In the last few decades, aerially transmitted human fungal pathogens have been increasingly recognized to impact the clinical course of chronic pulmonary diseases, such as asthma, cystic fibrosis or chronic obstructive pulmonary disease. Thanks to recent development of culture-free high-throughput sequencing methods, the metagenomic approaches are now appropriate to detect, identify and even quantify prokaryotic or eukaryotic microorganism communities inhabiting human respiratory tract and to access the complexity of even low-burden microbe communities that are likely to play a role in chronic pulmonary diseases. In this review, we explore how metagenomics and comparative genomics studies can alleviate fungal culture bottlenecks, improve our knowledge about fungal biology, lift the veil on cross-talks between host lung and fungal microbiota, and gain insights into the pathogenic impact of these aerially transmitted fungi that affect human beings. We reviewed metagenomic studies and comparative genomic analyses of carefully chosen microorganisms, and confirmed the usefulness of such approaches to better delineate biology and pathogenesis of aerially transmitted human fungal pathogens. Efforts to generate and efficiently analyze the enormous amount of data produced by such novel approaches have to be pursued, and will potentially provide the patients suffering from chronic pulmonary diseases with a better management.
This manuscript is part of the series of works presented at the “V International Workshop: Molecular genetic approaches to the study of human pathogenic fungi” (Oaxaca, Mexico, 2012).
En las últimas décadas se ha reconocido cada vez más la influencia de los hongos patógenos para el ser humano, y cuya transmisión es aérea, en el curso clínico de afecciones pulmonares crónicas, como el asma, la fibrosis quística o la enfermedad pulmonar obstructiva crónica. Gracias al desarrollo reciente de métodos de secuenciación de alto rendimiento, que no requieren cultivo, en la actualidad los análisis metagenómicos permiten detectar, identificar e incluso cuantificar comunidades de microorganismos procariotas o eucariotas que habitan en las vías respiratorias del ser humano, y acceder a la complejidad de las comunidades microbianas cuya población es de baja densidad, que posiblemente desempeñan un papel en las enfermedades pulmonares crónicas. En la presente revisión examinamos cómo los estudios metagenómicos y genómicos comparativos pueden ayudar a superar los obstáculos de los cultivos de hongos, mejorar nuestros conocimientos sobre la biología fúngica, desvelar el diálogo cruzado (crosstalk) entre el pulmón del huésped y la microbiota fúngica asociada, y adquirir información sobre la influencia patogénica de estos hongos transmitidos por el aire que afectan al ser humano. Revisamos los estudios metagenómicos y los análisis genómicos comparativos de microorganismos cuidadosamente seleccionados, y confirmamos la utilidad de estas estrategias para definir mejor la biología y la patogenia de hongos de transmisión aérea que son patógenos para el ser humano. Los esfuerzos por generar y analizar eficientemente la ingente cantidad de datos obtenidos con estos nuevos métodos deberán continuar, y es posible que ofrezcan un mejor tratamiento de los pacientes portadores de enfermedades pulmonares crónicas.
Este manuscrito forma parte de la serie de artículos presentados en el «V International Workshop: Molecular genetic approaches to the study of human pathogenic fungi» (Oaxaca, México, 2012).
