Chronic obstructive pulmonary disease (COPD) remains a priority in clinical practice, but it still presents gaps in care coordination, diagnosis, and treatment that have tangible impact on patients’ outcomes. The CARABELA-COPD previously identified key improvement areas within the Spanish healthcare system, setting the foundation for enhanced COPD care. As a continuation of the initiative, this document presents expert-driven recommendations to improve COPD care in the Spanish healthcare system.
Material and methodsThe CARABELA-COPD methodology involved seven pilot hospitals across Spain and included national and regional expert meetings. Through thematic discussions and prioritization exercises, key areas for COPD care improvement were identified and refined. This manuscript summarizes the resulting recommendations for the areas prioritized by the experts.
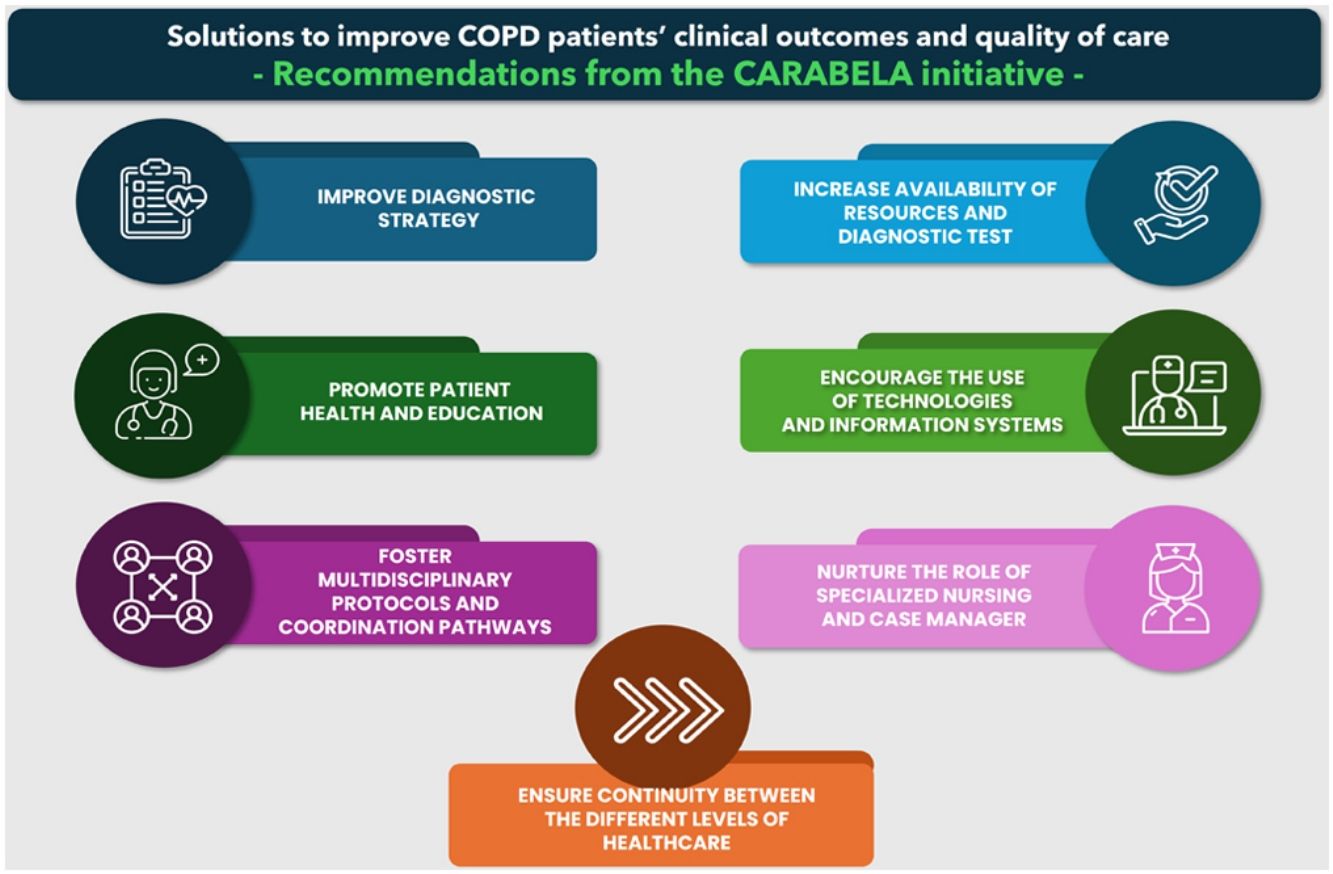
ResultsThe proposed strategies emphasize the importance of early detection, optimizing healthcare resource use, and implementing standardized care pathways to ensure a more uniform and effective management of the disease. Specific focus is placed on the role of specialized nursing, ensuring smooth transitions between levels of care, and integrating digital tools to facilitate clinical decisions.
