Central pontine myelinolysis is an osmotic demyelination syndrome which, in the majority of cases, occurs after rapid correction of hyponatraemia.1 Alcoholism, malnutrition, the prolonged use of diuretics, and liver transplantation are associated with increased risk for developing this syndrome.2 Hypernatraemia and, to a lesser extent, hypokalaemia and treatment with magnesium or lithium have also been suggested as possible trigger factors together with hyponatraemia.3 We present the case of a patient who developed central pontine and extrapontine myelinolysis secondary to glycaemic fluctuations.
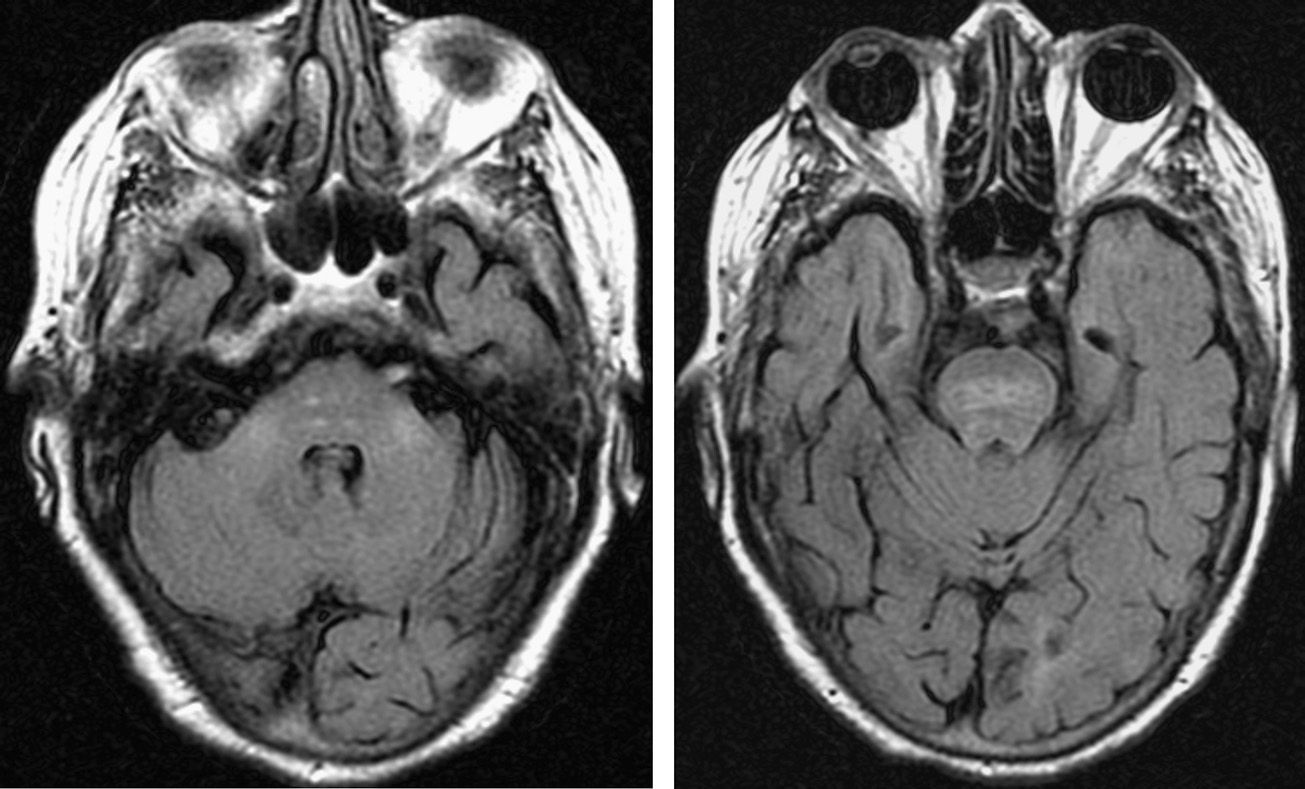
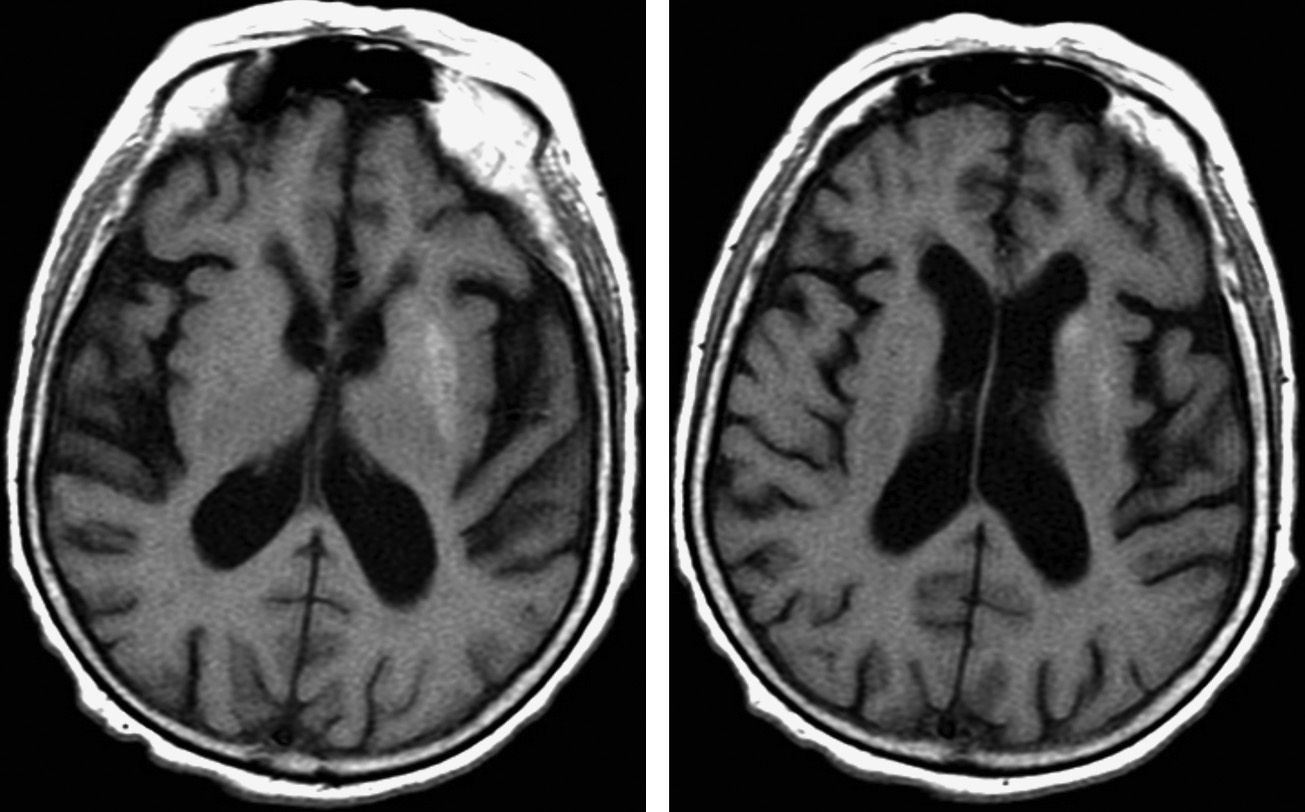
The patient was an 84-year-old woman who was found in her home with a low level of consciousness and hypoglycaemia (60mg/dL). Her medical history included arterial hypertension, dyslipidaemia, and type-2 diabetes mellitus; levels of glycated haemoglobin (11.5% 6 months before) suggested poor glycaemic control. The patient had presented at the emergency department 2 days previously with dizziness and nausea. Nonketotic hyperglycaemia (600mg/dL) was observed at that point and, as a consequence, the patient's normal insulin dose was increased. She lived alone and was independent, although in the preceding few months some self-neglect had become apparent, as the patient did not adhere to treatment and had poor hygiene habits. During the first few days after admission, our patient's level of consciousness improved. Three days later, she displayed no metabolic alterations and underwent a neurological examination where she was found to be alert but showed practically no initiative or voluntary activity. Extensor plantar response was observed bilaterally. The results from the examination of the sensory system and cranial nerves were normal. Spoken language, while infrequent, was normal and showed no signs of aphasia. Likewise, the patient displayed adequate verbal comprehension. Our patient's symptoms were therefore compatible with akinetic mutism; she also had signs of bilateral corticospinal dysfunction. A brain MRI revealed hyperintensities in the pons and both middle cerebellar peduncles in T2-weighted sequences (Fig. 1). These findings were suggestive of central pontine and extrapontine myelinolysis. The left lentiform nucleus and the head of the left caudate nucleus were also hyperintense in T1-weighted sequences (Fig. 2). None of these