Paediatric stroke is defined as stroke occurring in patients between one month and 18 years of age.1 Paediatric stroke is much less common than stroke in adults; however, morbidity (50% with serious neurological sequelae or epilepsy, with the ensuing socio-economic consequences),2 and mortality rates (15%-25%) are high.3 Fewer than 10% of paediatric strokes affect vertebrobasilar circulation.3 The typical form of presentation of paediatric basilar occlusion is a deterioration in the level of consciousness,4 which is the most common cause of locked-in syndrome.5 The wide range of clinical presentations and low incidence of this disorder lead to diagnostic delays in children.3 Paediatric basilar occlusion is frequently misdiagnosed as complicated migraine or epilepsy3 and its aetiology remains unknown in the majority of cases.3,4 No known treatment has been proven effective in randomised controlled clinical trials with children; what is known about this entity comes from isolated cases or case series.
Generally, in clinical practice, being younger than 18 years is an exclusion criterion for intravenous or intra-arterial thrombolysis.6,7 In the last few years, however, the excellent results of mechanical devices in adults8–10 (older retrievers or more recent models, such as stent retrievers) have opened the possibility of using these treatments for other indications.11,12 Such recent studies as the IMS-III, the SYNTHESIS, or the MR RESCUE,13–15 which failed to demonstrate the superiority of mechanical thrombectomy over ‘the best medical treatment available’, have been criticised for various design flaws, including the use of older retrievers (for example, the Merci) in place of stent retrievers, which have shown better recanalisation rates.
We present the case of a paediatric patient with a basilar occlusion effectively treated with stent retrievers and provide a brief review of the relevant literature.
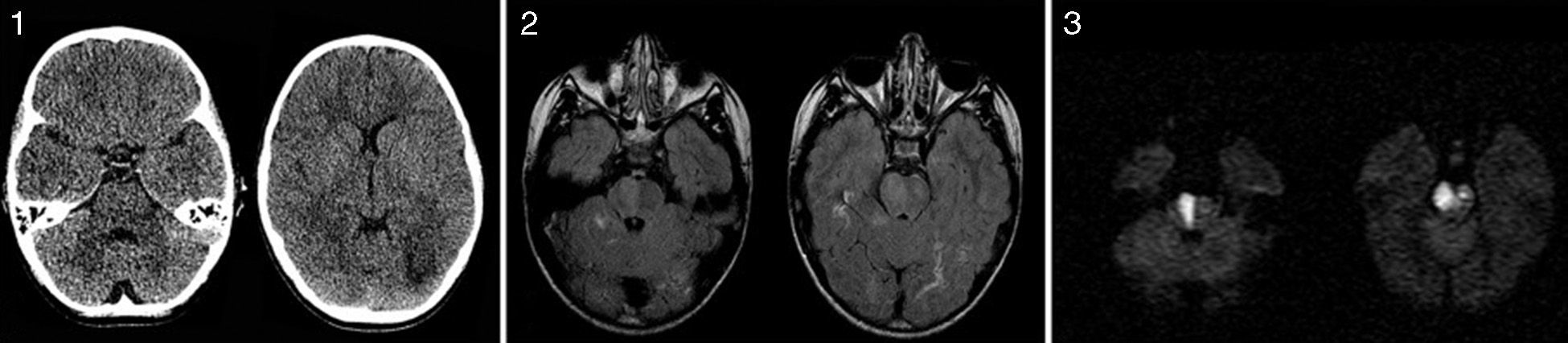
One month after a viral myositis, a 9-year-old boy presented at the emergency department with vomiting and rapidly progressive drowsiness. A neurological examination revealed a low level of consciousness, anarthria, skew deviation, and predominantly left-sided asymmetrical flaccid tetraparesis. Extensor plantar reflex was observed on the left foot, but there was no response on the right. His NIHSS score was 35 points. Laboratory test results were within normal limits. An emergency cranial CT scan revealed a small hypodense chronic lesion on the left subcortical occipital area, with no other relevant findings. The results from a lumbar puncture were also normal. The day after admission, the patient underwent a cranial MRI scan. T2-weighted sequences showed hyperintensities in the lumen of the basilar artery, and FLAIR sequences revealed the presence of hyperintense lesions compatible with ischaemic lesions in the pons and the white matter of the temporal and occipital lobes. The latter lesions showed different intensities in diffusion sequences as they were at a different stage of progression (Fig. 1).