ConclusionsThese recommendations are intended to close the gap between evidence-based guidelines and real clinical practice, so that every patient receives high-quality individualized care. Through collaboration between healthcare professionals, scientific societies, and policymakers, CARABELA-COPD seeks to reduce disparities in care, enhance system effectiveness, and ultimately improve quality of life for patients with COPD.
La enfermedad pulmonar obstructiva crónica (EPOC) sigue siendo una prioridad en la práctica clínica. Sin embargo, presenta deficiencias importantes en la coordinación asistencial, el diagnóstico y el tratamiento que impactan negativamente en los resultados. La iniciativa CARABELA-EPOC identificó áreas de mejora dentro del sistema sanitario español, sentando las bases para optimizar la atención a la EPOC. Como continuación de esta iniciativa, este documento presenta recomendaciones elaboradas por expertos para mejorar el manejo de la EPOC en España.
Material y métodosLa metodología CARABELA-EPOC involucró siete hospitales piloto e incluyó reuniones nacionales y regionales de expertos. Mediante discusiones y ejercicios de priorización, se definieron las áreas clave para la mejora de la atención a la EPOC priorizadas por los expertos. Este manuscrito resume las recomendaciones resultantes para dichas áreas.
ResultadosLas estrategias propuestas destacan la importancia de la detección temprana, la optimización en el uso de los recursos sanitarios y la implementación de rutas asistenciales estandarizadas para lograr un control más uniforme y eficaz de la enfermedad. Se presta especial atención al papel de la enfermería especializada, a la mejora de la continuidad asistencial entre niveles de atención y a la integración de herramientas digitales para facilitar la toma de decisiones clínicas.
ConclusionesLas recomendaciones buscan cerrar la brecha entre guías basadas en evidencia y la práctica clínica real, garantizando atención individualizada de calidad. La colaboración entre profesionales, sociedades científicas y responsables políticos pretende reducir desigualdades, mejorar la eficiencia y aumentar la calidad de vida de los pacientes con EPOC.
This article is a continuation of the CARABELA-COPD initiative previously described in detail in de Miguel-Diez et al. 2025,1 where the methodology, participating hospitals, and expert panels were outlined. Building on that foundation, the current manuscript focuses on presenting the consensus-driven recommendations and proposed actions that emerged from these expert discussions, focusing on the areas that were prioritized to improve COPD management across diverse healthcare settings in Spain.
