Patients with psoriatic arthritis (PsA) have a significant prevalence of metabolic syndrome (MS), however studies conducted in Latin America describing comorbidities of PsA patients are still scarce. The aim of the present work was to estimate the prevalence of MS in patients attending PsA clinics in tertiary university centers in the south region of Brazil and to evaluate the achievement of the minimal disease activity criteria among those with and without MS.
Materials and methodsA cross-sectional study was conducted; patients were recruited in two university hospitals and data collected during a routine clinic visit. The prevalence of MS was estimated using the National Cholesterol Education Programme's Adult Treatment Panel III (NCEP/ATP III). The prevalence of patients achieving the MDA criteria was compared between individuals with and without MS using Chi-square test.
ResultsOne hundred and five patients with PsA were evaluated, 81 in center A (Rio Grande do Sul) and 24 in center B (Paraná); 54.3% were female (N=57), the average age was 55.7 (SD 11.6) years and the median time of diagnosis in years was 7.4 (.16–42.2). A total of 51.9% (N=54) were diagnosed with MS., hypertension was found in 51.4% (N=54) and obesity in 38.1% (N=40) of the sample. There was no statistically significant association between MS and MDA.
ConclusionPatients followed in PsA clinics in university tertiary centers in the south of Brazil have a significant prevalence of MS. This work emphasizes the importance of the screening and treatment of comorbidities in PsA.
Los pacientes con artritis psoriásica (APs) tienen una prevalencia significativa de síndrome metabólico (SM), pero los estudios realizados en América Latina que describen las comorbilidades asociadas con esta enfermedad son escasos. El objetivo del presente trabajo fue estimar la prevalencia de SM en pacientes que asisten a clínicas de APs en centros universitarios de tercer nivel en la región sur de Brasil y evaluar el cumplimiento de los criterios mínimos de actividad de la enfermedad (MDA) entre aquellos con y sin SM.
Materiales y métodosSe llevó a cabo un estudio transversal con pacientes reclutados en dos hospitales universitarios; los datos se recopilaron durante una visita clínica de rutina. La prevalencia de SM se estimó utilizando el Panel III de Tratamiento para Adultos del Programa Nacional de Educación sobre el Colesterol (NCEP-ACT III). La prevalencia de pacientes que alcanzaron los criterios de MDA se comparó entre individuos con y sin SM mediante la prueba de chi-cuadrado.
ResultadosSe evaluaron 105 pacientes con APs, 81 en el centro A (Rio Grande do Sul) y 24 en el centro B (Paraná); 57 (54,3%) eran del sexo femenino, la edad promedio fue de 55,7 (DE: 11,6) años y la mediana del tiempo de diagnóstico en años fue de 7,4 (0,16-42,2). Un total de 54 (51,9%) individuos fueron diagnosticados con SM, y se encontró hipertensión también en 54 (51,4%) y obesidad en 40 (38,1%) de ellos. No hubo una asociación estadísticamente significativa entre SM y MDA.
ConclusiónLos pacientes seguidos en clínicas de APs en centros universitarios de tercer nivel en el sur de Brasil tienen una prevalencia significativa de SM. Este trabajo enfatiza la importancia del cribado y del tratamiento de las comorbilidades en la APs.
