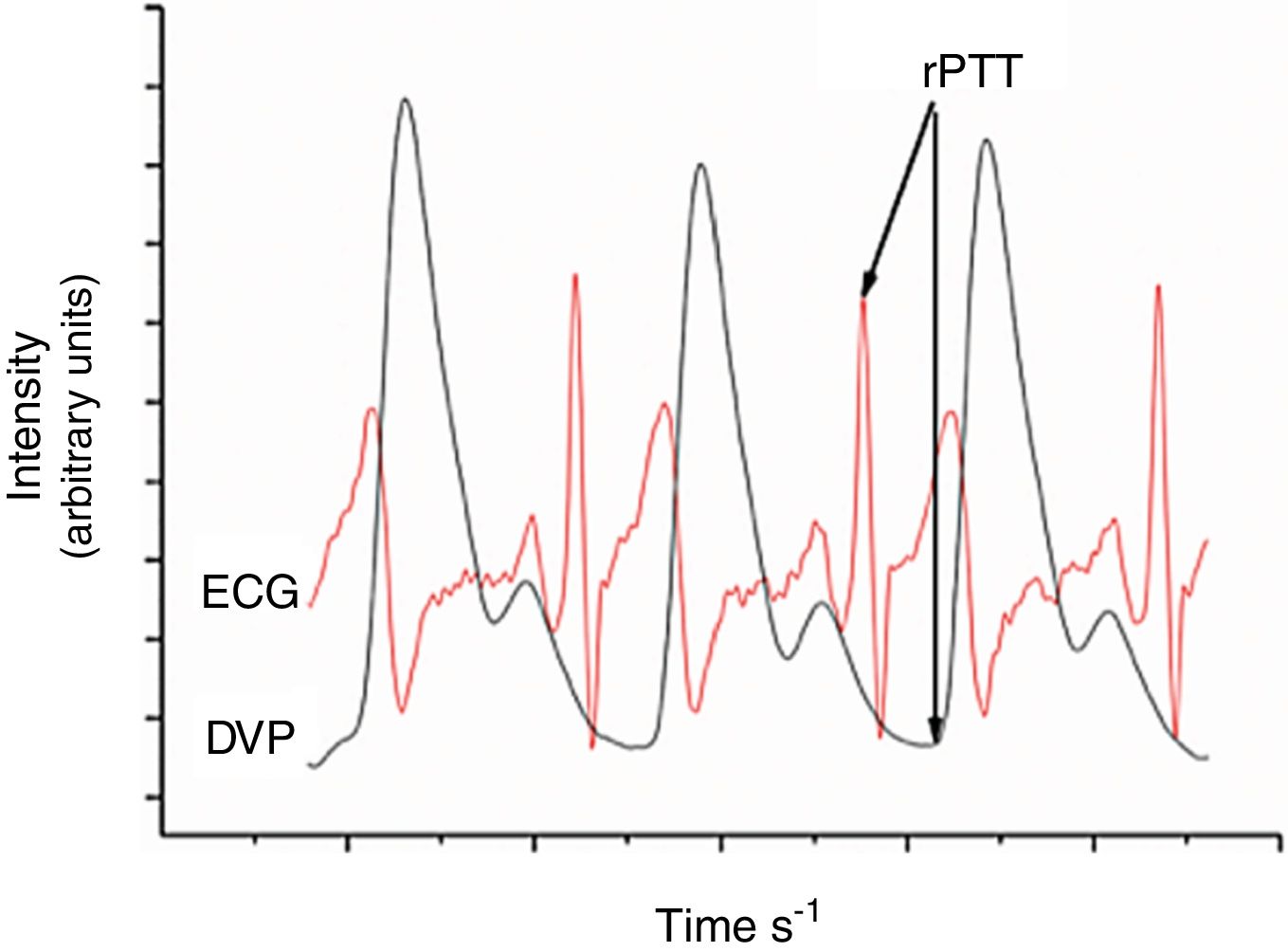
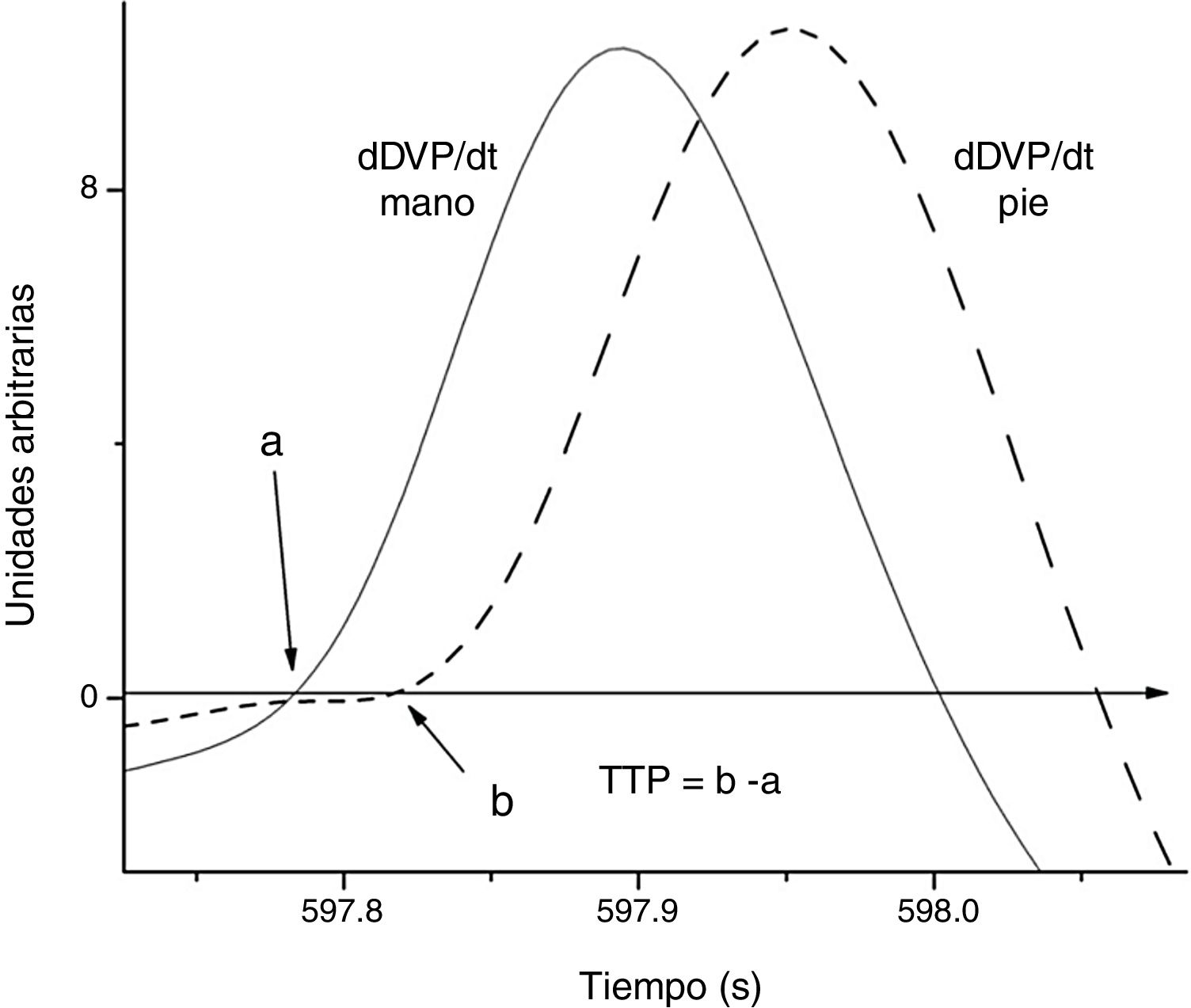
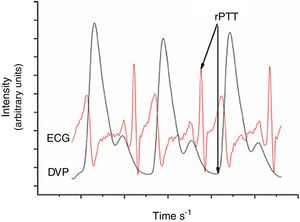
Pulse transit time. Two non-invasive methods are commonly used for the assessment of pulse transit time or pulse wave velocity. The rPTT is the interval between the R wave of the electrocardiogram (ECG) and the appearance or peak of the pulse wave of the same cardiac cycle measured at some peripheral vascular site,6,7 see Figure 1. The use of rTTP allows a more straightforward PTT measurement, but it has the disadvantage of having several variables. For example, rPTT involves the delay between the start of the R wave and the opening of the aortic valve (isometric contraction interval), besides the interval necessary for the pulse wave to travel from the aortic valve to the periphery, which is actual PTT.8 Besides, the isometric contraction is influenced by variables that modify the PTT such as blood pressure, ventricular volume ejection, and changes in intrathoracic pressure.9,10
The pPTT, from now on referred to as PTT, is the interval between the arrival at two distal anatomical sites of the same wave of the pulse volume. Consequently, PTT reflects the velocity of propagation of the arterial wave between the two sites.11 The PTT lets a more precise assessment of arterial stiffness;12 therefore, it was used in this study.