Although plant disease epidemics caused by fungi are recognized as having major impacts on food security, pathogenic fungi are emerging as major threats to animal health.27 Indeed, several severe wildlife declines have recently occurred in bats or amphibians pointing to previously unknown fungi as causes of mass mortalities. In humans, the contribution of fungi to the global burden of diseases is largely unrecognized. Over 600 fungal species have been reported to affect multiple organs and to cause mild-to-severe infections in immunocompetent or otherwise healthy individuals.10
In the last few decades, fungal infections have become a leading cause of mortality and morbidity especially in patients with severe immunological impairments.41 Indeed, the number of patients susceptible to fungal infections has increased dramatically as a consequence of underlining diseases (HIV infection, leucopenia, etc.) or treatments (including biotherapy) affecting their immunological status in the case of organ transplantation, surgery or cancer.41 In developing countries, invasive mold infections (especially aspergillosis and mucormycosis) are also more frequently reported both in a large economically deprived portion of the population but also in the limited but more prosperous portion, for which access to modern medical interventions (i.e. organ transplantation, intensive therapy for malignancies) is possible.17 The mortality due to mycoses still ranges from 30 to 50% in spite of recently discovered and more potent antifungal drugs as well as better diagnosis tools, which both need to be improved.61
Depending on the fungal burden and the immune status of the host, air-borne fungal pathogens may be harmless or cause invasive or non-invasive diseases, inflammation or even allergy.52 Indeed, in the case of Pneumocystis,16,60 a low fungal burden, defined as a colonization or carriage state with no clinical symptoms, could play a major role in the transmission of the disease from immunocompetent to susceptible patients or in the worsening of prognosis in chronic obstructive pulmonary disease (COPD) patients. Recent development of non-culture highthroughput sequencing methods enables detection, identification and even quantification of prokaryotic or eukaryotic microorganism communities inhabiting human digestive or respiratory lumina. Indeed, the lungs of healthy never-smoker individuals are inhabited by communities of bacteria that are few in number but composed of diverse genera, thus showing that the healthy lung is not as sterile as it first appeared.7,19,24 Although most recent studies focused mainly on bacterial communities, investigations have been initiated on viruses and fungi.18,21 These omics approaches are powerful enough to access the complexity of even low-burden microbe communities that modulate the immune system and are likely to play a role in chronic pulmonary diseases and pulmonary transplantation system.
In this review, we will focus on new generation technologies such as metagenomics or comparative genomics and try to approach how they can alleviate fungal culture bottlenecks and bring more knowledge about fungal biology and cross-talks between the host lung and the fungal microbiota. The scope of this review is restricted to aerially transmitted micromycetes and their impact on chronic pulmonary diseases such as asthma, cystic fibrosis (CF) or COPD.
Clinical impact of aerially transmitted micromycetes on chronic pulmonary diseasesFungi and lung allergySensitization to fungi is an important factor in patients with allergic respiratory tract diseases, playing a major role in the development, persistence and severity of low airway diseases, particularly asthma.44
Allergic bronchopulmonary mycosis (ABPM) can be caused by several fungi including Candida, Penicillium, Scedosporium, and Curvularia species. But the most common form of ABPM is allergic bronchopulmonary aspergillosis (ABPA) that is a well-recognized fungal complication of asthma and is caused by chronic or intermittent bronchial colonization with Aspergillus fumigatus.44 Severe asthma with fungal sensitization (SAFS) is less recognized but has been appropriately named to highlight that patients suffering from severe asthma are highly sensitive to fungal antigens and respond to oral antifungal therapy.22 The prevalence of ABPA ranges from 0.7% to 3.5% in asthmatic patients while it reaches 7–9% in CF patients.31,44
Fungi and chronic obstructive pulmonary diseasesIsolation of fungal conidia in the sputum of immunocompetent individuals often represents colonization with no clinical consequences. However, isolation of fungal conidia in sputum of immunocompromised or severely ill patients is highly predictive of invasive disease.45 For example, invasive pulmonary aspergillosis (IPA) primarily occurs in a context of neutropenia but patients with severe COPD or from intensive care unit have also emerged to be at risk for IPA.2 Advanced COPD stages, as well as prolonged use of corticosteroids, are correlated with a higher risk of developing IPA. The use of broad-spectrum antibiotics to prevent bacterial exacerbation episodes may also promote the emergence of fungal populations in airways.2