The strategic recommendationsDespite advances in knowledge, care and currently available treatment, COPD is the third leading cause of death worldwide2 and constitutes a major health problem due to its high prevalence, increasing incidence, social impact and economic costs. In Spain, 5 out of every 100 men and 2 out of every 100 women aged 40 years and older have COPD, and these values increase with decreasing income level.3 The management of COPD in Spain generates high healthcare costs,4,5 with an annual expenditure of €4644655, mainly due to ICU admissions, longer hospital stays, aging of the population, and several additional elements.4,5
COPD has been under the healthcare system spotlight for decades. The Spanish National Health System developed a COPD strategy6,7 15 years ago, but this policy today still has numerous shortcomings and faces challenges in implementing improvements in the care process. This is partly due to heterogeneity in adherence to clinical practice guidelines,8 as well as issues like underdiagnosis and, consequently, undertreatment.9 Despite considerable efforts to improve COPD care and patient outcomes in Spain, the expected benefits have not yet manifested as observable outturns.10–12
The CARABELA initiative aims to evaluate and comprehend the difficulties encountered by the Spanish health system in managing chronic illness, serving as a catalyst for systemic change to enhance disease management.13 Although several autonomous communities have implemented COPD-specific strategies,14 the CARABELA-COPD initiative offers an added value by identifying barriers and proposing objective, cross-regional recommendations based on experiences from multiple Spanish hospitals. It aims to support and complement local efforts by providing a common national framework.
As previously described, the CARABELA-COPD is a multicenter project involving seven hospitals across diverse Spanish healthcare settings. It identified seven key areas for COPD management improvement, which were refined through a national consensus meeting and four regional workshops involving expert discussions, debates, and prioritization based on clinical relevance, feasibility, and systemic impact. The present manuscript summarizes the strategic recommendations and proposed actions that emerged from these discussions, focusing on the areas that had a higher priority among the experts (Fig. 1): diagnostic strategy, availability of resources and diagnostic tests, multidisciplinary protocols and coordinated pathways, the role of specialized nursing, and continuity across healthcare levels. It provides a practical analysis of the current and future scenarios in COPD management, highlighting the necessary changes needed to shape a future in which all patients receive the best care available.
Material and methodsThe methodology used for the CARABELA-COPD initiative has been described in detail in a previous publication.1 In brief, the CARABELA-COPD methodology has been a four-phase process of work and transformation that involved individual sessions and detailed analysis of resources, protocols, and organization in seven pilot hospitals representative of Spanish COPD management. This effort led to the identification of seven areas of improvement.1 These areas were subsequently evaluated during the national CARABELA-COPD meeting for their significance and potential impact on improving COPD management. Results were then further refined in four regional meetings which explored regional differences in COPD management strategies across Spain and prioritized a series of action plans. More than 120 healthcare professionals from different specialties and levels of care, including Internal Medicine, Pulmonology, Primary Care, Emergency Care and Pharmacy, participated in both national and regional meetings to identify the areas with the greatest impact and to draw up responses to the areas of improvement identified. The strategic interventions and recommendations that emerged from all participants in CARABELA-COPD highlighted the importance of this initiative as a reference in the Spanish COPD care landscape.
Since the study did not involve any interventions on patients or the collection of patient data, approval from a research ethics committee was not required.
ResultsDiagnostic strategyAlthough COPD is a leading cause of morbidity and mortality worldwide, its proper diagnosis remains a challenge, with approximately 70% of cases remaining underdiagnosed.15,16 In this context, improvement in diagnostic strategies was identified as the first action, and participants in the CARABELA-COPD initiative proposed the following actions to be developed to improve one of the main weaknesses of this disease.
- 1)
Promotion of a strategy to identify patients with symptoms consistent with COPD. The early and accurate identification of polypathological patients with suspected COPD is crucial for improving clinical outcomes and quality of life.17,18 Strategies based on consensus clinical criteria that allow more efficient detection of COPD in this patient group are proposed. These strategies involve the training of health professionals of all specialties involved in the management of the disease.12 Occupational health can play an important role by contributing to the identification of patients by performing spirometry tests on subjects with exposure to smoke, fumes, dust, or pollutants and known smokers. Despite the fact that tobacco remains the main environmental risk factor for COPD, epidemiological studies have shown that about 30% of patients with COPD have never smoked,16 meaning additional potential environmental and genetic factors must also be borne in mind.19,20 Overall, this approach would probably result in a higher number of COPD patients being referred to a specialist by primary care (PC).