The understanding of spondyloarthritis as a systemic disease brought to light the interrelationship with the high cardiovascular risk seen in this population.1 Previous studies have shown that patients with psoriatic arthritis (PsA) have a high prevalence of obesity and metabolic syndrome(MS)2,3 with cardiovascular disorders representing their leading cause of death.4 In this context, the European League Against Rheumatism (EULAR) recommends screening for cardiovascular diseases and managing cardiovascular risk factors in the clinical follow-up of this population.5
In addition to the impact of the Metabolic Syndrome on cardiovascular risk and, therefore, mortality, there is an association of MS with the severity of the autoinflammatory condition. Patients with MS have a higher rate of radiographic damage and a greater need for tumor necrosis factor inhibitor (TNFi) therapy to control arthritis compared to patients without MS.2 A prevalence of MS is reported to be about 1.3 times higher in PsA than in patients with isolated psoriasis.6 Minimal disease activity (MDA) criteria are used to assess disease activity in PsA.7 Overweight and obese patients with PsA achieve sustained MDA (more than one year) less frequently than normal-weight patients.8 In this sense, improvement in MS was demonstrated in patients treated with tumor necrosis factor inhibitors (TNFi) in a two-year follow-up.9
The MS consists of a variety of metabolic abnormalities that increase the risk of cardiovascular disease (CVD) with diabetes mellitus (DM) and obesity representing the most important ones.10,11 Adipose tissue secretes inflammatory mediators that include mainly leptin, plasminogen activator inhibitor-1 (PAI-1), interleukin 6 (IL-6) and tumor necrosis factor alpha (TNF-α).12 TNF-α, Leptin and PAI-1 induce endothelial dysfunction and IL-6 and TNF-α promote insulin resistance in skeletal muscle and liver and pro-inflammatory activity in synovial tissue.13 In addition, these inflammatory cytokines inhibit the production of adiponectin, which has a protective effect against metabolic and vascular diseases.14 In this sense, there is a description of a 5.3% increase in the risk of developing PsA for each unit increase in body mass index (BMI) in patients with psoriasis.15
The prevalence of MS in the Brazilian general population is around 30–40%.16 Data on the prevalence of MS among patients with PsA in the Brazilian population and other Latin America countries are scarce. The prevalence of MS among patients with other autoimmune diseases living in Brazil is high: a study in the northeast region demonstrated a 51.3% prevalence of MS among patients with rheumatoid arthritis (RA) versus 21.8% in the controls from the local community17; another work conducted in south Brazil found a 39.2% prevalence of MS among RA patients.18
The present study aimed to investigate the prevalence of MS (and its components), overweight and obesity in PsA patients followed at university hospitals in southern Brazil. In addition, the association between MS and PsA disease activity, represented by the achievement of the MDA, was studied.
Material and methodsA cross-sectional study was conducted in two university hospitals located in south of Brazil. Adult patients with PsA diagnosed by a rheumatologist and followed in the PsA clinic were invited during a routine visit to participate.
Definition and assessment of outcomesData collection: Metabolic syndrome (MS) was defined according to the National Cholesterol Education Program's Adult Treatment Panel III (NCEP/ATP III) metabolic syndrome criteria. In order to be diagnosed with MS, the individual should fulfill three or more risk factors19:
- •
central obesity (waist circumference greater than 102cm for men and 88cm for women),
- •
systemic hypertension (systolic pressure greater than or equal to 130mmHg or diastolic pressure greater than or equal to 85mmHg, previous diagnosis of hypertension or current use of antihypertensive drugs),
- •
high blood glucose (fasting blood glucose greater than or equal to 100mg/dL, previous diagnosis of type 2 DM or current treatment for DM),
- •
low High Density Lipoproteins (HDL) (less than or equal to 40mg/dL for men and less than or equal to 50mg/dL for women),
- •
hypertriglyceridemia (greater than or equal to 150mg/dL) or current use of antilipemic agents.
Obesity was assessed using the BMI criteria, defined as weight over square heigh. According to World Health Organization, eutrophy was considered as BMI between 20 and 25, values above 25kg/m2 were considered overweight and values over 30kg/m2 were considered obesity. Obesity was graded at levels: I from 30 to 34.9kg/m2, II from 35 to 39.9kg/m2 and III above 40kg/m2.
