Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosTo assess the effect of repetitive peripheral magnetic stimulation (rPMS) on improving insomnia and pain in patients with chronic low back pain.
MethodThe research method used an analytic experimental cross-sectional design for chronic NPB patients enrolled in Dr. Wahidin Sudirohusodo Hospital and Clinic Inggit Medical Center, from March to May 2019. rPMS was conducted and assessed the Insomnia Severity Index (ISI) and assessed the Numeric Pain Rating Scale (NPRS) before and after rPMS was performed. Samples were divided randomly into the control and treatment groups. A comparison of ISI and NPRS values before and after rPMS was performed with a paired t-test analysis.
ResultThere were 30 samples (15 controls and 15 treatments) with differences in ISI and NPRS scores in both groups of 5.00 (±2.10) and 1.80 (±0.68) in the treatment group and 0.93 (±1.33) and 1.07 (±0.26) in the control group. There was a significant improvement in ISI and NPRS values after rPMS was performed on chronic NPB.
ConclusionRepetitive peripheral magnetic stimulation affects improving insomnia and pain in patients with chronic lower back pain.
Sleep disturbances experienced by patients who experience chronic problems are of growing concern to researchers and are an important factor in the quality of human life. Improve research that has been done on the nature of pain and improve insomnia that occurs in chronic pain. Pain patients who complain of difficulty falling asleep, onset latency sleep longer, are more awake during sleep, sleep jam less, and sleep less soundly than uninjured patients.1
Insomnia is a form of sleep disorder that often occurs in patients with chronic low back pain (LPB). Among patients with chronic low back pain, the prevalence of insomnia ranges from 50% to 90%. Insomnia affects the quality of life, daily functioning, and recovery from pain in patients. Previous studies have examined the prevalence and severity of insomnia in patients with chronic LPB.2 Pain intensity is one of the most important factors associated with insomnia in patients with chronic musculoskeletal pain. One study found that pain intensity and fatigue were strongly associated with insomnia in patients with chronic LPB. Previous studies have shown that the intensity of pain, anxiety, and depression correlate significantly with insomnia in patients with chronic LPB.3
Insomnia or lack of sleep is also a common problem in developed countries. It is associated with difficulty in starting sleep, often waking up at night with difficulty returning to sleep, and waking up too early.4 Sixty-four million Americans suffer from sleep deprivation according to a report from the US health ministry. This data is 1.4 times more frequent in women. On the other hand, sleep quality has a close relationship with quality of life. Poor sleep quality affects mood, pain experiences, daily performance, and general quality of life.
The main problem in sufferers of low back pain is pain that will interfere with functional activities. Based on “Graying of America,” the problem of lower back pain will increase significantly in the future. In 2010, there were around 40.3 million Americans aged 65 years or older suffering from low back pain, which constituted 13% of the total population. By 2030, it is estimated that around 20% is the population aged 65 years or more. The onset of lower back pain is usually at the age of 20–60 years and mostly occurs in the middle age of 30–40 years. The peak incidence of low back pain is at the age of 45–60 years.5
Studies in the UK suggest that NPB is a major cause of disability in young adults, which causes more than 100 million workdays lost each year. Thus, LPB is a cause of decreased work productivity and is associated with a large economic burden. Low back pain is associated with high costs, including those related to health care and indirect costs of job loss or decreased productivity. The total cost of lower back pain in the United States was estimated at 100 billion dollars in 2006, two-thirds of which were indirect costs of lost wages and productivity.