- 2)
The implementation of training plans (technical aspects, referral criteria, and circuits) focused on specialties involved in the management of COPD patients. To streamline the diagnosis and treatment of patients with suspected COPD, a preferential care circuit should be established in hospital care for patients with suspected COPD. This circuit prioritizes the performance of respiratory function tests for patients attending initial consultations. The aim is to reduce waiting times and ensure rapid and accurate diagnosis through appropriate resource allocation and optimization of care processes. This approach fosters efficiency-based clinical practice and continuous improvement and enhances patient experience and health outcomes.21,22
COPD diagnosis in PC often relies on clinical assessment alone, leading to underdiagnosis and suboptimal treatment.23 It is therefore essential to ensure the adequate provision of diagnostic resources and tests. Reactivating functional tests for COPD diagnosis appears promising in enhancing diagnostic accuracy and improving patient outcomes. In this respect, CARABELA-COPD experts prioritized two solutions to address this issue.
- 1)
Reactivation of COPD testing in PC (spirometry and alpha-1 antitrypsin). Training initiatives aimed at enhancing spirometry proficiency among PC practitioners are imperative. To this end, a collaborative effort involving healthcare professionals, policymakers, and healthcare systems is mandatory.24,25 In fact, the establishment of expert networks operating under a common care framework would result in equitable access for patients not only to available resources, but also to cutting-edge technologies (new diagnostic procedures, gamified training, etc.), and would foster the notion of COPD management as a cross-functional process. The experts also emphasized that the generation of a shared resource structure between hospitals and PC, along with shared access to available training courses and technological resources, would enhance collaboration and improve patient care outcomes. In this respect, the creation or upgrading of multipurpose day hospitals could contribute to better patient follow-up and the much sought-after multidisciplinary continuity of care.26
- 2)
Developing a common strategy with pulmonary rehabilitation units. The evidence shows that pulmonary rehabilitation programs are key elements in the treatment of COPD, given the benefit they confer on respiratory function, including health-related quality of life, and functional and maximal exercise capacity.27 Therefore, the creation of pulmonary rehabilitation clinics or increasing the number of these facilities can further enhance the continuum of care and support provided to COPD patients.
The integration of referral criteria and the standardization of COPD care processes are crucial in view of the complexities of managing this disease, which include associated comorbidities, the involvement of multiple medical specialties, and the multitude of intra- and extra-hospital processes required. Within the context of evolving care strategies, two actions were ranked as the most relevant.
- 1)
Development/refinement of referral protocols that guide the transition from PC to hospital settings, ensuring that functional assessments are performed before referral to specialist consultation. This step is essential, because it prepares the specialist with essential information about the patient's condition, potentially expediting the diagnostic and treatment processes. This approach would address the frequent bottleneck in the referral process from PC to hospitals, which often arises from outdated or unclear referral criteria. So, the definition/update and dissemination of comprehensive care protocols for patients throughout the care process, incorporating the perspective of different professionals and care levels would help reduce waiting lists, promote early detection of COPD, and avoid short-term readmissions.
- 2)
Establishment of a streamlined pathway and fast-track entry from emergency care to hospital care and PC for patients with more urgent clinical situations. The creation of a rapid and direct transition pathway between care settings for patients in urgent clinical conditions is vital for managing COPD progression effectively. This initiative reduces waiting times in emergency care and improves clinical outcomes, including reductions in hospital stays and mortality.28
These targeted initiatives enhance the overall efficiency and effectiveness of COPD care. Spanish Scientific Societies underscore the importance of such multidisciplinary and integrative approaches in its guidelines, advocating for collaborative protocols that address both the respiratory and systemic aspects of COPD.29
Role of specialized nursing and case managerSince COPD is a complex chronic condition requiring meticulous management to prevent the progression of the disease, nursing personnel often serve as primary caregivers for COPD patients, offering day-to-day support, managing acute episodes and enabling the patient to take a more active role in managing their condition.26 Research has demonstrated that nurse-led interventions significantly enhance COPD patients’ mental and physical well-being, as well as their quality of life.30,31 Furthermore, nurses ensure continuity of the care pathway. In this context, the experts suggested two actions to improve COPD management.