A patient was considered in MDA when 5 of the following 7 criteria were met: tender joint count≤1; swollen joint count≤1; Psoriasis Area and Severity Index (PASI)≤1 or body surface area (BSA)≤3%; patient pain visual analog score (VAS pain)≤15; patient global disease activity (VAS global)≤20; Health Assessment Questionnaire (HAQ) Disability Index≤0.5; tender entheseal points≤1.20 Since the analysis aiming to compare the achievement of MDA between patients with and without MS was defined a posteriory, data on MDA status was available only for patients recruited in Hospital de Clinicas de Porto Alegre, where MDA criteria are registered in routine practice. MDA status was not available for patients included in Hospital Evangélico de Curitiba. As a way of pairing the MDA assessment with the assessment of disease activity by continuous score, the DAS-28 of the participants at inclusion was measured. The DAS-28 is a validated instrument for the assessment of disease activity in rheumatoid arthritis and that, before the arrival of instruments aimed at spondyloarthropathies, was widely used in the evaluation of inflammatory arthropathies in general. DAS28 is calculated based on assessment of pain and swelling of 28 joints, global assessment of disease by the patient and serum level of inflammatory tests (C-reactive protein or erythrocyte sedimentation rate)
The data were collected during a routine visit in the PsA Clinic from April 2016 to October 2018 and complemented by information recorded in electronic medical records when necessary. Immediatly before the routine visit, the patient was instructed to answer patient reported outcomes (PROs) as Functional Capacity Score – HAQ 20, questionnaire on pain, on fatigue and on disease activity and cutaneous component using a visual analog scale (VAS).
Then, during the usual care the rheumatologist assessed previous history of comorbidities and its treatment and performed the 66/68 joint count, anthropometric measures (weight, height, waist circumference), blood pressure measurements at rest and entheseal count according to the Leeds Enthesitis Index.
Lipid profile (High Density Lipoproteins and triglycerides), fasting glucose and glycated hemoglobin were included in routine outpatient follow-up exams. Laboratorial exams collected up to 3 months before inclusion in the study were accepted.
Statistical analysisSample size calculation: Based on the prevalence of previous studies,3,19,20 considering a 95% confidence interval, prevalence of MS assumed at 30% and a half-width of the confidence interval between 5 and 10%, a sample of n=81 was necessary to detect the prevalence of MS.