Until now, management in patients with low back pain, both acute, subacute, and chronic, still use pharmacological therapy, non-pharmacological therapy, and surgical therapy. However, there are several obstacles, such as long-term use of drugs that can cause side effects, sufferers feel uncomfortable when advised to perform operative measures, as well as some cases of sufferers of low back pain who do not feel improvement in symptoms after performing operative action.6
Repetitive peripheral magnetic stimulation (rPMS) is a non-invasive treatment method that can penetrate deeper conductive structures with relatively painless stimulation. Of the various studies conducted since 1995, no studies have looked at side effects after getting rPMS. Thus, rPMS can be considered as a method of treatment with a high level of tolerance and safety. Due to various therapeutic effects, therapy is mainly indicated in musculoskeletal and neurological disorders.7
Repetitive peripheral magnetic stimulation (rPMS) is characterized by very deep penetration, the absence of current flowing through the skin, and the absence of high local current density. It avoids the activation of skin receptors such as nociceptors and receptor mechanisms. rPMS used in muscles induces proprioceptive flow to the central nervous system (CNS) in two different ways: First, indirect activation of sensory receptors due to stimulation-induced contraction and rhythmic relaxation and muscle vibration. It includes depolarization of the Ia, Ib, and II fiber groups. Second, direct activation of sensorimotor nerve fibers by orthodromic and antidromic conduction. In addition, it has been proven that rPMS is a potential treatment option for muscle relaxation, and rPMS can activate the process of modulation and plasticity on CNS. rPMS has been used in patients with chronic low back pain in four studies. rPMS is considered a promising method of treatment from various perspectives. Due to various therapeutic effects, therapy is mainly indicated in musculoskeletal and neurological disorders.8
MethodsResearch designThis study is an experimental analytic study with a cross-sectional design that assesses the effect of repetitive peripheral magnetic stimulation on insomnia and pain in chronic low back pain patients. The study was conducted at Dr. Wahidin Soedirohusodo Hospital and Inggit Medical Center Clinic.
Research populationThe study population was all chronic low back pain patients who experienced insomnia and pain who went to the Neurology Polyclinic at Wahidin Sudirohusodo Hospital and the Inggit Medical Center Clinic in March to May 2019.
Research samples and ways of taking samplesThe sample of this study is chronic low back pain patients who experience insomnia and pain by meeting the inclusion and exclusion criteria. Samples are obtained by consecutive sampling method in accordance with the conditions or sample requirements of specific populations that are most easily reached or obtained.
Inclusion and exclusion criteriaThe inclusion criteria of this study were patients with chronic low back pain based on clinical manifestations, and MRI results are Hernia Nucleus Pulposus, Insomnia Severity Index (ISI) Score ≥8, Numeric Pain Rating Scale (NPRS) ≥4, and willing to be included in this study by signing informed consent. The exclusion criteria were chronic NPB patients who have had surgical intervention, Chronic NPB patients caused by trauma or malignancy, and kidney stones.
Data collection began when chronic low back pain patients were treated at the Neurology Polyclinic at Wahidin Sudirohusodo Hospital and Inggit Medica Center Clinic. Patients were given the Insomnia Severity Index (ISI) questionnaire to determine whether they had insomnia and to assess the pain scale with the Numeric Pain Rating Scale (NPRS). Patients were given repetitive peripheral magnetic stimulation for 30min for five cycles. The data collected was then analyzed with Statistical Product and Service Solutions (SPSS) version 25.
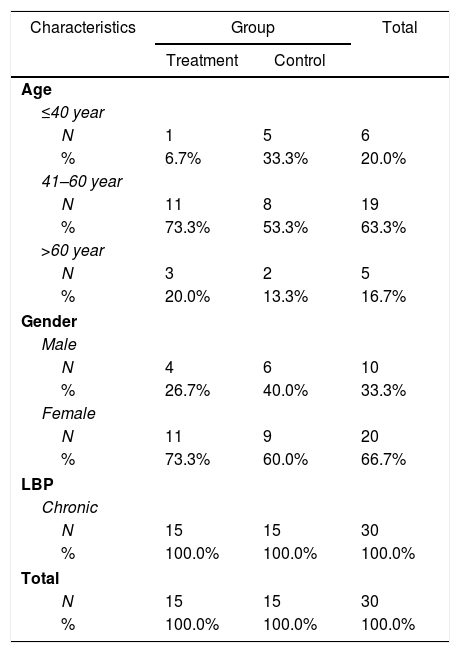
ResultsThis research was conducted at the Wahidin Sudirohusodo General Hospital for Education and the Inggit Medica Clinic in March to May 2019. In this study, the number of samples that met the inclusion criteria fulfilled 30 samples where the baseline data characteristics of the study sample showed the age distribution of the sample with the age group ≤40 years. Totaling 6 people, age group 41–60 years totaling 19 people, age group >60 years totaling five people. Based on Table 1, there were 20 female sex samples (66.7%) and ten female samples (33.3%).