It is now widely accepted that infection is the predominant cause of exacerbation in COPD patients and most probably contributes to the pathogenesis of COPD.71 Even microorganism communities developing at low-burden in the lungs may perpetuate inflammatory and lung-remodeling responses that lead to an increased severity of COPD.59,60 This is illustrated by Pneumocystis jirovecii, a micromycete colonizing patients suffering from severe COPD. The Pneumocystis colonization state is defined as low number of organisms present in the lungs without clinical symptoms of pneumonia. The prevalence of colonizing P. jirovecii in COPD patients is increased, reaching 55% when compared to patients with other pulmonary diseases (reviewed in Morris and Norris57). Whether the installation of P. jirovecii is secondary to COPD or a risk factor for the establishment of this chronic disease remains to be elucidated. Several animal and human studies report Pneumocystis colonization as being a risk factor (i) to develop more severe COPD in non-HIV patients58 or (ii) to suffer from airway obstruction in HIV patients.55
Fungi and cystic fibrosisIn CF patients, a defective mucociliary clearance and a thickening of bronchial mucus lead to the entrapment of inhaled bacteria or fungal conidia, thus providing suitable conditions for germination and thus for development of respiratory infections.36 Although considerable attention has been paid over the last decades to bacterial infections in CF patients, understanding the role of fungal infections in the progression of the disease is only starting to rise. The most common agent of fungal infections in CF patients is by far A. fumigatus with a prevalence rate ranging from 5.9% to 58.3%.36 Other species such as Aspergillus terreus or Scedosporium spp. may also colonize the respiratory tract of CF patients and many more fungal species have been identified in the sputum of these patients by using pyrosequencing technology.21 Although a direct role of colonizing fungi on lung function in CF patients is difficult to ascertain, they most likely play a greater role in CF lung disease than previously thought. Indeed, more and more findings depict a clear association between older patients, bacterial colonization, lower lung function and the chronic presence of A. fumigatus.74,75
The clinical significance of P. jirovecii in CF patients remains poorly explored. Only few studies reported the frequency of colonization by P. jirovecii in CF patients to range between 1.3% and 21.5% in Europe29,34,67,73 while it reaches 38.5% in Brazil.63 The CF patients colonized by P. jirovecii do not seem to be at increased risk to develop Pneumocystis pneumonia (PcP) as reported in a 1-year-follow-up-longitudinal study, but a perpetual Pneumocystis colonization/clearance cycle seemed to occur in these patients.53 The immune system of CF patients is probably competent enough to prevent the shift toward severe PcP. Even if some authors hypothesize that low burden of Pneumocystis organisms may (as in COPD patients) fuel inflammatory response, lung tissue damage and worsening of respiratory function, more studies are needed to formerly assess Pneumocystis clinical impact on CF patients.13,32 Nevertheless, these colonized patients constitute a source of Pneumocystis organisms that can be potentially airborne-transmitted to susceptible patients with impaired immune system. Moreover, colonizing micromycetes may also alter the complex poly-microbial community inhabiting the CF lung. Synergistic or antagonistic interactions most probably occur between fungi, as well as between fungi and bacteria in the lungs of CF patients.13 Recently, exploration of the airway microbiota has revealed a relation existing between the absence of Pseudomonas aeruginosa and a better pulmonary function in CF patients colonized with P. jirovecii.21,34 Our knowledge is still far from covering the intricate network of microbial relations occurring in the lungs of patients with chronic diseases.
The lung microbiota: a complex polymicrobial communityThe exploration of the lung microbiota is only starting to raise interest as lungs were classically thought to be sterile.7,24,43 Numerous recent findings underscore the importance of microbiotas as a distinctive feature of tissue compartmentalization. While trillions of commensal bacteria termed “the microbiota” are in close proximity to a single layer of epithelial cells in the colon,6 only 20 to 1 bacteria per 1000 human cells seem to occur in lung tissue.19,24,76 Here, we review recent published data that analyze bacterial,5,14,18–21,26,28,30,46,50,51,56,77,82–84 fungal,20,21 and viral46,48,80,81 microbiota harbored by the human lung, using massive parallel sequencing techniques. Since these molecular methods can distinguish rare and difficult-to-cultivate causative microorganisms (such as P. jirovecii, Scedosporium apiospermum, atypical mycobacteria, anaerobes and viruses), as well as new or as yet unknown pathogens,5,8,9,15,48 corresponding results provide information on microbial community composition without a priori knowledge of existing microorganisms, and consequently offering new insights into lung diseases, especially into chronic pulmonary diseases such as CF, COPD, and asthma.
