Pulmonary nocardiosis is a rare opportunistic infection, often misdiagnosed due to its subacute onset and non-specific clinical and radiological findings. We report an 82-year-old man with severe chronic obstructive pulmonary disease (COPD) and bilateral bronchiectasis, who presented with progressive dyspnoea and productive cough unresponsive to conventional antibiotic therapy. Nocardia pneumoniae was isolated from bronchoalveolar lavage at ≥104CFU/mL. Initial treatment with trimethoprim–sulfamethoxazole (TMP–SMX) was discontinued due to renal impairment and electrolyte disturbances; minocycline was initiated with good tolerance and complete radiological resolution after six months. This case highlights the need to suspect nocardiosis in COPD and bronchiectasis patients, even without classical immunosuppression, particularly after repeated corticosteroid courses. Early diagnosis, communication with the microbiology laboratory, and targeted antibiotic therapy are key to improving outcomes.
La nocardiosis pulmonar es una infección oportunista poco frecuente, que a menudo se diagnostica erróneamente debido a su inicio subagudo, y a la inespecificidad de sus hallazgos clínicos y radiológicos. Presentamos el caso de un varón de 82 años con enfermedad pulmonar obstructiva crónica (EPOC) grave y bronquiectasias bilaterales, que acudió por disnea progresiva y tos productiva, sin respuesta a la antibioterapia convencional. Se aisló Nocardia pneumoniae en lavado broncoalveolar con una concentración≥104UFC/ml. El tratamiento inicial con trimetoprim-sulfametoxazol (TMP-SMX) se suspendió por deterioro de la función renal y alteraciones hidroelectrolíticas; se inició tratamiento con minociclina con buena tolerancia y resolución radiológica completa a los 6 meses. Este caso subraya la necesidad de sospechar nocardiosis en los pacientes con EPOC y bronquiectasias, incluso en ausencia de inmunosupresión clásica, especialmente tras cursos repetidos de corticoides. El diagnóstico precoz, la comunicación con el laboratorio de microbiología y la antibioterapia dirigida son claves para mejorar el pronóstico.
Pulmonary nocardiosis is an uncommon opportunistic infection, often misdiagnosed due to its subacute presentation and the non-specific nature of its clinical and radiological presentation.1
We present the case of an 82-year-old man with severe chronic obstructive pulmonary disease (COPD) (GOLD 3E) and bilateral bronchiectasis, who presented with progressive dyspnoea and productive cough without improvement after conventional antibiotic treatment.
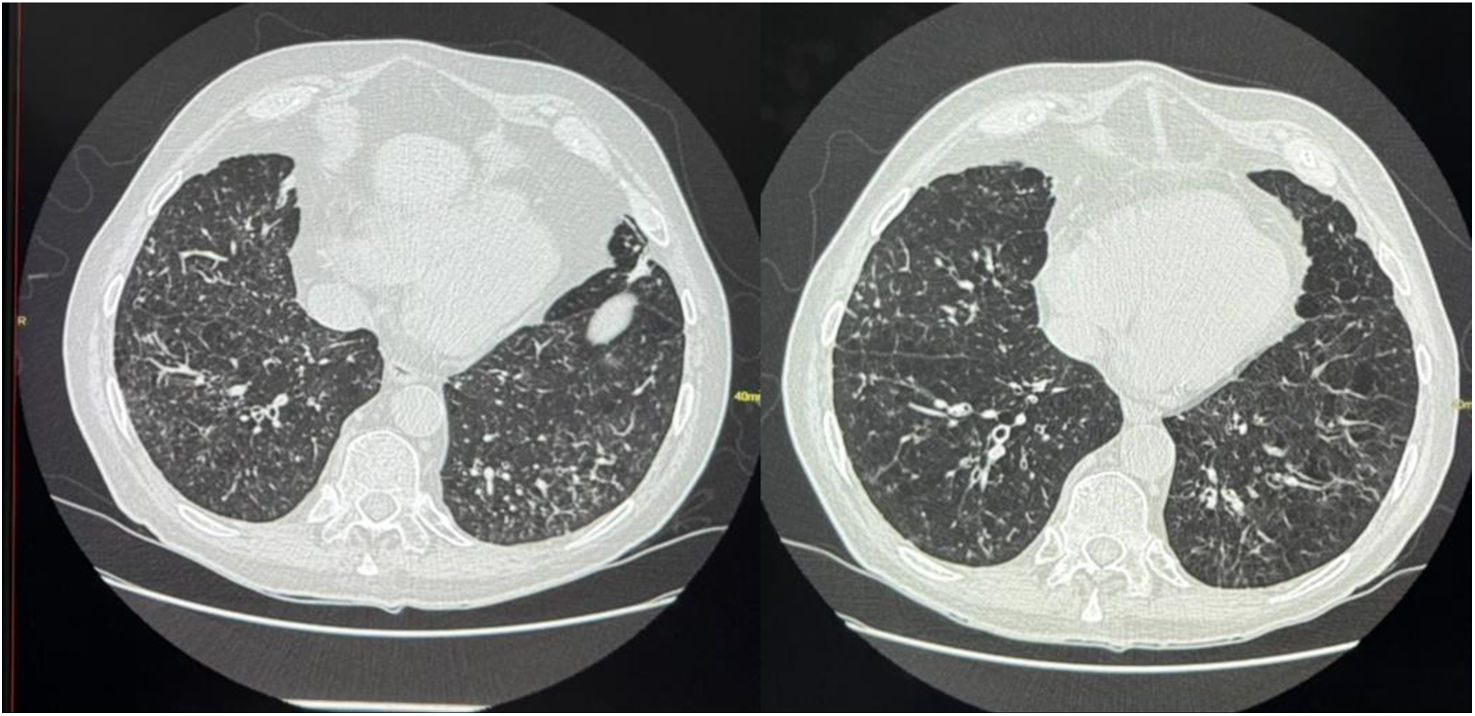
The patient had a history of multiple exacerbations with repeated use of oral corticosteroids. Follow-up chest CT revealed multiple peripheral acinar nodules bilaterally (Fig. 1A). Given the suspicion of atypical infection, fibrobronchoscopy with bronchoalveolar lavage (BAL) and bronchoaspiration was performed, isolating Nocardia pneumoniae at concentration of ≥104CFU/mL, a threshold considered diagnostic for pulmonary nocardiosis. Treatment with trimethoprim–sulfamethoxazole (TMP–SMX) was initiated but discontinued due to renal function deterioration and electrolyte disturbances. Minocycline 100mg every 12h for six months was then initiated, with good clinical tolerance. Follow-up after six months showed complete resolution of the nodular lesions (Fig. 1B), and the patient experienced no further exacerbations.
Chest CT scan after and before treatment. (A) Chest CT scan before treatment. Multiple acinar nodules with peripheral and bilateral distribution, some of which exhibit a halo of attenuation. (B) Follow-up chest CT scan after treatment: radiological improvement and resolution of nodular involvement.