- 1)
Specialization of nursing personnel in COPD management. Training specialist nursing personnel in COPD management necessitates extensive education to furnish nurses with expert skills and knowledge in the complexities of COPD care. This expertise is crucial because it allows nurses to provide proactive care, potentially reducing hospital readmissions and enhancing patient quality of life. It also facilitates the registration and evaluation of patient-reported outcomes (PROMs) and patient-reported experiences measures (PREMs). Additionally, specialized nursing plays a key role in patient education, particularly in the correct use of treatments such as inhalers, which are essential for effective disease management and adherence.
- 2)
Implementation of the COPD nurse case manager role. This role is designed to bridge the gaps in care that patients often experience. A nurse case manager acts as a central point of contact for patients, coordinating with various healthcare professionals and ensuring that care plans are followed consistently and effectively. This function is crucial for gathering and managing data on patient health status, interventions, and results, information that is critical for determining the effectiveness of the COPD management plan and making required changes. Furthermore, the nurse case manager plays a key role in the early identification of patient deterioration and in organizing medical visits to prevent exacerbations, which is essential in reducing the risk of acute episodes and improving overall patient outcomes. It also enhances the ability of the healthcare system to monitor long-term outcomes and identify patterns or areas for improvement.
Clinical continuity across several healthcare settings is critical in managing chronic diseases such as COPD, including patient follow-up after discharge from hospitalization Experts have identified three main activities that improve continuity, ensuring that every stage of patient care is integrated and cohesive, resulting in better patient outcomes and quality of life.
- 1)
Implementation of a single shared medical history across all levels of healthcare
COPD patients frequently see many doctors, including primary care specialists, pulmonologists, internal medicine and emergency care teams among other specialities. With more than one caregiver involved, the patient may have many medical records that differ or have gaps in patient information. To prevent this, a universal health record should exist for all those involved in patients’ healthcare management. In that way, all physicians would have access to up-to-date and detailed patient information as needed, thereby increasing care quality.
- 2)
Protocols for referral to nursing consultation after the specialist visit for individualized patient education.
Enhancing the role of nursing in the follow-up of patients with COPD is crucial for improving their quality of life and clinical results. Comprehensive disease management may be significantly impacted by adopting follow-up procedures that underscore the roles that nursing staff play in patient follow-up, education, and training. Implementing nursing-led follow-up procedures can improve comprehensive care for COPD patients by providing more individualized and patient-centered care and serving as a resource for patients and other clinical professionals involved in their treatment.32
- 3)
Creation of effective communication channels among specialists involved in COPD management.
In order to guarantee that COPD patients receive coordinated and high-quality care, effective communication between various care levels is essential. Throughout the course of the patient's treatment, care continuity can be significantly enhanced by the creation and application of flexible communication channels between primary and inpatient care, and across various hospital specialties. The dissemination and use of agile communication channels can facilitate interprofessional collaboration and shared decision-making, promoting integrated and patient-centered care to improve clinical outcomes and patient satisfaction. In addition, the definition of a cross-cutting coordination figure with competences and decision-making autonomy in all healthcare areas would contribute very positively. As mentioned before when talking about the nurse case manager role, this integrative and unifying figure would act as a link between different healthcare professionals and services, facilitating communication and interdisciplinary collaboration.
DiscussionCARABELA-COPD provides a new framework for the optimization of COPD management in healthcare centers throughout Spain. It assesses the reality of the situation and develops plans for either optimizing current care processes or upgrading to advanced pathways in the patient journey. These strategies aim to reduce inefficiencies in the system, improve quality of life, and align with national plans, guidelines and recommendations.