Quantitative variables were tested for normality using Shapiro–Wilk test and described as mean (standard deviation) if normally distributed or median (25/75 interquartiles) if a non-normal distribution was found. Independent t test or Mann–Whitney U test were used to compare quantitative variables between the two hospitals according to tests for normality and Chi-square test was used to compare qualitative variables.
The comparison of achievement of MDA disease criteria (yes/no) between patients with and without metabolic syndrome was analyzed using Chi-square test. It was also evaluated between patients with and without obesity.21
Ethical considerations: All patients in the study signed an informed consent form. The study was approved by the ethics committee of the Porto Alegre clinic hospital, project number GPPG 16 0165 and of Beneficent Evangelical Society of Curitiba, protocol number 2.346.248.
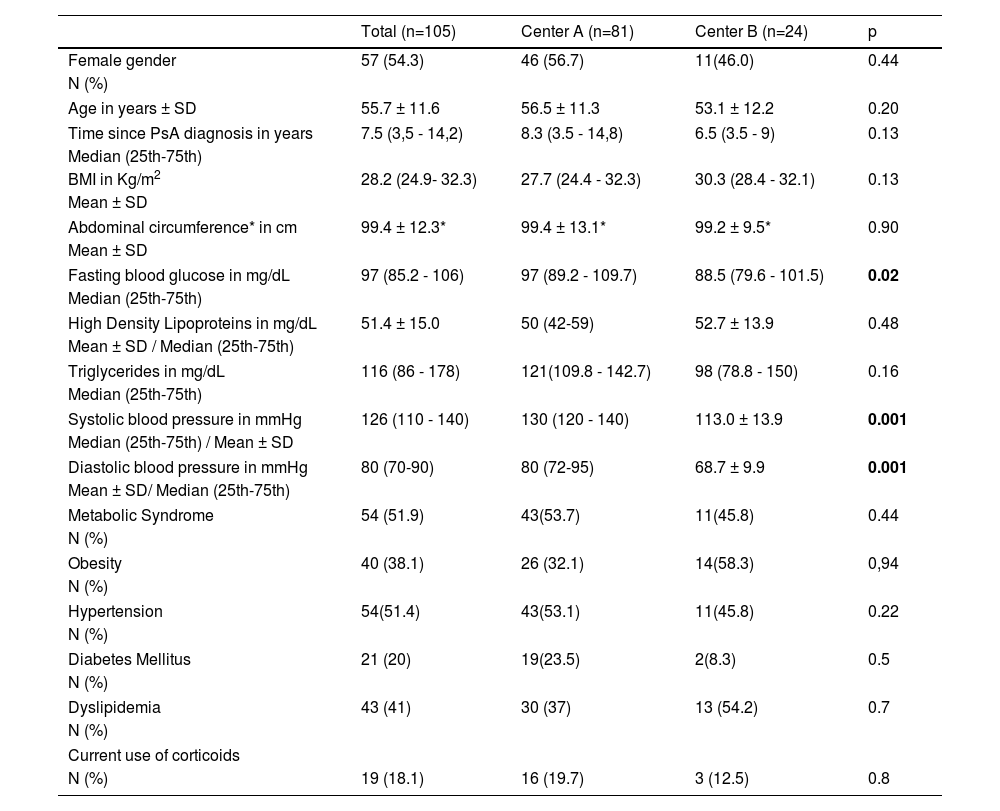
ResultsA total of 105 patients with psoriatic arthritis were recruited, 81 from center A (Rio Grande do Sul) and 24 from center B (Paraná). In this sample, 54.3% were female (N=57), the mean age was 55.7±11.6 years, and the median time of diagnosis of PA in years was 7.4 (0.16–42.2). Table 1 summarizes population characteristics globally and at each center. A comparison was made between the two centers. Although the prevalence of MS and its comorbidities did not differ, the levels of fasting glucose and systolic and diastolic blood pressure were statistically different. Center B had better blood pressure levels in the routine consultation and lower glycemic levels in control exams. There was no statistically significant difference in other population characteristics between the two hospitals.
Characteristics of the PsA patients included in the study.
| Total (n=105) | Center A (n=81) | Center B (n=24) | p | |
|---|---|---|---|---|
| Female gender | 57 (54.3) | 46 (56.7) | 11(46.0) | 0.44 |
| N (%) | ||||
| Age in years ± SD | 55.7 ± 11.6 | 56.5 ± 11.3 | 53.1 ± 12.2 | 0.20 |
| Time since PsA diagnosis in years | 7.5 (3,5 - 14,2) | 8.3 (3.5 - 14,8) | 6.5 (3.5 - 9) | 0.13 |
| Median (25th-75th) | ||||
| BMI in Kg/m2 | 28.2 (24.9- 32.3) | 27.7 (24.4 - 32.3) | 30.3 (28.4 - 32.1) | 0.13 |
| Mean ± SD | ||||
| Abdominal circumference* in cm | 99.4 ± 12.3* | 99.4 ± 13.1* | 99.2 ± 9.5* | 0.90 |
| Mean ± SD | ||||
| Fasting blood glucose in mg/dL | 97 (85.2 - 106) | 97 (89.2 - 109.7) | 88.5 (79.6 - 101.5) | 0.02 |
| Median (25th-75th) | ||||