(1) An emergency low-dose CT scan shows a small hypodense occipital subcortical lesion adjacent to the occipital horn of the left lateral ventricle, with no other relevant findings. (2) Brain MRI scan: an axial FLAIR sequence reveals hyperintense lesions compatible with ischaemic lesions on the pons and in white matter of the temporal and occipital lobes. (3) An axial DWI sequence (b=1000s/mm2) confirmed the presence of an acute ischaemic lesion on the pons, with markedly restricted diffusion. The left occipital and right temporal lesions are not hyperintense in the DWI sequence due to a longer progression time.
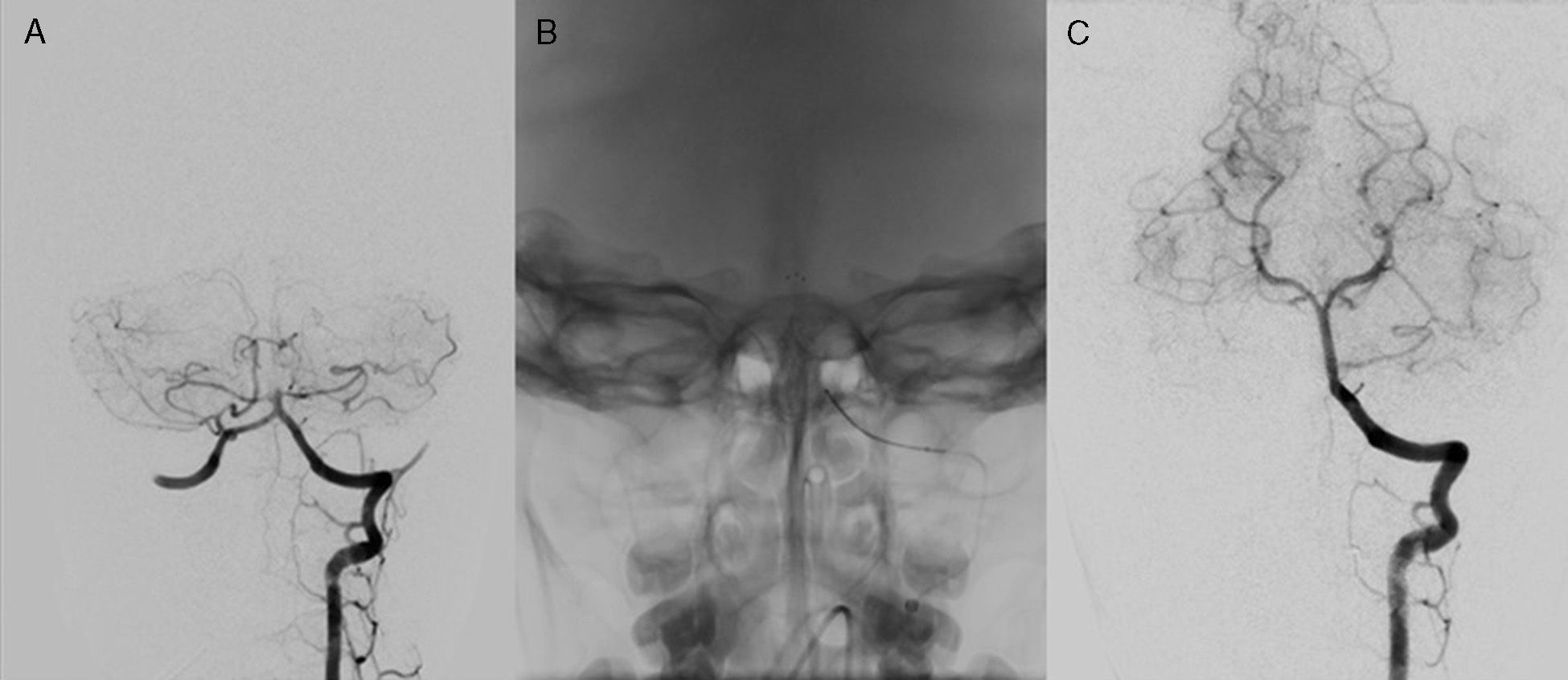
These findings raised suspicion of basilar thrombosis. Emergency CT angiography and perfusion CT scan were requested since we had not been able to satisfactorily assess MRI angiography and perfusion MR images due to a technical error. CT images revealed the presence of an occlusion at the level of the proximal portion of the basilar artery and an extensive area of penumbra in both occipital and temporal lobes. Mechanical thrombectomy was considered in view of the patient's poor clinical state. Thirty-six hours after symptom onset, our patient underwent a digital subtraction angiography through the femoral artery, which confirmed the presence of an occlusion in the proximal portion of the basilar artery. In light of these findings, the patient underwent a mechanical thrombectomy with stent retriever (Solitaire FR revascularisation device SFR-4-20, ev3, Irvine, CA, USA); the procedure achieved complete recanalisation of the basilar artery and all its distal branches (Fig. 2). The next day, a follow-up CT scan showed an established pontine infarction without haemorrhagic complications; the patient initiated treatment with low-molecular-weight heparin as an embolic aetiology was suspected. In the next few days, the patient began to improve and started rehabilitation. We conducted an aetiological study of the stroke, including a study of thrombophilia and vasculitis, serology tests, and transthoracic and transoesophageal echocardiography; the study yielded no conclusive results. The patient was discharged 16 days after symptom onset; he had a normal level of consciousness, and showed normal cranial nerves, mild dysarthria, mild left-sided dysmetria, mild left spastic hemiparesis (able to hold up the left arm for more than 10 seconds with minimal drift), and spasticity (NIHSS score=3).