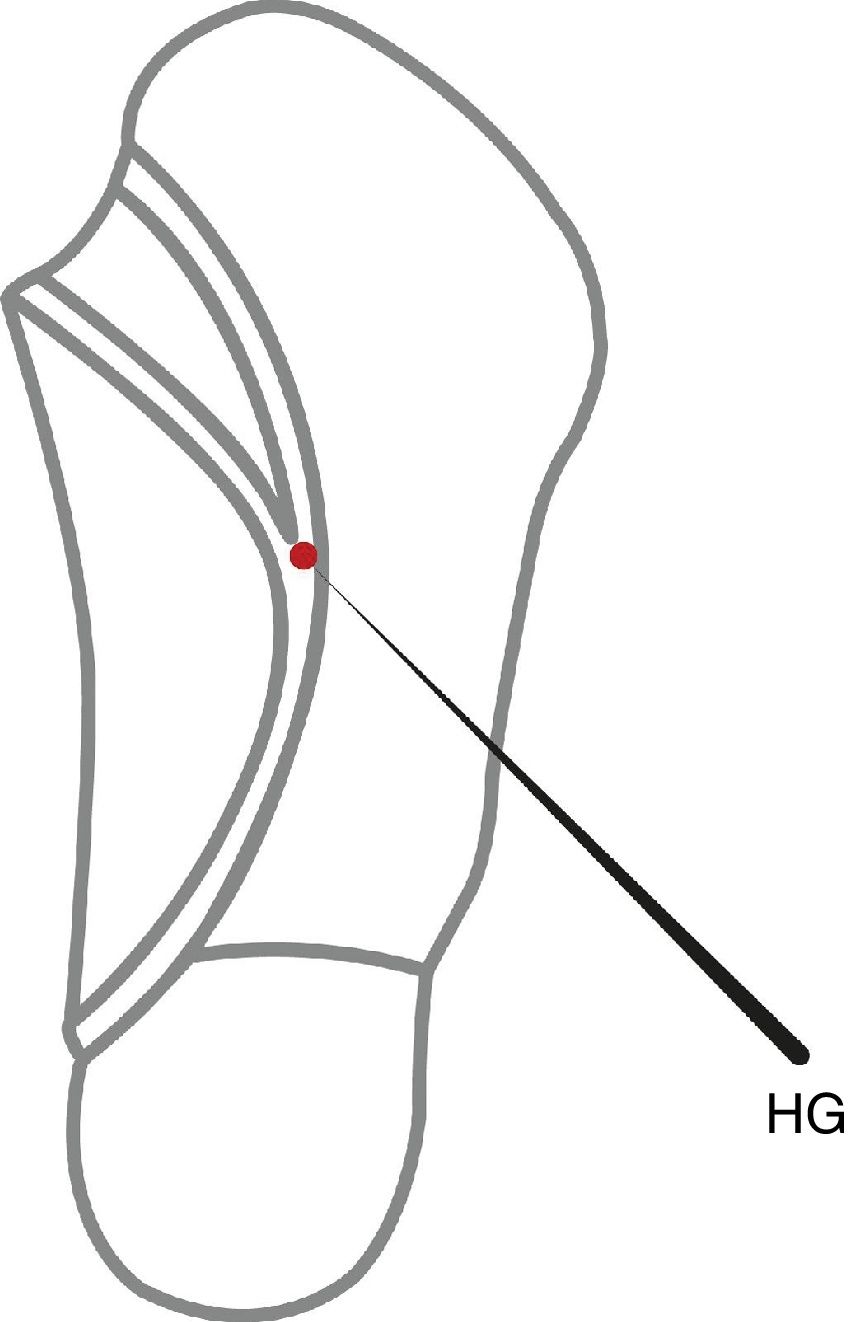
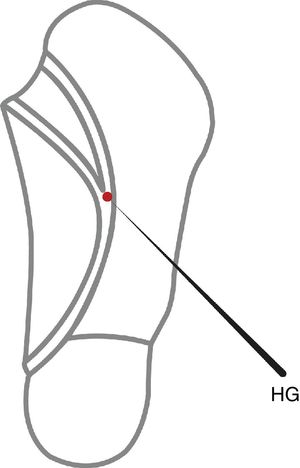
Auriculotherapy is frequently used in the treatment of cardiovascular disorders; therefore, the knowledge of its cardiovascular mechanisms is an important task.13 Besides, acupuncture in the same point but on opposite sides of the body had different effects.14,15 It has been reported that the Hypertensive Groove (HG) auricular point lowers blood pressure and improve anxiety,16 and acutely modifies second derivative photoplethysmogram indices in healthy subjects.17 The HG auricular point also called Hypotensive groove is located in the posterior and superior fold of the ear,18 see Figure 2.
Therefore, this study was aimed to evaluate the effect of manual acupuncture in HG on the PTT in healthy subjects; and also to analyze if there is a difference between the stimulation of this point in the right versus the left ear.
Materials and methodsStudy Design and settingA cross-sectional experimental without control study was conducted. The study was performed at Acupuncture Clinic, Unidad Iztapalapa, Universidad Autónoma Metropolitana.
PopulationAll of the subjects in this study were healthy student volunteers of the Institution Universidad Autónoma Metropolitana, campus Iztapalapa, Ciudad de México, México. These subjects were recruited by use of flyers.
There were 30 healthy subjects of any sex aged 26.4±4.9 years (mean±SD), non-smoker, without clinical data of cardiovascular diseases, obesity, athletic training, and without having received medication or treatment with acupuncture in the ten days before the study.
Ethical aspects. The Biological and Health Division Ethics Committee approved this study (Approval Number 27-093-2). The study conforms to the principles of the revised version of the Declaration of Helsinki (World Medical Association 2013). The subjects were provided with a written explanation about the study, and written informed consents were obtained.