| High Density Lipoproteins in mg/dL | 51.4 ± 15.0 | 50 (42-59) | 52.7 ± 13.9 | 0.48 |
| Mean ± SD / Median (25th-75th) | ||||
| Triglycerides in mg/dL | 116 (86 - 178) | 121(109.8 - 142.7) | 98 (78.8 - 150) | 0.16 |
| Median (25th-75th) | ||||
| Systolic blood pressure in mmHg | 126 (110 - 140) | 130 (120 - 140) | 113.0 ± 13.9 | 0.001 |
| Median (25th-75th) / Mean ± SD | ||||
| Diastolic blood pressure in mmHg | 80 (70-90) | 80 (72-95) | 68.7 ± 9.9 | 0.001 |
| Mean ± SD/ Median (25th-75th) | ||||
| Metabolic Syndrome | 54 (51.9) | 43(53.7) | 11(45.8) | 0.44 |
| N (%) | ||||
| Obesity | 40 (38.1) | 26 (32.1) | 14(58.3) | 0,94 |
| N (%) | ||||
| Hypertension | 54(51.4) | 43(53.1) | 11(45.8) | 0.22 |
| N (%) | ||||
| Diabetes Mellitus | 21 (20) | 19(23.5) | 2(8.3) | 0.5 |
| N (%) | ||||
| Dyslipidemia | 43 (41) | 30 (37) | 13 (54.2) | 0.7 |
| N (%) | ||||
| Current use of corticoids | ||||
| N (%) | 19 (18.1) | 16 (19.7) | 3 (12.5) | 0.8 |
Note: PsA,psoriatic arthritis; N, number; SD, Stand derivation *without differentiating gender
A prevalence of 51.9% (N=54) of MS was verified in the population with psoriatic arthritis followed up in a tertiary care outpatient clinic. The prevalence of comorbidities in the general sample and by center is summarized in Table 1. Two patients had no recent laboratory tests, but in only 1 case it was not possible to define whether the subject met the criteria for MS.
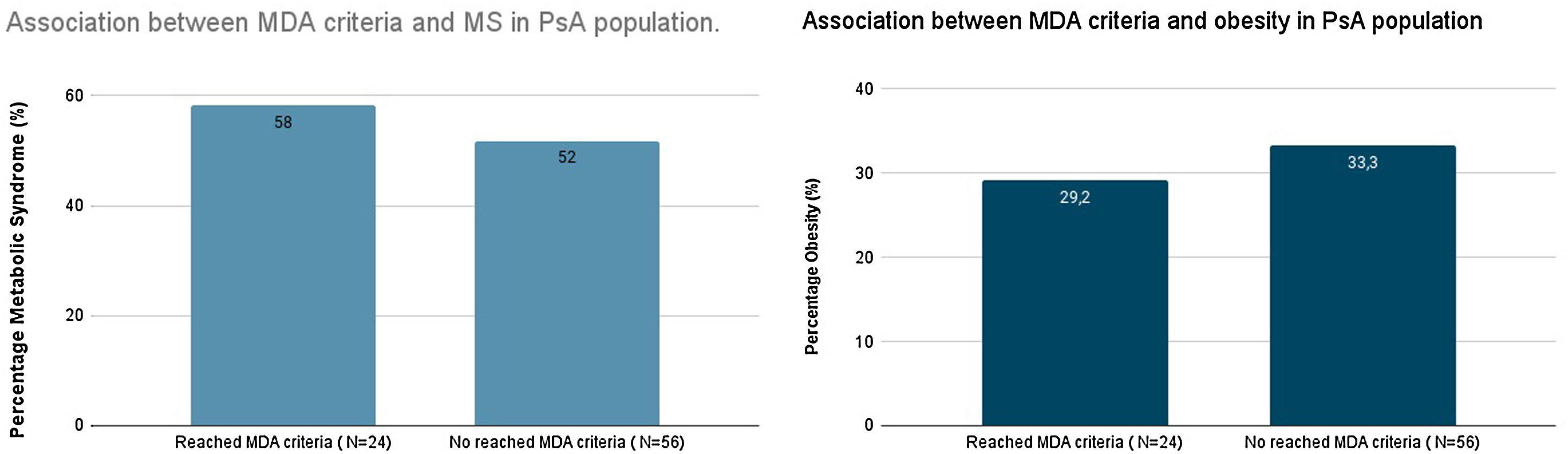
A secondary analysis was performed with the population of center A, with a view to evaluating the possibility of association of MS and obesity with evaluation of rheumatic disease control using the MDA criteria. Of the 81 patients recruited at center A, 29.6% (N=24) met the MDA criteria and the mean DAS28 of was 3.35 with a standard deviation of 1.32. Among patients who met the MDA criteria of which 58.3% (N=14) had MS. Among patients who did not reach MDA (n=56) the prevalence of MS was 51.8% (N=29). There was no statistical difference in the prevalence of MS between patients who achieved MDA and patients who did not achieve MDA (p=0.59). Obesity was identified in 29.2% of patients who achieved MDA (N=7) and in 33.3% of patients who did not achieve MDA (N=19), and it was not significant (p=0.71), as illustrated in Fig. 1. There was no statistical difference in mean BMI between patients who reached MDA (27.7±4.4) and those who did not reach MDA (28.7±5.8) (p=0.21), although a difference of 1 point was observed between the groups. Poisson regression univariate analysis also found no association of achieving MDA with population characteristics.