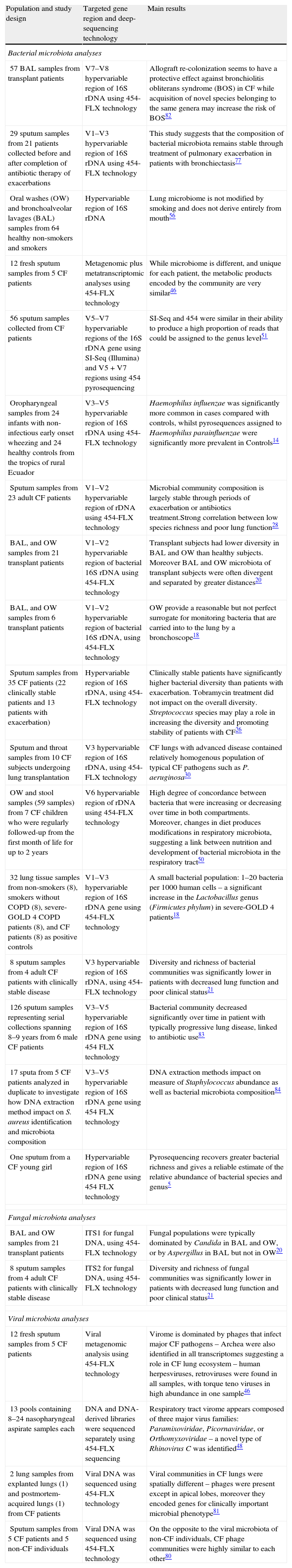
Lung microbiota: from medical concept to rational dataDespite some differences in microbiota composition, lung and intestinal populations similarly change over time,50 appear to be linked (core bacterial microbiota dominated by Veillonella and Streptococcus species), and are involved in inflammatory response.6,68 High degree of concordance between bacteria that were increasing or decreasing over time in both intestinal and respiratory compartments has been recently documented in CF children,50 as well as a general dysbiosis.23 Although the new high-throughput technologies have facilitated the identification and characterization of the human microbiome at mucosal sites including lungs, the mechanisms by which the commensal flora might influence lung immunity and their role in the development of inflammation are not well characterized. Moreover, published studies were mainly focused on bacterial communities (Table 1), while numerous results suggest virus implication in pulmonary exacerbation, and mold-related respiratory effects in chronic pulmonary diseases.38,42,65,66 So far, fungal and viral microbiotas have been poorly studied in respiratory tract.
Summary of the current studies analyzing lung microbial communities by high-throughput sequencing.
| Population and study design | Targeted gene region and deep-sequencing technology | Main results |
| Bacterial microbiota analyses | ||
| 57 BAL samples from transplant patients | V7–V8 hypervariable region of 16S rDNA using 454-FLX technology | Allograft re-colonization seems to have a protective effect against bronchiolitis obliterans syndrome (BOS) in CF while acquisition of novel species belonging to the same genera may increase the risk of BOS82 |
| 29 sputum samples from 21 patients collected before and after completion of antibiotic therapy of exacerbations | V1–V3 hypervariable region of 16S rDNA using 454-FLX technology | This study suggests that the composition of bacterial microbiota remains stable through treatment of pulmonary exacerbation in patients with bronchiectasis77 |
| Oral washes (OW) and bronchoalveolar lavages (BAL) samples from 64 healthy non-smokers and smokers | Hypervariable region of 16S rDNA | Lung microbiome is not modified by smoking and does not derive entirely from mouth56 |
| 12 fresh sputum samples from 5 CF patients | Metagenomic plus metatranscriptomic analyses using 454-FLX technology | While microbiome is different, and unique for each patient, the metabolic products encoded by the community are very similar46 |
| 56 sputum samples collected from CF patients | V5–V7 hypervariable regions of the 16S rDNA gene using SI-Seq (Illumina) and V5+V7 regions using 454 pyrosequencing | SI-Seq and 454 were similar in their ability to produce a high proportion of reads that could be assigned to the genus level51 |
| Oropharyngeal samples from 24 infants with non-infectious early onset wheezing and 24 healthy controls from the tropics of rural Ecuador | V3–V5 hypervariable region of 16S rDNA using 454-FLX technology | Haemophilus influenzae was significantly more common in cases compared with controls, whilst pyrosequences assigned to Haemophilus parainfluenzae were significantly more prevalent in Controls14 |
| Sputum samples from 23 adult CF patients | V1–V2 hypervariable region of rDNA using 454-FLX technology | Microbial community composition is largely stable through periods of exacerbation or antibiotics treatment.Strong correlation between low species richness and poor lung function28 |
| BAL, and OW samples from 21 transplant patients | V1–V2 hypervariable region of bacterial 16S rDNA using 454-FLX technology | Transplant subjects had lower diversity in BAL and OW than healthy subjects. Moreover BAL and OW microbiota of transplant subjects were often divergent and separated by greater distances20 |
| BAL, and OW samples from 6 transplant patients | V1–V2 hypervariable region of bacterial 16S rDNA, using 454-FLX technology | OW provide a reasonable but not perfect surrogate for monitoring bacteria that are carried into to the lung by a bronchoscope18 |
| Sputum samples from 35 CF patients (22 clinically stable patients and 13 patients with exacerbation) | Hypervariable region of 16S rDNA, using 454-FLX technology | Clinically stable patients have significantly higher bacterial diversity than patients with exacerbation. Tobramycin treatment did not impact on the overall diversity. Streptococcus species may play a role in increasing the diversity and promoting stability of patients with CF26 |
| Sputum and throat samples from 10 CF subjects undergoing lung transplantation | V3 hypervariable region of 16S rDNA, using 454-FLX technology | CF lungs with advanced disease contained relatively homogenous population of typical CF pathogens such as P. aeruginosa30 |