DVP registrationTransducers for photoplethysmography (BIOPAC Systems, TSD200) were placed on the index finger of the left hand and the second toe of the left foot. These transducers transmitted infrared light of 860±90nm to obtain a DVP record. The response frequency of the photoplethysmograph was flat at 10Hz19,20 The digital output of the photoplethysmograph was recorded using a converter from an analog signal to a digital signal with a sampling frequency of 200 points per second (BIOPAC Systems, MP150) using the analysis platform provided by AcqKnowledge v. software 4.0. A record of 10minutes was obtained for each participant.
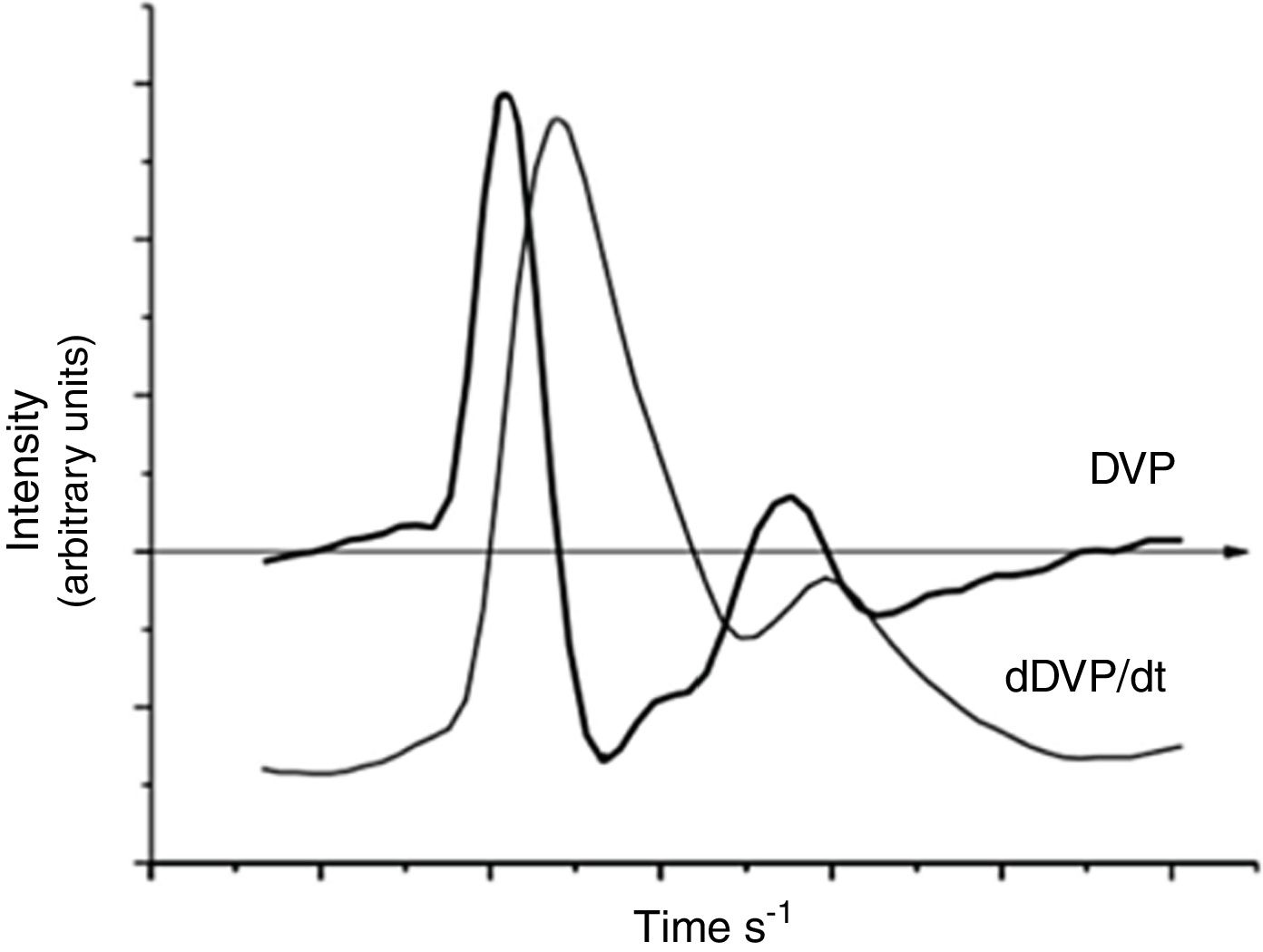
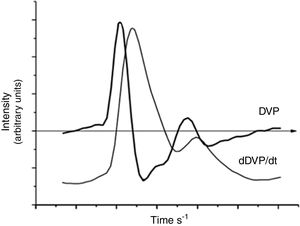
Calculation of pulse transit timePulse transit time change was estimated through the period elapsed between the start of the DVP in hand versus the foot. The exact beginning of the DVP was calculated by using the first derivative of the DVP obtained with the Origin software version 8.0 (Microcal Software, Inc., Northampton, MA, USA), Figures 3 and 4.