DiscussionIn line with other studies conducted around the world, this work showed that patients with PsA treated at university hospitals in southern Brazil have an important prevalence of MS (51.9%). In addition, the 51.4% prevalence of hypertension and 20% prevalence of diabetes, two important cardiovascular risk factors, demonstrates the great vulnerability of this population to harsh outcomes such as death, stroke and acute myocardial infarction. In this study, no difference was identified in the proportion of patients reaching therapeutic target for MDA between obese/non-obese and with MS versus without MS.
The prevalence of MS in the Brazilian population reported in recent publications has a significant variation among studies, going from 12.4% to 28.5% in men and from 10.7% to 40.5% in women.22 This variety is due to the lack of uniformity of criteria for MS.22 In the population of southern Brazil, a small study conducted in a single city found a prevalence of 8.5% in men and 22% in women according to the criteria of the NCEP/ATP III.23 Thus, the prevalence of MS found in our sample, composed by PsA patients followed in a tertiary health center is higher than that of the Brazilian general population.
In comparison with other studies in the population with PsA, our study also had a higher prevalence of MS. A Turkish study showed a 35.5% prevalence of MS by the NCEP/ATP III criteria among PsA patients compared to only 14.6% in the healthy controls.24 An Irish study, using the NCEP/ATP III criteria, identified a 44% prevalence of MS; their sample had an average age similar to ours and was predominantly female, but PsA disease duration was longer.2 An American study found a similar prevalence of 58.1% with the same criteria used in this study, however with a predominantly male population (95%).25
Considering other immune mediated diseases, such as RA, which was the first to have demonstrated association with cardiovascular diseases,26 studies showed a worse metabolic profile in patients with PsA compared to RA.27 In southern Brazil the prevalence of MS (according to the NCEP/ATP III criteria) in people with RA was 39.2% compared to 19.5% in healthy controls (p<0.001).18 Since this work with RA patients was conducted in the same region of Brazil (and same hospital) and included a similar population (mean age 56.8 years old and 50% men), we can hypothesize that the metabolic profile of patients with PsA is more pronounced than in RA.18
Regarding the comorbidities that are part of MS, as in other studies, there was an important prevalence of arterial hypertension.2,25 The prevalence of hypertension is around 35% in the Brazilian population.28 In this study, 51.4% of the sample met the criteria for hypertension. Dyslipidemia was another cardiovascular risk factor that emerged in the analysis, reaffirming findings from previous studies.29 Diabetes had a prevalence slightly above that described in the literature, around 12–18.6%.30 Obesity was present in 40% of the evaluated patients, representing twice the prevalence of the Brazilian population.31 However, compared with a study with a population with PsA in the Mediterranean, the BMI of our sample was lower by about 1 point, as well as the abdominal circumference values were lower in our sample by 1.5 points.32
Numerous studies have sought the association of MS with worse PsA activity indexes.2,8,33 Some studies have shown an association with the severity of the condition, using specific models of severity criteria as radiographic evaluation and need for more medication to control the disease2 and with a cutaneous component for answered an interview and standardized questionnaires (Dermatology Life Quality Index questionnaire [DLQI], 36-Item Short Form Health Survey [SF-36] and EuroQol Five-Dimension Questionnaire Three-Level version [EQ-5D-3L].34
Recently, an Italian study aimed to assess the influence of MS in obtaining MDA. In this sample 59.3% had MS and an inverse association was found between the presence of MS and the probability of reaching MDA in the univariate analysis (OR 0.45, p<0.001).35 The high prevalence of metabolic syndrome and obesity found in our population led us to attempt an exploratory attempt to assess the association between these conditions and disease activity, using the MDA assessment instrument, in our population. However, I emphasize that the study was not designed to assess association and, therefore, the sample size calculation was not performed with this approach. We could not find an inverse association between the presence of MS and the achievement of MDA. However, the sample size was calculated aiming to analyze the prevalence of MS (our primary objective) and not the association between MS and disease activity and it is possible that the study was unpowered to demonstrate that association. In this sense, the nullity of the hypothesis of association between metabolic syndrome with reaching MDA and obesity with reaching or not the MDA criteria observed in our study cannot be attested, is an exploratory finding. To test this hypothesis, a cohort study should be carried out in which the sample size for this purpose was calculated.