| OW and stool samples (59 samples) from 7 CF children who were regularly followed-up from the first month of life for up to 2 years | V6 hypervariable region of rDNA using 454-FLX technology | High degree of concordance between bacteria that were increasing or decreasing over time in both compartments. Moreover, changes in diet produces modifications in respiratory microbiota, suggesting a link between nutrition and development of bacterial microbiota in the respiratory tract50 |
| 32 lung tissue samples from non-smokers (8), smokers without COPD (8), severe-GOLD 4 COPD patients (8), and CF patients (8) as positive controls | V1–V3 hypervariable region of 16S rDNA gene using 454-FLX technology | A small bacterial population: 1–20 bacteria per 1000 human cells – a significant increase in the Lactobacillus genus (Firmicutes phylum) in severe-GOLD 4 patients18 |
| 8 sputum samples from 4 adult CF patients with clinically stable disease | V3 hypervariable region of 16S rDNA, using 454-FLX technology | Diversity and richness of bacterial communities was significantly lower in patients with decreased lung function and poor clinical status21 |
| 126 sputum samples representing serial collections spanning 8–9 years from 6 male CF patients | V3–V5 hypervariable region of 16S rDNA gene using 454 FLX technology | Bacterial community decreased significantly over time in patient with typically progressive lung disease, linked to antibiotic use83 |
| 17 sputa from 5 CF patients analyzed in duplicate to investigate how DNA extraction method impact on S. aureus identification and microbiota composition | V3–V5 hypervariable region of 16S rDNA gene using 454 FLX technology | DNA extraction methods impact on measure of Staphylococcus abundance as well as bacterial microbiota composition84 |
| One sputum from a CF young girl | Hypervariable region of 16S rDNA gene using 454 FLX technology | Pyrosequencing recovers greater bacterial richness and gives a reliable estimate of the relative abundance of bacterial species and genus5 |
| Fungal microbiota analyses | ||
| BAL and OW samples from 21 transplant patients | ITS1 for fungal DNA, using 454-FLX technology | Fungal populations were typically dominated by Candida in BAL and OW, or by Aspergillus in BAL but not in OW20 |
| 8 sputum samples from 4 adult CF patients with clinically stable disease | ITS2 for fungal DNA, using 454-FLX technology | Diversity and richness of fungal communities was significantly lower in patients with decreased lung function and poor clinical status21 |
| Viral microbiota analyses | ||
| 12 fresh sputum samples from 5 CF patients | Viral metagenomic analysis using 454-FLX technology | Virome is dominated by phages that infect major CF pathogens – Archea were also identified in all transcriptomes suggesting a role in CF lung ecosystem – human herpesviruses, retroviruses were found in all samples, with torque teno viruses in high abundance in one sample46 |
| 13 pools containing 8–24 nasopharyngeal aspirate samples each | DNA and DNA-derived libraries were sequenced separately using 454-FLX sequencing | Respiratory tract virome appears composed of three major virus families: Paramixoviridae, Picornaviridae, or Orthomyxoviridae – a novel type of Rhinovirus C was identified48 |
| 2 lung samples from explanted lungs (1) and postmortem-acquired lungs (1) from CF patients | Viral DNA was sequenced using 454-FLX technology | Viral communities in CF lungs were spatially different – phages were present except in apical lobes, moreover they encoded genes for clinically important microbial phenotype81 |
| Sputum samples from 5 CF patients and 5 non-CF individuals | Viral DNA was sequenced using 454-FLX technology | On the opposite to the viral microbiota of non-CF individuals, CF phage communities were highly similar to each other80 |
Briefly, lung microbiomes are disturbed in patients with chronic pulmonary diseases compared to healthy controls, with some geographic differences that might traduce local composition of indoor flora and/or the signature of the outdoor environment that the subjects are exposed to.14,19,21,24 Bacterial diversity seems to be adjustable according to primary disease (Table 1). In severe COPD, bacterial diversity is described to be higher than in lung samples from CF patients with a significant increase in the Lactobacillus genus,76 but this diversity remains limited in comparison to healthy subject.24 In asthmatic or wheezing infants, bronchial tree seems to harbor a specific flora that is disturbed by the presence of pathogens such as Haemophilus influenzae, as indicated from pyrosequencing,14 or clone library-sequencing35 or a combination of 16S rDNA microarray and clone library-sequencing approaches37; this microbiota is different from that of healthy individuals (predominantly composed of commensal bacteria).35 In CF, which is the most studied chronic pulmonary disease by metagenomics (Table 1), lung microbiota analyses point to a dominant role of Pseudomonas, the importance of some Streptococcus species in increasing the diversity and promoting stability of patients in CF, and the community partition into two groups (the dominant bacteria and the group of less dominant ones).26,83 Respiratory tract virome appears to be composed of three major virus families: Paramixoviridae, Picornaviridae, or Orthomyxoviridae, dominated by phage communities with some spatial differences in CF patients.46,48,80,81