So far, it has not been possible to establish a structure for the management of COPD in Spain due to the coordination and sharing of strategic initiatives among political and health authorities, scientific societies, health professionals, etc. The lack of genuine commitment to the national strategic plan is an added complication.6,12 In this context, the proposed actions reflect consensus-based, achievable priorities that can serve as the foundation for broader systemic improvements. While some recommendations may appear simple, they are designed to enable immediate implementation, recognizing the complexity of the Spanish healthcare system and the variability in local contexts.
CARABELA-COPD provides a tool that can define healthcare models and establish healthcare quality indicators to evaluate the achievement of the different objectives, generating local solutions with a real impact on the health of COPD patients (Fig. 2). This optimization process has been made possible thanks to the multidisciplinary work of three scientific societies, SECA (Spanish Society of Quality of Care), SEMI (Spanish Society of Internal Medicine) and SEPAR (Spanish Society of Pulmonology and Thoracic Surgery) in partnership with AstraZeneca. This approach will allow the entire community involved in COPD management to participate in this shift drive and to progressively alleviate the problems that have persisted year after year.
CARABELA-COPD is the prelude to the future and sets the foundation for an optimized patient journey in which barriers are addressed through actions to foster patient engagement, the widespread implementation of screening programs to detect COPD in early stages before significant lung damage occurs, and the broadening of the scope of training for healthcare professionals to achieve holistic management of COPD. In addition, this initiative offers the opportunity to regularly update and refine care protocols based on the results of ongoing program evaluations through health quality control indicators. Furthermore, areas of improvement and proposed solutions are being tailored locally (in different hospitals) through the Playbook—a digital tool that consolidates valuable project information for advancing COPD care. This tool was also developed to disseminate and apply the results obtained, enabling the implementation of specific solutions within each healthcare setting.
As previously discussed in the original publication describing the main results of CARABELA-COPD initiative,1 this model presents certain inherent limitations that must be acknowledged. Implementation of the proposed measures may face challenges such as regional heterogeneity, limited availability of specialized nursing, and sustainability issues in spirometry training due to staff turnover and resource constraints. Furthermore, the lack of direct representation from patient associations and nursing organizations in the current phase is a notable limitation; future iterations should ensure their active involvement to incorporate real-world perspectives and enhance the relevance and applicability of the recommendations.
ConclusionDespite numerous efforts, there is still much room for improvement in the early detection and management of COPD patients. By embracing the CARABELA-COPD mindset, each center could initiate its own optimization process, assess its circumstances, and set realistic goals to optimize its standards of care and thus improve the quality and consistency of COPD care in Spain. This program is a catalyst for change in the direction of comprehensive and integrated treatment for people with COPD, working toward the goal of maximizing diagnosis, management, and outcomes by coordinating efforts across healthcare settings. While many of the identified gaps are known, CARABELA-COPD provides a renewed stimulus and actionable roadmap for their effective implementation. CARABELA-COPD outcomes and solutions, such as the ones presented in this document as a guide, prioritize a united front in the efforts of all parties involved in COPD healthcare to create a more effective and patient-centered strategy.
FundingCARABELA-COPD is a co-organization accord between scientific societies and AstraZeneca Spain.
Authors’ contributionsJesús Díez-Manglano, Inmaculada Mediavilla, Luciano Escudero and Javier de Miguel-Díez participated in the conceptualization, drafting and writing of the manuscript. The final version of the manuscript has been reviewed and validated by all authors belonging to the CARABELA-COPD Scientific Committee.
Artificial intelligence involvementHe authors declare that they have not used artificial intelligence for generation or writing this manuscript.