The coexistence of COPD and bronchiectasis increases the risk of infection by uncommon pathogens, including Nocardia spp.2,3 Up to 40% of pulmonary nocardiosis cases have been reported in patients with chronic respiratory diseases.4–7 CT findings such as peripheral nodules, consolidations, or a nodular-bronchiectatic pattern should prompt consideration of atypical infections.5,8,9
Diagnosis requires a high level of suspicion, as clinical and radiological features can mimic tuberculosis or non-tuberculous mycobacterial disease.5,6,8 Microbiological confirmation through culture and molecular techniques is essential. Nocardia species are slow-growing, and their identification often requires prolonged incubation and specific laboratory protocols. This underscores the importance of alerting the microbiology laboratory when the infection is suspected, to ensure active search and appropriate culture conditions. For BAL, a threshold of ≥104CFU/mL is considered a reliable diagnostic criterion, offering greater specificity and helping differentiate colonization from active infection.5,10
In the present case, N. pneumoniae was isolated—an uncommon species within the genus—which highlights the value of species-level identification by molecular methods, both for clinical relevance and therapeutic guidance.
The treatment of choice for nocardiosis is TMP–SMX, with sensitivity rates of over 95% in most series, as in our case.4,5,10 In cases of intolerance, alternatives such as linezolid, minocycline, amikacin, or imipenem should be considered according to susceptibility profiles and disease severity.4,10 Treatment is recommended for at least six months, adjusted according to clinical response and the presence of immunosuppression or disseminated disease. In our patient, suspension of TMP–SMX due to renal impairment and the subsequent use of minocycline with good clinical response is consistent with published evidence supporting minocycline as an effective alternative in susceptible Nocardia infections.
The presence of bronchiectasis and COPD favours colonization and infection by Nocardia spp., even in the absence of classical immunosuppression, particularly in patients who have received multiple courses of systemic corticosteroids. Maintaining a high index of suspicion is therefore essential in patients with chronic respiratory diseases. Nocardiosis has been reported to both develop in patients with pre-existing bronchiectasis and contribute to its progression.5,10 It should therefore be considered in the comprehensive management of the patient, requiring a multidisciplinary approach and close follow-up.4,11
A multidisciplinary approach, microbiological testing and clinical-radiological follow-up have been key to the patient's favourable evolution. We consider that this case may be useful for other clinicians in similar situations.
In conclusion, nocardiosis should be included in the differential diagnosis of respiratory exacerbations in patients with COPD and bronchiectasis, especially in the presence of atypical radiological findings or poor clinical evolution. Early diagnosis and targeted treatment can significantly improve outcomes and they are essential for improving the prognosis, and the selection of the antibiotic regimen must be individualized according to the patient's sensitivity and comorbidities.
Informed consentOral informed consent was obtained from the patient for the publication of their clinical data and images.
FundingThis work did not receive any specific funding.
Authors’ contributionsAll authors contributed to the preparation, review, and approval of the final manuscript.
Artificial intelligence involvementNo generative artificial intelligence was used for the drafting, analysis, or editing of the scientific content of this manuscript.
Conflict of interestThe authors declare that they have no conflicts of interest.