While a higher bacterial diversity has been observed among asthmatic patients,37 decreased airway community richness and diversity have been correlated with deteriorating respiratory function (as measured by Forced Expiratory Volume in 1s) in CF patients.21,26,28,76,83,85 In lung explant sampling or broncho-alveolar lavages (BAL) after lung transplantation, the bacterial richness and diversity appear also significantly reduced in transplanted CF subjects.18,20,30 Pulmonary exacerbation does not appear associated with an increasing bacterial density in CF.83 In addition, changes in the composition of lung bacterial microbiota do not appear to account for exacerbations in patients with bronchiectasis.77 These divergent data probably result from differences in the primary disease physiopathology (asthma vs. CF) and underline the importance of deciphering the role of fungal microbiota.
Regarding transplanted CF patients, fungal populations were typically dominated by Candida in BAL and oropharyngeal washings (OW), or by Aspergillus in BAL but not in OW.20 Recently, Aspergillus culture was negatively correlated with a bacterial microbiota dominated by Pseudomonas.82 Using massive parallel sequencing strategy, we evaluated more extensively the diversity of fungi compared to culture methods, and observed a complex fungal biota in sputum samples with a majority of the fungal species or genera that were identified by pyrosequencing but not by cultures.21 Using phylogenetic tools, we also highlighted a high molecular diversity at the sub-species level for the main fungi identified in this study. Strikingly, the diversity and species richness of fungal and bacterial communities was significantly lower in patients with decreased lung function and poor clinical status, which highlights the role of potential interactions between microorganisms in the disease course.
Metagenomics: a new translational field with technical and medical perspectivesAdvanced techniques able to massively identify microbial sequences have provided new insights into the depth and breadth of fungal microbiota present in both healthy and abnormal lungs. To have the best chance to render deep-sequencing analyses highly informative, all steps of a metagenomic study, including wet and dry biology, have to be well-designed. From the methodological point of view, DNA extraction, primer design, and representativeness and quality of the sequences available in reference databases are undoubtedly limiting factors affecting these targeted metagenomic approaches. Most of the recent studies realized on respiratory samples used DNA extraction kit after mechanical homogenization of the sample.18,20,30,50,76,83,84 While bacterial identification based on 16S rDNA sequences compared to well-documented databases (such as SILVA, NCBI, HOMD or RDP) is widely used,64,70,78 fungal identification has been done in a more confidential manner. ITS1 and ITS2 are the most popular loci used to identify and discriminate between fungal species; recent development of curated reference databases has allowed more reliable comparison and identification of ITS amplicons.21,70 ITS2 region has revealed to be most discriminant for fungus identification at the taxonomical level.3 Optimal detection of low abundance taxa is increased by replicate analysis of samples,18,70 and must be combined with an appropriate bioinformatic analysis that can screen for amplicon quality (Q-score), short trimmed sequences, trimmed sequences containing some undetermined nucleotides, or chimeric sequences (such as QIIME pipeline).5,14,21,26,28,30,46,48,51,80,81,83,84 Considering the clinical or medical point of view, the contribution of fungi to chronic pulmonary disease genesis, exacerbation, and management need to be extensively studied. Fungal (and viral) microbiota should be included into deep-sequencing studies of lung diseases, since viral and fungal infections are emerging pathogens and have been described as exacerbation inducers of chronic pulmonary diseases (CF, COPD, asthma).22,38,42,65,66 Moreover, metagenomic analysis and whole genome (shotgun) approaches allowed to access pan-microbial resistance genome or resistome as proposed by Rolain et al.,69 which is of particular relevance when phage community is highlighted in viral lung microbiota.46,80,81 More recently, coupling metatranscriptomic to metagenomic has provided an overview of the present bacterial taxa and their current activities46; such an approach, that is currently limited to the bacteria, remains to be developed for fungi.
