Chronic constipation is a very common problem in the elderly. This can lead to fecal impaction and stercoral colitis, which can have high morbidity and mortality. Fecal impaction refers to the accumulation of hard feces in the rectum and colon that cannot be evacuated naturally. Due to the increasing pressure on the walls, it can produce distension, ischemia, necrosis, and ulcer. It has been studied that more than 70% of the people living in nursing homes present chronic constipation, and 47% of them have had fecal impaction according to patient history.1
We report the case of an 87-year-old woman with a history of mild cognitive impairment, atrial fibrillation, pacemaker carrier, cardiac failure, hypertension, hypothyroidism and used a wheelchair for mobility due to a hip fracture the year before. The patient was completely dependent for personal care, high risk of malnutrition, had double incontinence and lived in a nursing home. As a daily treatment, she was taking rosuvastatin (10mg od), bisoprolol (2.5mg bid), levothyroxine (100mcg od), furosemide (40mg od), calcifediol (1 tablet every 2 weeks), indapamide (2.5mg od), amiodarone (200mg od) and rivaroxaban (15mg od). The patient presented to the Emergency Department due to hyporexia and 11kg weight loss over the past 2 months. Physical examination revealed diffuse abdominal pain and a palpable hypogastric mass and the laboratory results showed metabolic alkalosis with hypokalemia (pH 7.56 [normal value – NV: 7.33–7.43]; pCO2 40.6mmHg [NV: 38–50]; HCO3− 36.3mmol/L [NV: 23–27]; K+ 1.9mmol/L [NV: 3.5–5.1]).
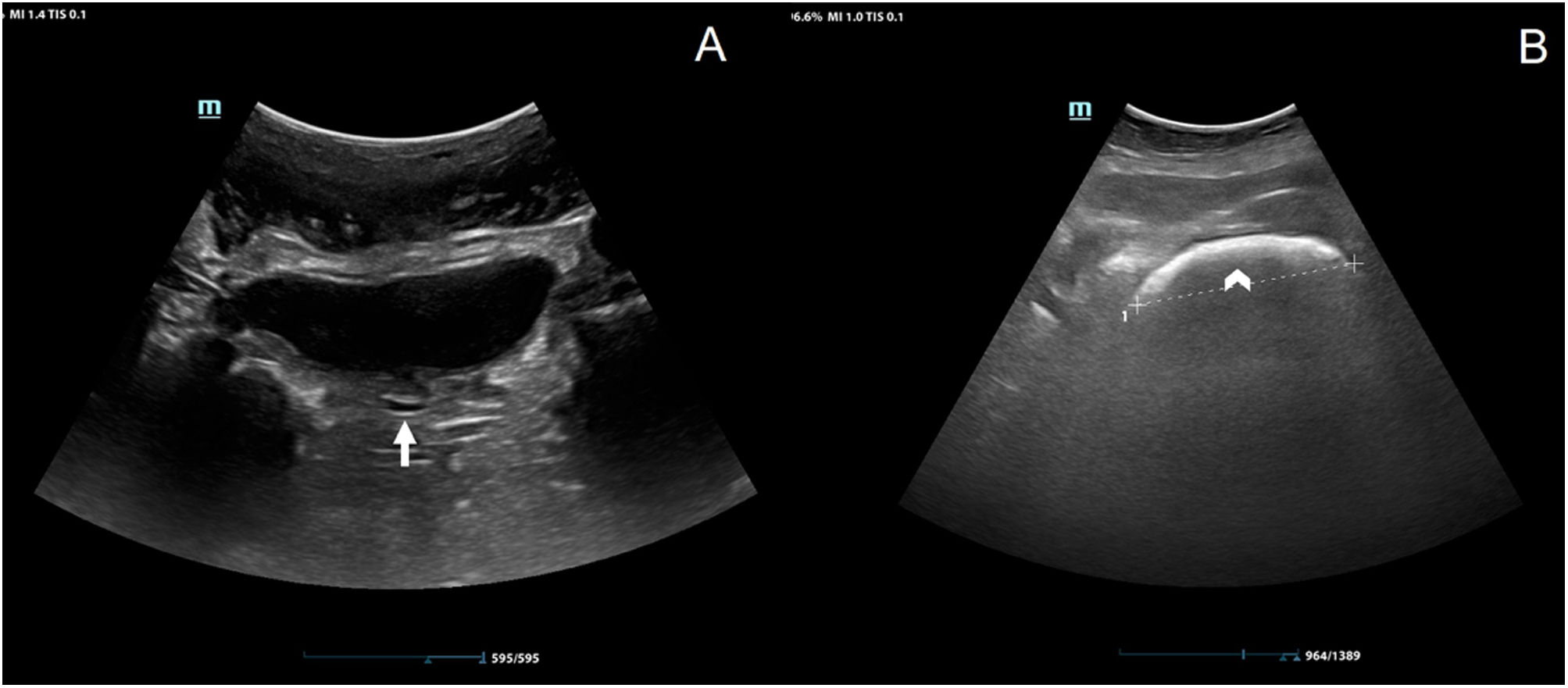
During hospitalization, she presented diarrhea (over 10 stools per day), whereby feces samples were taken for a polymerase chain reaction based fecal pathogen panel, with negative results. In this context, abdominal radiography was performed not showing relevant abnormalities besides feces in the recto-sigmoid area. As a complementary tool for enhanced physical examination, abdominal sonography was performed showing signs of fecal impaction, hence, facilitating the diagnosis (Fig. 1B). A manual extraction was performed, showing a decrease in the diameter of the rectum ampulla. Furthermore, an abdominal computed tomography (CT) was performed 3 days later, to further investigate the weight loss which confirmed fecal impaction in the rectum as well as copious feces through the colon. Unfortunately, the patient's clinical situation deteriorated and eventually died with bloody stools, probably due to stercoral colitis.