Auricular acupuncture treatmentManual acupuncture without additional electrical or laser stimulation was applied on the auricular point Hypertension Groove, Figure 2. The point in the ear was traditionally located wherein the needle was inserted vertically to a depth of 2mm for 10seconds. Sterile acupuncture needles that were 13mm, 0.22mm, with a silver handle (Seirin Corporation, Shizuoka, Japan) were used.
Practitioner's Background. One acupuncturist, with two years of experience, performed all the acupuncture stimuli.
Study ProtocolThe measurements were carried out after a fasting period of ≥ 8hours. During the study, the subjects remained supine. After registration of its clinical information, all subjects were at rest for a period ≥ 20minutes before starting the records. The measurements were taken between 9:00 a.m. to 12:00 p.m. to standardize the conditions regarding the circadian variations in blood pressure. After the rest period, digital photoplethysmographs were affixed to the hand and toe fingers of each subject. DVP measurements commenced, and after one-minute of registration, acupuncture in HG point was applied in the second 60 of the record for 10seconds. After the needle was removed, the DVP registration was continued to complete 600seconds After one week period of washout, the same procedure was carried out in the ear of the opposite side.
ComparisonsThe first comparison was made among the means of the PTT before, 30seconds of the basal registration period, and after post-acupuncture stimulation in each ear at 540 second. The second comparison was made between right or left ear stimulation.
Statistical AnalysisFor the analysis, the total sample and its division into two groups using the median (193ms) of basal PTT were considered: A subjects with shorter PTT (PTT<193ms) and B longer PTT (PTT> 193ms). The data are reported as mean±standard deviation. Paired t-Student tests were used to determine the differences between baseline versus treated values. We examined the Pearson correlations between the values of PTT before and after acupuncture in HG in either right or left ear of the total sample (TS), groups A and B, with shorter or larger PTT, respectively. The analysis was performed with the software SPSS 16.0 (SPSS IBM, USA). A p-value <0.05 was considered to be statistically significant.
ResultsThe study population consisted of 30 (13 female) healthy subjects having a global age of 26.4±4.9 (mean±SD).
Effect of the Hypertensive Groove auricular point in the pulse transit time
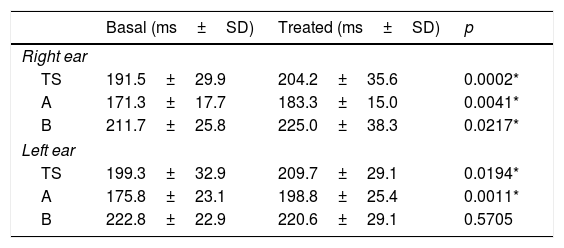
The effect of the manual acupuncture in the HG of the right ear on the PTT is shown in Table 1.
Effect of manual acupuncture in Hypertension Groove point in subjects with different basal levels of pulse transit time in: TS=total sample, A=group with shorter, and B=group with longer pulse transit time.
| Basal (ms±SD) | Treated (ms±SD) | p | |
|---|---|---|---|
| Right ear | |||
| TS | 191.5±29.9 | 204.2±35.6 | 0.0002* |
| A | 171.3±17.7 | 183.3±15.0 | 0.0041* |
| B | 211.7±25.8 | 225.0±38.3 | 0.0217* |
| Left ear | |||
| TS | 199.3±32.9 | 209.7±29.1 | 0.0194* |
| A | 175.8±23.1 | 198.8±25.4 | 0.0011* |
| B | 222.8±22.9 | 220.6±29.1 | 0.5705 |
Numbers are: mean±SD of pulse transit time in milliseconds.
The p-value of the t-student test for paired values.
The treatment with auriculopuncture in HG point in both the right or left ear produced a significant increase in PTT in the total sample. However, the subgroup with higher basal PTT in the treated left ear showed a non-significant decrease in TTP (p=0.5705).