Cerebral digital subtraction angiography, left vertebral artery injection, AP view. (A) Image taken before treatment confirming the occlusion of the middle third of the basilar artery. (B) Image taken during the procedure which shows the mechanical extraction device (stent retriever) open inside the basilar artery. (C) Final follow up image showing the recanalisation of the basilar artery and all its distal branches.
Paediatric basilar thrombosis manifests with severe symptoms and is associated with high morbidity and mortality rates. No treatment has proven to be safe and efficacious in randomised controlled clinical trials; the only experience we have is based on isolated cases or case series.16 Intravenous thrombolysis has demonstrated efficacy in some cases,1,17 but its use is limited due to the short treatment window (below 3-4.5 hours). Mechanical thrombectomy has the advantage of a longer treatment window and theoretically a lower risk of bleeding. However, until now no clinical studies have demonstrated its efficacy in children and its use is therefore still experimental.16
In a recent review article,16 the authors went over 63 published cases of basilar thrombosis in children. Of the 45 patients who did not receive intravascular treatment, 24 improved satisfactorily (53%), while 13 of the 18 who were treated showed good outcomes (72%). Despite this apparent positive tendency, interpreting these results is complicated since the term ‘intravascular treatment’ encompasses intra-arterial thrombolytic therapy, mechanical thrombectomy, and combined treatment.
In regards to mechanical thrombectomy, the literature reports 9 cases of basilar thrombosis treated with different mechanical devices, only 2 of which used stent retrievers.11,12 These devices were self-expanding stents of 3 to 6mm in length which deploy inside the thrombus and stick to it to then be removed with the thrombus inside. In adults, stent retrievers have been shown to be more effective than older devices,18 probably thanks to their larger area of contact. However, with reference to children only the 2 previously mentioned cases have been published.11,12
Ours is the first case in Spain and supports stent-retriever thrombectomy as a valid treatment for children with basilar thrombosis. In our patient, a 9-year-old male, clinical progression after stent-retriever thrombectomy was positive (baseline NIHSS score=35, NIHSS score on discharge=3) despite the diagnostic delay (the patient was outside the treatment window for intravenous thrombolysis) and the fact that thrombectomy was performed 36 hours after symptom onset.
In our view, in cases of basilar thrombosis there are various factors which give stent-retriever thrombectomy an advantage over methods which use older devices, especially the longer treatment window for the posterior territory (24-48 hours according to the literature, 36 hours in our case), greater speed, and higher recanalisation rates.18 These factors make mechanical thrombectomy with stent retrievers a viable treatment option in cases of paediatric basilar thrombosis when other treatments are ineffective or contraindicated. We must be mindful, however, that up to this point no randomised clinical trial has demonstrated the efficacy of mechanical thrombectomy in either adults or children.
Please cite this article as: Garnés Sánchez CM, Parrilla G, García Villalba B, Alarcón Martínez H, Martínez Salcedo E, Reyes Domínguez S. Oclusión basilar pediátrica tratada mediante trombectomía con stents extractores. Neurología. 2016;31:347–350.
This study was presented in poster format at the 65th Annual Meeting of the Spanish Society of Neurology on 22 November 2013.