areas showed diffusion restriction in diffusion-weighted sequences. Blood analysis revealed glycated haemoglobin at 7.9% and fluctuations in glucose levels with hypoglycaemia as low as 21mg/dL and hyperglycaemia above 350mg/dL. The remaining parameters, including sodium level, were at all times within normal ranges. In the following weeks the patient improved to some extent and was more interactive and communicative, but continued to display apathy and a lack of initiative.
Pontine and extrapontine myelinolysis are usually due to a rapid correction of hyponatraemia. Several cases of hyperglycaemia and ketoacidosis associated with alterations in sodium levels1,4 have been reported in recent years, suggesting that hyperglycaemia associated with hyponatraemia should be added to the list of risk factors (alcoholism, malnutrition, etc.) for developing myelinolysis. Reports of isolated cases of severe hyperglycaemia5–8 or hypoglycaemia9,10 have also been published. Our patient displayed the typical radiological and clinical findings of pontine and extrapontine myelinolysis after correction of hyperglycaemia, and subsequently developed hypoglycaemia, which had to be further corrected. T1-weighted MRI sequences revealed hyperintensities in the lentiform and caudate nuclei, which is associated with nonketotic hyperglycaemia.11
The pathophysiology of myelinolysis includes astrocytic lesions and demyelination caused by fluctuations in osmolality,12 most commonly a rapid increase after a chronic state of low osmolality. We reported the case of a patient with poor glycaemic control and high glucose levels who experienced a sudden change in glucose levels leading to a sharp change in osmolality.
In conclusion, the clinical case described confirms that variations in plasma glucose levels can cause pontine and extrapontine myelinolysis as a result of abrupt shifts in osmolality. Likewise, our case supports the hypothesis that rapid changes in osmolality can play a role in the aetiopathogenesis of pontine and extrapontine myelinolysis, independently of the osmotic factor (sodium, glucose), and underscores the necessity of avoiding abrupt corrections of any metabolic alteration that may influence osmolality.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Matías-Guiu JA, Molino ÁM, Jorquera M, Jiménez R, Ruiz-Yagüe M. Mielinólisis pontina y extrapontina secundaria a fluctuaciones en la glucemia. Neurología. 2016;31:345–347.