Conflicts of interestInmaculada Mediavilla has received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from AstraZeneca, Novartis, Bristol-Myers-Squibb, Boehringer-Ingelheim, MSD, Pfizer, and Bayer; support for attending meetings and/or travel from Novartis and Pfizer; she is the President of the Spanish Society for Quality of Care. Jesús Díez-Manglano has received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from AstraZeneca, Bristol-Myers-Squibb, Esteve, GSK, and Boehringer-Ingelheim. Javier de Miguel-Díez has received grants or contracts from GSK and AstraZeneca; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from AstraZeneca, Bial, Boehringer, Chiesi, FAES, Ferrer, Gebro, GSK, Janssen, Menarini, Novartis, Roche, Teva and Pfizer; support for attending meetings and/or travel from AstraZeneca, Bial, Boehringer-Ingelheim, Chiesi, FAES, Gebro, GSK, Menarini, Novartis, Roche, Teva, and Pfizer; he is the COPD coordinator of the Spanish Society of Pulmonology and Thoracic Surgery. Juan Luis García has received grants or contracts from GSK and AstraZeneca; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from AstraZeneca, GSK, Gebro, Sanofi, Grifols and Chiesi; support for attending meetings and/or travel from AstraZeneca, GSK and Sanofi; he has participated in a Data Safety Monitoring Board or Advisory Board from AstraZeneca and GSK; he is the secretary of the Spanish Society of Pulmonology and Thoracic Surgery and the president of the Cantabrian Association for Respiratory System Research. Francisco Javier Medrano has received consulting fees from AstraZeneca; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from AstraZeneca. Francisco Casas-Maldonado has received consulting fees from AstraZeneca, CSL Behring, Grifols and GSK; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from AstraZeneca, Boehringer-Ingelheim, and CSL Behring; support for attending meetings and/or travel from AstraZeneca, Boehringer- Ingelheim, and CSL Behring. Ramón Boixeda has received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from AstraZeneca, Gilead, and GSK; support for attending meetings and/or travel from Chiesi and Gilead; he has participated in a Data Safety Monitoring Board and Advisory Board for Bayer. María Belén Alonso-Ortíz has received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from AstraZeneca, Bayer, Chiesi, FAES Farma, GSK and Nestlé Health Science and support for attending meetings and/or travel from Almirall, GSK and Novo Nordisk. Luciano Escudero, Carmen Corregidor, Eunice Fitas and Lucía Regadera are employees of the AstraZeneca Medical Department. Sergio Campos has no conflicts of interest to report.
The authors acknowledge the participation of all the professionals participating in the regional meetings of the CARABELA-COPD initiative, and of all those involved in the pilot phase of the CARABELA-COPD initiative from Hospital Álvaro Cunqueiro (Pontevedra, Spain), Hospital Clínico de Valencia (Valencia, Spain), Hospital Galdakao (Bizkaia, Spain), Hospital de Mieres (Asturias, Spain), Hospital La Paz (Madrid, Spain), Hospital El Bierzo (Ponferrada, Spain), Hospital Vall d’Hebron (Barcelona, Spain).
Medical writing support was provided under the guidance of the authors by Miriam Ejarque, PhD, Blanca Piedrafita, PhD and Vanessa Marfil, PhD from Medical Statistics Consulting (MSC), Valencia, Spain, and was funded by Astra Zeneca, Madrid, Spain, in accordance with Good Publication Practice (GPP3) guidelines.
The CARABELA-COPD Scientific Committee consists of the following members (listed alphabetically by last name): María Belén Alonso-Ortíz (Spanish Society of Internal Medicine), Ramón Boixeda (Spanish Society of Internal Medicine), Sergio Campos (Spanish Society of Pulmonology and Thoracic Surgery), Francisco Casas-Maldonado (Spanish Society of Pulmonology and Thoracic Surgery), Carmen Corregidor (AstraZeneca Farmacéutica Spain), Jesús Díez-Manglano (Spanish Society of Internal Medicine); Luciano Escudero (AstraZeneca Farmacéutica Spain), Eunice Fitas (AstraZeneca Farmacéutica Spain), Juan Luis García (Spanish Society of Pulmonology and Thoracic Surgery), Inmaculada Mediavilla (Spanish Society for Quality Care), Francisco Javier Medrano (Spanish Society of Internal Medicine), Javier de Miguel-Díez (Spanish Society of Pulmonology and Thoracic Surgery and Lucía Regadera (AstraZeneca Farmacéutica Spain).