Although not significant, in our study we found an 1-point difference in median BMI when comparing patients achieving MDA status versus those not on MDA. In fact, studies indicate that obesity is associated with worse disease parameters. In this context an experimental study conducted in Switzerland showed a positive impact of the introduction of a specific dietary protocol for 12–16 weeks. The average weight loss was 18.7kg (IQR 14.6–26.5) or 18.6% (IQR 14.7–26.3) of basal weight. The percentage of patients with MDA increased from 29 to 54% (p=0.002) after weight loss.36
The main limitation of our study is the lack of a control group, allowing us to calculate the prevalence of MS in a population with the same demographic factors, but without PA. A priori, our intention was to compare the prevalence of metabolic syndrome in the study population with the prevalence in the general population. As the study was limited to patients followed at tertiary centers, the prevalence of comorbidities may have been overestimated. Furthermore, the lack of data on characteristics that are known to influence the course of autoimmune disease such as smoking that is associated with axial disease in patients with PsA and who end up not being evaluated by the MDA criteria.37
In addition to the limitation in the evaluation of demographic characteristics relevant to the scope of the article. C-reactive protein dosage and erythrocyte sedimentation rate, which are part of the follow-up of patients with spondyloarthritis, were not collected in our database. In addition, the study was carried out in only 2 centers in southern Brazil, with limited external validity.
In conclusion, more than half of PsA patients seen at university centers in southern Brazil have metabolic syndrome. The findings of this study are a warning to rheumatologists and other health professionals responsible for the care of patients with PsA. The high prevalence of MS results in increased cardiovascular risk. The management of these comorbidities, and not just the disease activity, should be part of the follow-up of these patients.
Cardiovascular risk control goals are in line with recent International League of Rheumatology Associations (ILAR) recommendations on the management of psoriatic arthritis in low-resource settings. This guideline highlights the need for greater attention in screening for infectious diseases and tracking associated comorbidities.38 In general, populations with limited resources are excluded from large Clinical Trials evaluating the treatment of psoriatic arthritis. Thus, there is little evidence of the safety of using disease-modifying medications in an endemic setting for several infectious diseases, such as tuberculosis.39 In parallel, the prevalence of associated comorbidities and their impact is also poorly studied in Latin American and African countries. Timely recognition of these conditions is necessary for adequate interventions in the course of these diseases and long-term modification in the mortality of this population.
In that regard, weight control, blood pressure, narrow glycemic targets and dyslipidemia control should be encouraged. In this sense, multidisciplinary approach, with a physical educator and nutritionist for example, will contribute not only to the control of immune-mediated disease activity, but also to the survival of this population, which has cardiovascular disease as its main cause of death.
Ethical considerationsAll patients in the study signed an informed consent form. The study was approved by the ethics committee of the Porto Alegre clinic hospital, project number GPPG 16 0165 and of Beneficent Evangelical Society of Curitiba, protocol number 2.346.248.
Financial supportNone.
Conflicts of interestThe authors declare no conflict of interest regarding the manuscript.