Pearson correlation coefficients between pre- and post-acupuncture PTT with the right or left ear stimulation
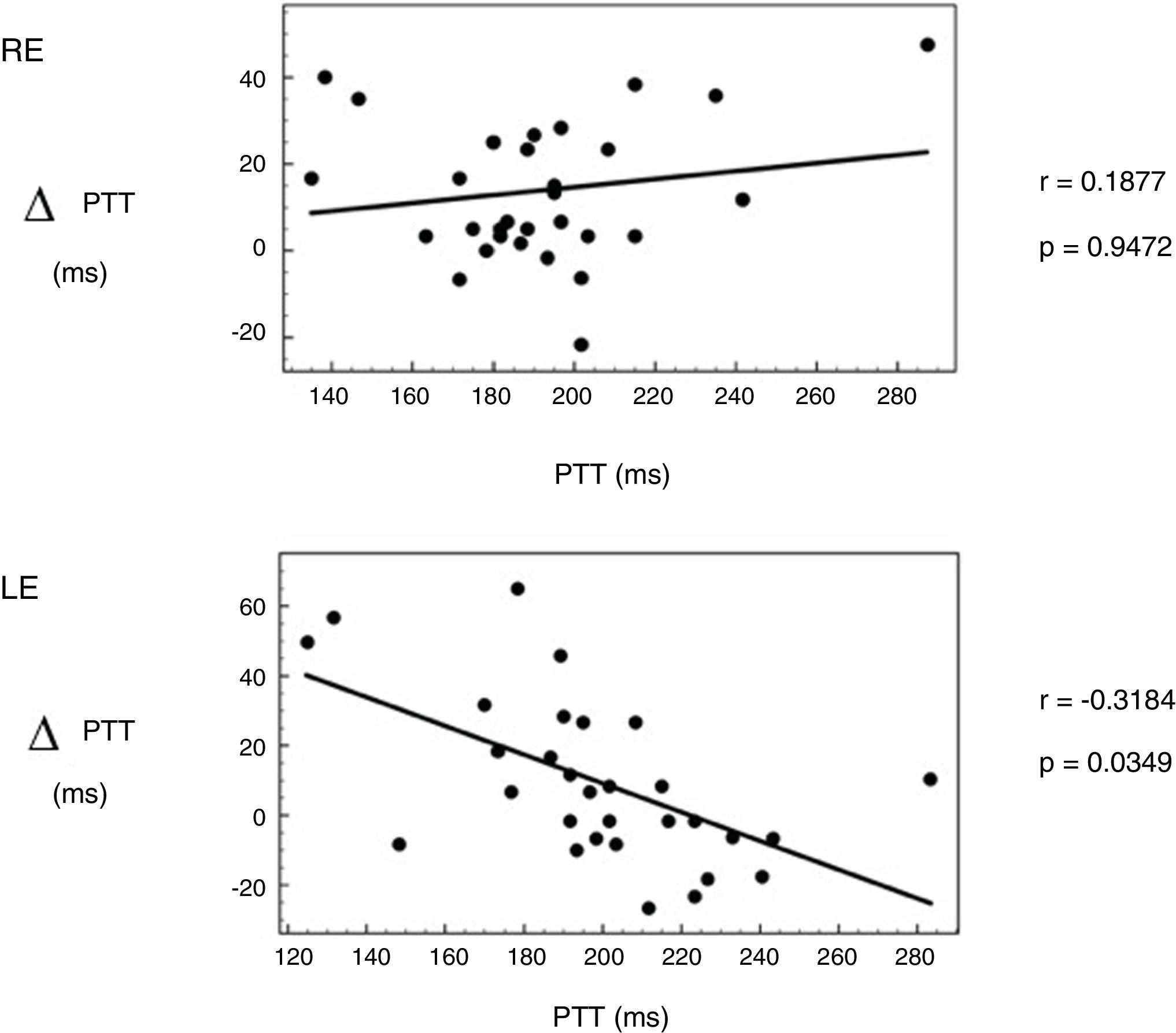
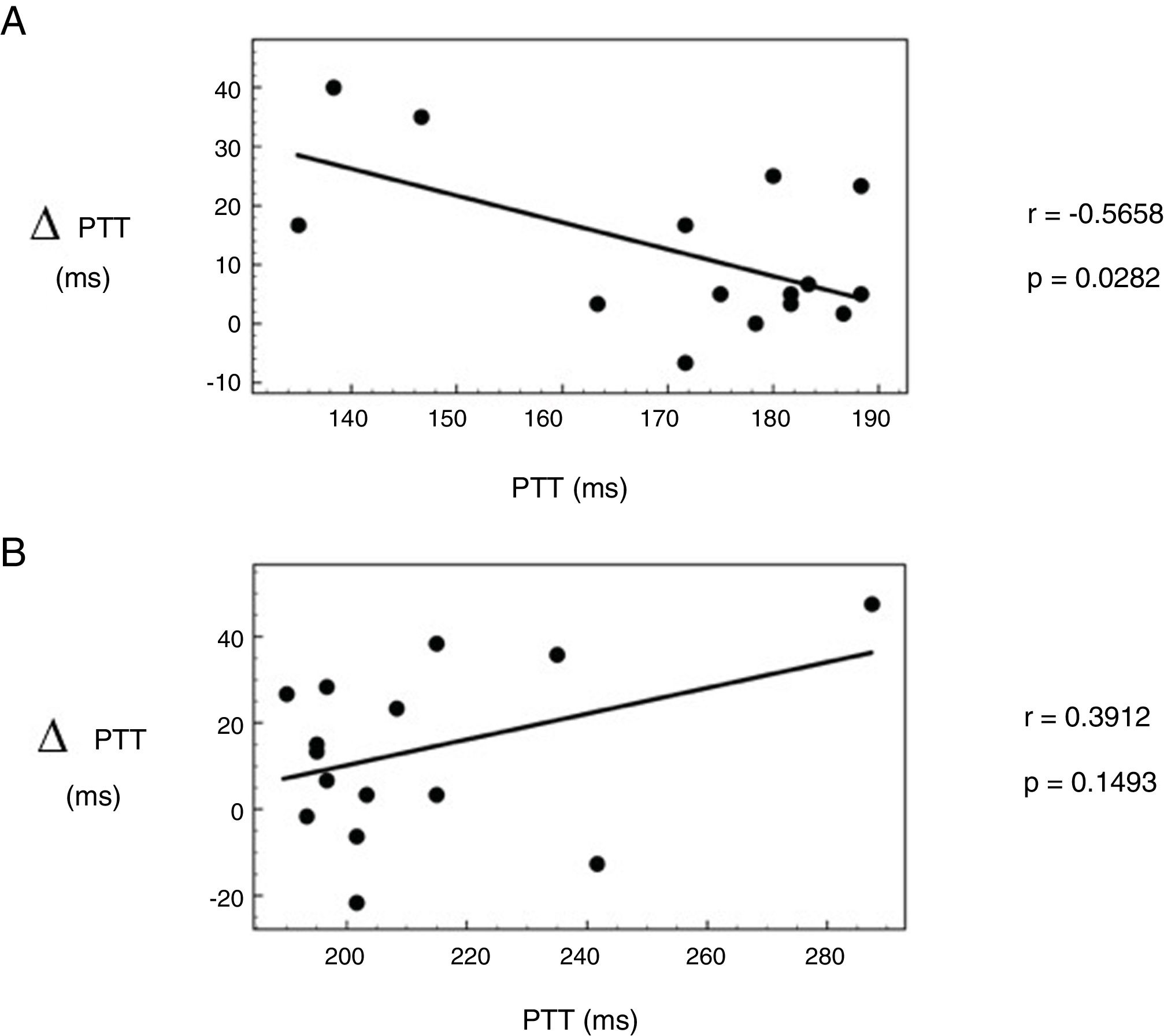
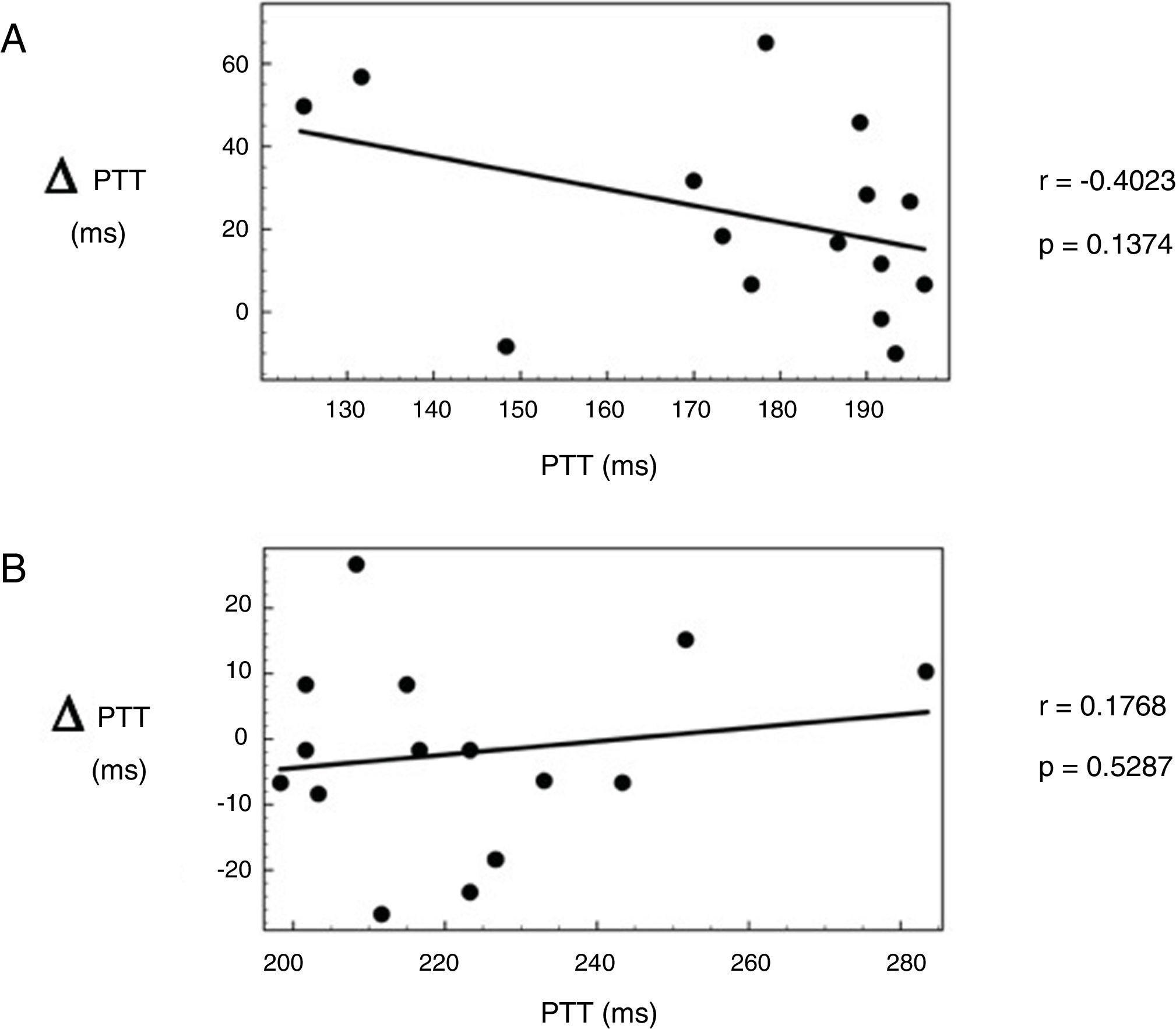
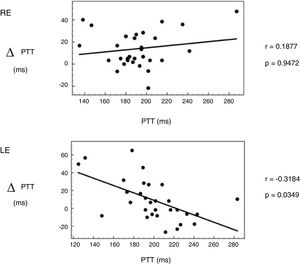
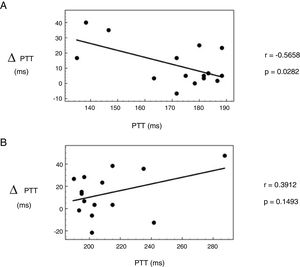
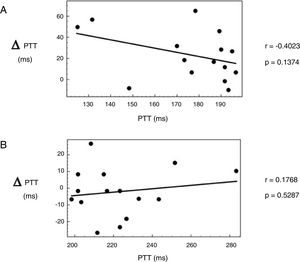
The Pearson correlation coefficients of basal PTT with the PTT changes elicited for acupuncture in the right or left ear are shown in Figures 5-7, respectively.
Pearson correlation coefficient between basal values and the differences in the pre- and post-treatment of pulse transit time elicited through manual acupuncture in Hypertension Groove in the total sample: RE=right ear and LE=left ear. p=the p-value calculated for the Pearson correlation coefficient.
Pearson correlation coefficient between basal values and the differences in the pre- and post-treatment of pulse transit time elicited through manual acupuncture in Hypertension Groove in the right ear: A) shorter and B) larger basal pulse transit time in milliseconds. p=the p-value calculated for the Pearson correlation coefficient.
Pearson correlation coefficient between basal values and the differences in the pre- and post-treatment of pulse transit time elicited through manual acupuncture in Hypertension Groove in the left ear. A) correspond with shorter and B) larger basal pulse transit time in milliseconds. p=the p-value calculated for the Pearson correlation coefficient.