Lung microbiota analysis is a new translational research area, offering the potential to redefine the process that drives the progression of chronic pulmonary diseases such as CF, COPD, and asthma. Studies focused on human respiratory fungal microbiota will clearly impact our patient management, changing current paradigms of physiopathology and therapy. Whether we can develop personalized therapy strategies, such as adjusting antimicrobial therapy according to the local spatial distribution of microbiome, or manipulate the complex microbiota (i.e. controlling growth of less desirable microorganisms as previously proposed40), represent new challenges.
Comparative genomics: genetic basis of pathogen life stylesComparative genomics can be defined as a comparison of genome structure and function across different species or strains. The objectives are to gain a better understanding of how species have evolved and to determine the function of genes and noncoding regions of the genomes.33 Another purpose is to identify groups of genes that play unique biological role in a particular microorganism and thus provide an efficient approach to exploring the genetics of specialized functions such as pathogenesis and the evolution of virulence in pathogenic organisms.54 Not only can sets of genes that are unique be identified, but the location and distribution of these genes among microorganisms can also shed light on their origins and functions.
For example, comparative genomic analysis (CGA) among fungal pathogens can provide the genetic basis to understand the microorganism adaptation to an ecological niche (narrow/wide spectrum of hosts, animal/plant hosts, etc.) or lifestyle (opportunist, pathogen, saprophyte, etc.). CGA can also shed light toward development of novel disease management strategies for combating these human diseases.
Unlike the relatively easy identification of virulence factors directly associated with human diseases in many bacterial and viral pathogens, the identification of virulence factors or, more correctly, virulence associated factors in fungal pathogens, is usually less clear-cut and we still have much to learn regarding how fungi can cause diseases. Providentially, the genomes of many of the most important human fungal pathogens have been sequenced over the past decade and we will present, in this section, how CGA of related species, has contributed to our understanding of the pathogenesis of some pulmonary human fungal pathogens like Aspergillus spp., Coccidioides spp., and Cryptococcus spp., and the evolution of virulence in these microorganisms. Information collected from the comparison of fungal genome sequences can also help scientists to develop novel molecular diagnostic tools and new strategies to combat fungal human diseases.
While comparative transcriptomics analyses also offer a great opportunity to unveil the genetic bases of fungal biology and pathogenicity (i.e. 4,11,12,39,62,79), we will focus here on the contributions brought by comparative genomics studies in (i) fungal pathogenesis and virulence evolution, as well as in (ii) the identification of fungal drug targets and development of novel molecular diagnostic tools.
Insights into pulmonary fungal pathogenesis and virulence evolutionThe overriding goal of CGA of human pathogenic fungi is the identification of pathogen-specific genes required to efficiently colonize and infect the human host.
As soon as 2005, the genome sequencing of two related strains of Cryptococcus neoformans serotype D and comparative genomics with already-available fungal genomes has allowed to find unique C. neoformans genes that may contribute to the unusual virulence properties of this basidiomycetous yeast.47
More recently, Fedorova et al.25 have used the power of comparative genomics to gain insights into the genetic mechanisms that may contribute to the metabolic versatility and pathogenicity of A. fumigatus. By comparing the genomes of two A. fumigatus clinical isolates and two closely related but rarely pathogenic species (i.e. Neosartorya fischeri and Aspergillus clavatus), they found that species-specific genes (known as lineage-specific (LS) genes) exhibited a subtelomeric bias and that these genes clustered together in chromosomal islands that were enriched for pseudogenes, transposons and other repetitive elements.25 In A. fumigatus, the metabolic activities encoded by these subtelomeric genomic islands involve carbohydrate and amino acid metabolism, transport, detoxification, or secondary metabolite biosynthesis that may facilitate the adaptation to heterogeneous environments such as soil or a mammalian host.25 Interestingly, results obtained by these authors suggest that the origin of A. fumigatus LS genes cannot be attributed to horizontal gene transfer (HGT) like it was previously thought. Instead, phylogenies of these LS genes, their subtelomeric bias and size differences are consistent with the duplication, diversification and differential gene loss (DDL) hypothesis.25 In other words, gene duplication seems to be the primary genetic mechanism responsible for the origin of these LS genes. Moran et al.,54 compiling the results of comparative genomics studies performed on human pathogenic fungi (such as A. fumigatus, C. neoformans, Coccidioides spp.) in an excellent review, also highlighted that the evolution of virulence across these fungi has occurred largely through gene duplication and the expansion of gene families, particularly at subtelomeric regions.