Demographic characteristics of samples.
| Characteristics | Group | Total | |
|---|---|---|---|
| Treatment | Control | ||
| Age | |||
| ≤40 year | |||
| N | 1 | 5 | 6 |
| % | 6.7% | 33.3% | 20.0% |
| 41–60 year | |||
| N | 11 | 8 | 19 |
| % | 73.3% | 53.3% | 63.3% |
| >60 year | |||
| N | 3 | 2 | 5 |
| % | 20.0% | 13.3% | 16.7% |
| Gender | |||
| Male | |||
| N | 4 | 6 | 10 |
| % | 26.7% | 40.0% | 33.3% |
| Female | |||
| N | 11 | 9 | 20 |
| % | 73.3% | 60.0% | 66.7% |
| LBP | |||
| Chronic | |||
| N | 15 | 15 | 30 |
| % | 100.0% | 100.0% | 100.0% |
| Total | |||
| N | 15 | 15 | 30 |
| % | 100.0% | 100.0% | 100.0% |
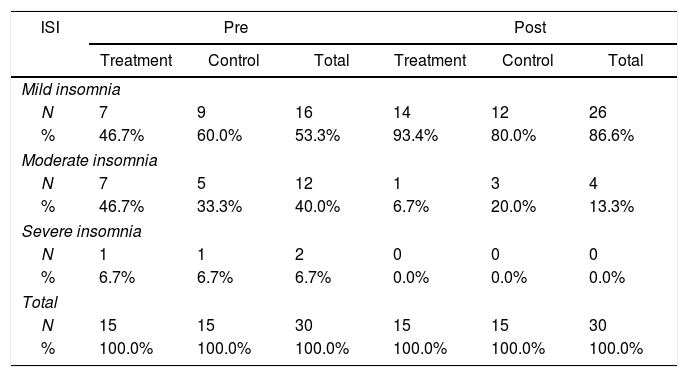
In Table 2 shows the degree of insomnia with pretest mild insomnia category amounted to 16 people (53.3%), while the posttest amounted to 26 people (86.6%). For moderate insomnia, pretest is 12 people (40.0%), posttest is 4 people (13.3%). Pretest severe insomnia was two people (6.7%). The Posttest severe degree of insomnia was 0 people (0.0%).
Description of the pretest and posttest Insomnia Severity Index (ISI) values.
| ISI | Pre | Post | ||||
|---|---|---|---|---|---|---|
| Treatment | Control | Total | Treatment | Control | Total | |
| Mild insomnia | ||||||
| N | 7 | 9 | 16 | 14 | 12 | 26 |
| % | 46.7% | 60.0% | 53.3% | 93.4% | 80.0% | 86.6% |
| Moderate insomnia | ||||||
| N | 7 | 5 | 12 | 1 | 3 | 4 |
| % | 46.7% | 33.3% | 40.0% | 6.7% | 20.0% | 13.3% |
| Severe insomnia | ||||||
| N | 1 | 1 | 2 | 0 | 0 | 0 |
| % | 6.7% | 6.7% | 6.7% | 0.0% | 0.0% | 0.0% |
| Total | ||||||
| N | 15 | 15 | 30 | 15 | 15 | 30 |
| % | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% |
ISI: Insomnia Severity Index.