The evaluation of constipation and fecal impaction is based on the clinical history, which can be challenging in cognitively impaired patients, complemented with physical examination, including digital rectal examination.2 Abdominal radiography and computed tomography are the diagnostic tests typically recommended although they are not innocuous to the patient and they may not be readily available, especially in different settings such as home healthcare providers, nursing homes or long-term care facilities. In contrast, sonography is a low-cost and safe tool to evaluate fecal retention. This case shows the usefulness of sonography to diagnose and follow-up fecal impaction, as well as to raise awareness of the severity of this pathology. Prompt diagnosis is essential to control symptoms’ development and avoid clinical deterioration. Moreover, it also provides access to abdominal or rectal areas not reachable through a digital rectal examination as well as helps to narrow the differential diagnose of other abdominal conditions such as appendicitis, diverticulitis, etc.
Few studies have examined the use of sonography in the evaluation of constipation and fecal impaction. To perform the exam, the patient lies in a supine position, and the curvilinear or linear probe is placed in the abdomen, following a “mowing the lawn” scanning technique. The signs described in the literature, are a hyperechoic area shaped like a half-moon for fecal retention in the rectum with acoustic shadow for hard stool retention3 and increased rectum diameter (Fig. 1B). It has been shown that 92.9% of elder patients with an acoustic shadow on the crescent shape hyperechoic area had hard stools.4,5
Fecal impaction has already been described as fatal in the literature.4–6 Prevention and evaluation are of paramount importance in elder patients and even more in nursing homes. Some drugs are well-known causes of constipation and thus, special attention should be considered in polymedicated patients, such as the ones previously described. Although in our case, we lack a definitive diagnosis, and other causes could not be ruled out (i.e., ischemic or inflammatory colitis, enema complication, etc.), seems plausible the fecal impaction was a direct contributing factor to the fatal outcome.
In conclusion, sonography is not only a useful tool for the prompt diagnosis of fecal impaction but also for the evaluation of the therapy's effectiveness, both in hospital and nursing home settings because it allows the identification of constipation and fecal retention, even before symptoms appear, leading to a proper treatment instauration.
Informed consentInformed consent was obtained from the patient next of kin.
FundingInformed consent was obtained from the patient next of kin and protocols in the workplace regarding patient information treatment have been followed.
Conflict of interestThe authors declare that they have no conflict of interest.