Another comparative genomic analyses focusing on Coccidioides immitis, Coccidioides posadasii, a nonpathogenic relative, Uncinocarpus reesii, and a more diverged pathogenic fungus, Histoplasma capsulatum, interestingly revealed increases and decreases in gene family size (gene gain and loss) which can be associated with a host/substrate shift from plants to animals in the Onygenales.72 On the whole, these results suggest that Coccidioides spp. are not soil saprophytes but that they might have evolved in response to interaction with an animal host, i.e. with dead animal hosts on soil.72
Identification of drug targets and development of novel molecular diagnostic toolsBecause available antifungal therapies (which most of the time lead to side effects, toxicities, drug interactions and antifungal resistance) are currently limited, the search for alternative therapies and/or the development of more specific drugs is increasingly relevant and necessary.
Selecting new molecular targets by comparative genomics, homology modeling and virtual screening of compounds is promising in the process of new drug discovery. For example, Abadio et al.,1 in 2011, identified potential drug targets (i.e. essential genes and/or genes affecting the cell viability, conserved in pathogenic organisms and absent in the human genome) common to 8 human fungal pathogens (Candida albicans, A. fumigatus, Blastomyces dermatitidis, Paracoccidioides brasiliensis, Paracoccidioides lutzii, C. immitis, C. neoformans and H. capsulatum) using comparative genomics strategy. Of 10 genes that were present in all pathogenic fungi analyzed and absent in the human genome, they focused on 4 candidates: trr1 that encodes for thioredoxin reductase, rim8 that encodes for a protein involved in the proteolytic activation of a transcriptional factor in response to alkaline pH, kre2 that encodes for a-1,2-mannosyltransferase, and erg6 that encodes for Δ(24)-sterol C-methyltransferase. The authors argue that these results are currently being used to virtually screen chemical libraries.1
The availability of multiple complete genomes from various fungal species, strains or isolates may also facilitate the development of molecular diagnostic and typing methods for fungal diseases. Recently, the analysis and comparison of four complete mitochondrial genomes of P. jirovecii isolates – fungi that still lack a complete and annotated nuclear genome – have highlighted a potential new genetic target for P. jirovecii strain typing and molecular diagnostic tool.49
ConclusionsMetagenomic studies and comparative genomics analyses of carefully chosen microorganisms are useful novel approaches to study biology and pathogenesis of aerially transmitted human fungal pathogens. Implementation of these methodologies involves massive parallel sequencing technologies and bioinformatic analyses, implicating an intimate collaboration between biologists and bioinformaticians. We argue that studies based on “omic” approaches (i.e. metagenomics, transcriptomics) have to be pursued to make sense of such enormous volumes of data, to expand functional annotation of fungal pathogen genomes, and to improve the collection of large-scale genetic variation data at within- and between-species levels, in order to better understand the implication of these fungi in the course of chronic pulmonary diseases and to improve the management of such patients.
Conflict of interestsThe authors declare that they have no conflict of interests.
We thank Lille 2 University, the Lille Pasteur Institute, the Agence Nationale de Sécurité Sanitaire de l’Alimentation, de l’Environnement et du Travail (ANSES, grant EST/2011/1/053), the French Ministry of Health and Research (PHRC Nu 2006/1902), and Pfizer France Pharmaceutical Division (Nu 2006/158), and Vaincre la mucoviscidose (Mucofong, Mucofong-ATF, MucoBacMyco – RC 2012-0600697) for their financial support.