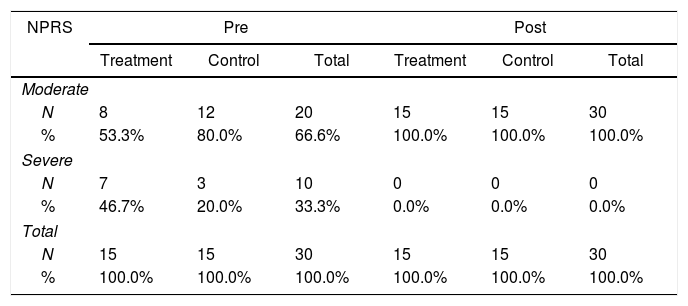
In Table 3, It can be seen the results of moderate pain in the pretest treatment group amounted to 20 people (66.6%), and the posttest amounted to 30 people (100.0%). As for the severe depression in the pretest control group amounted to 10 people (33.3%) and posttest amounted to 0 people (0.0%).
Description of the pretest and posttest Numeric Pain Rating Scale (NPRS).
| NPRS | Pre | Post | ||||
|---|---|---|---|---|---|---|
| Treatment | Control | Total | Treatment | Control | Total | |
| Moderate | ||||||
| N | 8 | 12 | 20 | 15 | 15 | 30 |
| % | 53.3% | 80.0% | 66.6% | 100.0% | 100.0% | 100.0% |
| Severe | ||||||
| N | 7 | 3 | 10 | 0 | 0 | 0 |
| % | 46.7% | 20.0% | 33.3% | 0.0% | 0.0% | 0.0% |
| Total | ||||||
| N | 15 | 15 | 30 | 15 | 15 | 30 |
| % | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% |
Numeric Pain Rating Scale (NPRS).
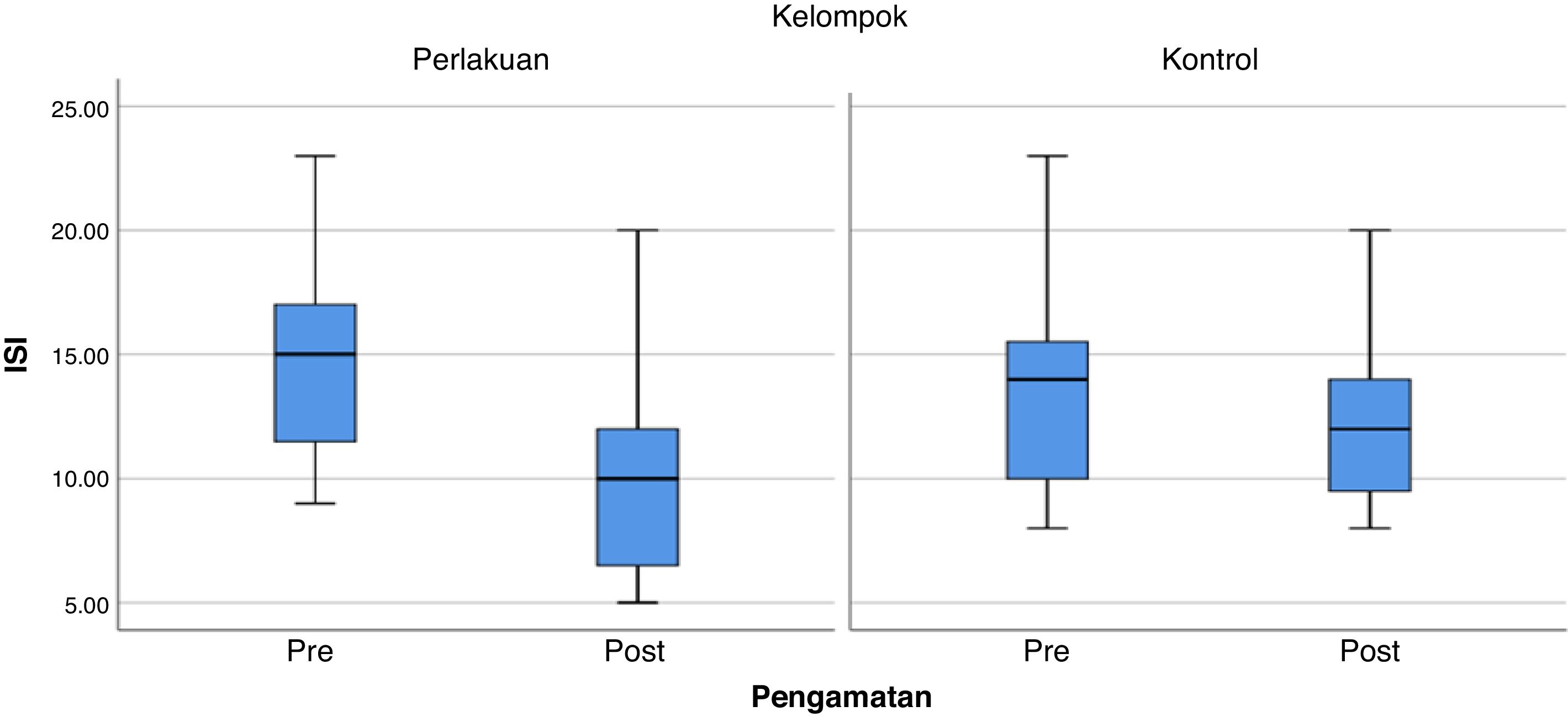
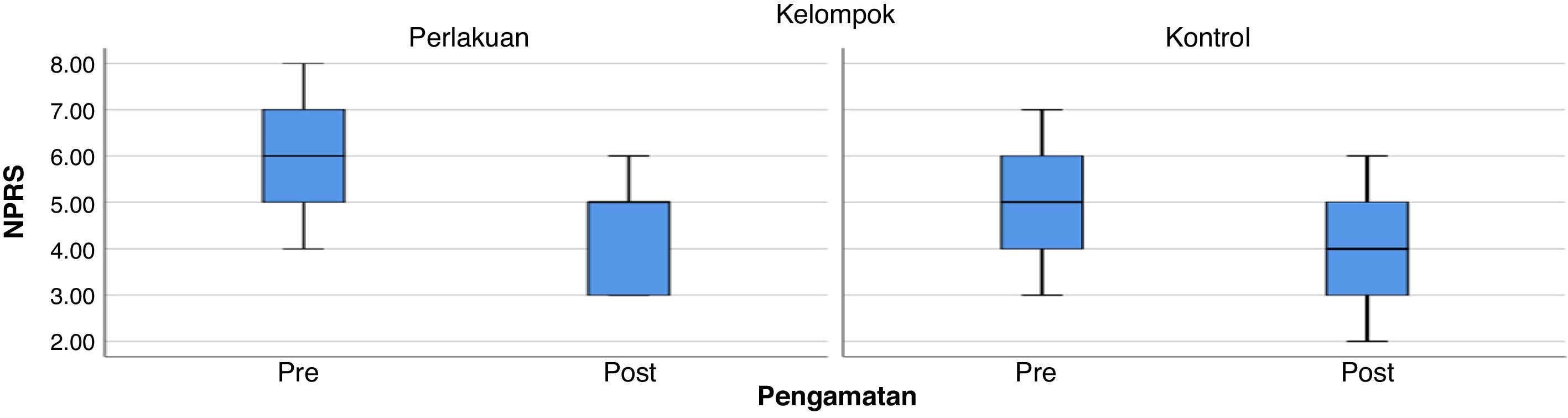
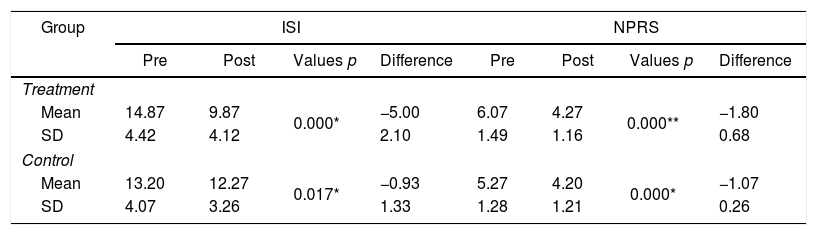
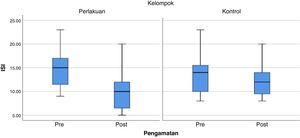
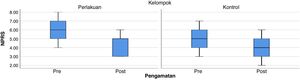
Based on Table 4, it can be seen the average test results of Insomnia Severity Index (ISI) in the pretest treatment group 14.87±4.42, and posttest 9.87±4.12, for the average Insomnia Severity Index (ISI) in the group pretest control 1320±4.07, and posttest 12.27±3.26. As for the average Numeric Pain Rating Scale (NPRS) test results in the pretest treatment group 6.07±1.49, and posttest 4.27±1.16, for the average Numeric Pain Rating Scale (NPRS) respectively in the control group pretest 5.27±1.28, and posttest 4.20±1.21 (Graphs 1 and 2).