In the total sample, the Pearson correlation coefficient analysis showed a positive and non-significant (p=0.9472) correlation in the subjects treated in the right ear, and negative and significant (p=0.0349) in the subjects treated in the left ear, see Figure 5.
In the subjects treated in the right ear, the Pearson correlation coefficient analysis showed a negative and significant (p=0.0282) correlation in the subjects with shorter basal PTT; and positive and no significant (p=0.1493) in the subjects with larger basal PTT.
In the subjects treated in the left ear, the Pearson correlation coefficient analysis showed a negative and no significant (p=0.1374) correlation in the subjects with shorter basal PTT; and positive and no significant (p=0.5287) in the subjects with larger basal PTT.
DiscussionThis study is the first that systematically examines the location specificity and response characteristics of cardiovascular changes in the relationship with the basal values of the dependent variable. The distinctive findings of this study were that treatment with auriculopuncture in HG point in the total sample, in both the right or left ear, produced a significant increase in PTT. However, in the subgroup treated in the left ear, and with higher basal PTT showed a non-significant decrease in TTP.
In the total sample, the Pearson's correlation coefficients between basal values of pulse transit time and the differences elicited through auriculopuncture in HG showed a non-significantly positive correlation for the right ear, and significantly negative for the left ear. Otherwise, in subjects with shorter basal PTT, stimulation in both right or left ear elicited a positive correlation, and in subjects with longer basal PTT, the correlation was negative.
PTT is a noninvasive method to investigate arterial elasticity and it is inversely related to PWV, and therefore useful to evaluate arterial stiffness.21 The analysis of PTT provides quantitative information regarding autonomic control mechanisms in the body;22 thus, PTT could be adopted as an index useful to evaluate the effects of acupuncture. Previous studies indicated that several auricular points improved symptoms of hypertension.23–26 Besides, it has been postulated that auricular points stimulation could influence the autonomic nervous system.27 Moreover, the stimulation of auricular points could originate vagal arousal through afferent impulses toward solitary tract nucleus.28 Besides, the HG auricular point is located in an ear zone innervated by an auricular branch of vagus nerve.29 Therefore, auricular acupuncture in HG could elicit changes through a mechanism related to the increased vagal activity.
Conclusions. Each one of the bilateral Hypertension Groove auricular points has differentiated effects on the pulse transit time of the healthy subjects. Moreover, the effect of this point depends on the basal state of pulse transit time. Further prospective studies are needed in patients with arterial stiffness to assess the potential therapeutic effect of HG in these patients.
Conflict of interestThe authors have no conflict of interest to declare