Description of ISI and NPRS pretest and posttest values.
This study assessed the effect of repetitive peripheral magnetic stimulation on insomnia and pain in chronic low back pain patients. Insomnia scores were obtained from the Insomnia Severity Index (ISI) questionnaire. ISI is an instrument used to determine the severity of insomnia experienced by patients clinically. Pain assessment uses the Numeric Pain Rating Scale (NPRS). The NPRS is a useful scale for assessing the patient's degree of pain. Chronic NPB patients who enter the inclusion criteria are chronic low back pain caused by hernia nucleus pulposus (HNP), which is diagnosed by clinical symptoms and MRI results.5
This study uses ISI (Insomnia Severity Index) and NPRS (Numeric Pain Rating Scale) scores. Chronic LPB patients who had ISI scores ≥8 and NPRS ≥4. The number of samples that met the inclusion criteria were 30 people consisting of 15 treatment and 15 control people. From the 30 samples, there were more women (66.7%) than men (33.3%). Based on the age distribution, this study found that the number of samples was higher at the age of above 40 years compared to those under the age of 40 years. It is following several studies that show that the epidemiology of chronic low back pain occurs most often at the age of more than 40 years.1
Insomnia is a form of sleep disorder that often occurs in patients with chronic low back pain (LPB). Among patients with chronic low back pain, the prevalence of insomnia ranges from 50% to 90%. Insomnia or lack of sleep is also a common problem in developed countries. Characterized as difficulty in starting sleep, often waking up at night with difficulty returning to sleep, and waking up too early.3 Data obtained from the measurement results were analyzed using a paired t-test with a significance level of 5%. The t-test produces a calculated t value and a probability value (p) that can be used to prove the hypothesis that there is or no significant influence. The way to determine whether or not significant is if the p-value <0.05, then there is a significant difference, then if p>0.05, then there is no significant difference, the results of the analysis using the SPSS version 25. In this study, the results show that there is a repetitive effect of peripheral magnetic stimulation on improvement insomnia and pain in chronic low back pain patients with the Insomnia Severity Index where values (p=0.000) and Numeric Pain Rating Scale (p=0.000), there are significant differences.
Repetitive peripheral magnetic stimulation (rPMS) is a non-invasive treatment method that can penetrate deeper conductive structures with relatively painless stimulation. Besides, it has been proven that rPMS is a potential treatment option for muscle relaxation and rPMS can activate the process of modulation and plasticity in CNS. rPMS has been used in patients with chronic low back pain in four studies. Although there is still little research using rPMS, it is a non-invasive therapeutic approach that has pain relief effects, so it is considered a promising treatment method from various perspectives. Given the better treatment results, it is recommended for lower back pain with the effect of muscle relaxation and reduce pain. With reduced pain, the quality of sleep will improve and increase patient productivity (Young Ho et al. .2018).
ConclusionsBased on the results of the analysis of the research data above, it can be concluded that the repetitive peripheral magnetic stimulation influences the improvement of insomnia and pain in chronic low back pain patients.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.