Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosTo compare differences in quality of life in epilepsy patients with and without sleep disorders.
MethodsAn analytic comparative observational method with a cross-sectional study was conducted to patients that have been diagnosed with epilepsy for at least one year. The sample was derived using a consecutive sampling method with inclusion criteria at the RSUP Dr. Wahidin Sudiohusodo, collaborative hospital, and private practice in April–May 2019. Independent variable: quality of sleep assessed by the Pittsburgh Sleep Quality Index (PSQI) questionnaire. Dependent variable: insomnia assessed by Insomnia Severity Index (ISI) and quality of life assessed by Quality of Life in Epilepsy-31 (QOLIE-31). Statistical analysis was conducted using the unpaired t-test, Mann–Whitney test, and Chi-square test.
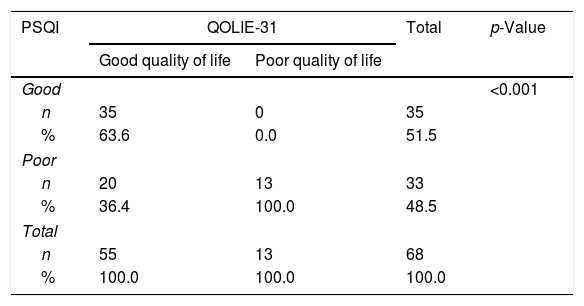
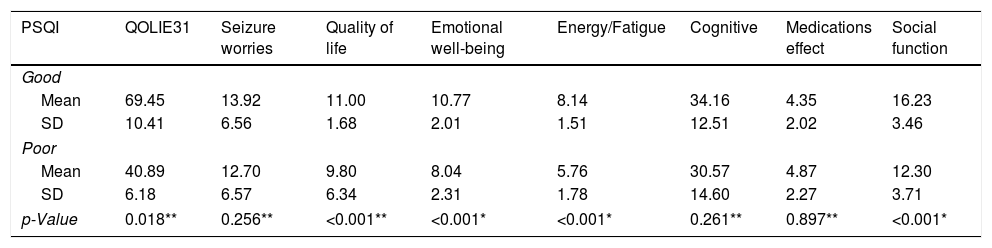
ResultsSixty-eight subjects met the inclusion criteria; 35 subjects with good sleep quality and 33 subjects with poor sleep quality, consist of 5 subjects with no clinically significant insomnia, 16 subthreshold insomnia, nine moderate insomnia, and three severe insomnia. The results showed a significant difference between 2 groups (p=0.018). A significant difference (p=<0.01) can be seen in the component of overall quality of life, emotional well-being, energy/fatigue, and social function. While in seizure worry (p=0.256), cognitive (p=0.261) and medication effects (p=0.897) the differences were not statistically significant.
ConclusionThere are differences in the quality of life of epileptic patients with and without sleep disturbance. Epileptic patients with sleep disturbance have a poorer quality of life compared to epileptic patients without sleep disturbance.
Epilepsy is a brain disorder characterized by a tendency to cause epileptic seizures that are continuous, with neurobiological, cognitive, and social consequences. In contrast, epileptic seizures occur for a momentary sign and symptom due to abnormal and excessive neuronal activity in the brain.1,2 Epilepsy is a chronic disease that is found in 0.5–1% of the total population. According to WHO, an estimated 50 million people worldwide have epilepsy. The prevalence and incidence of epilepsy in Indonesia are not known with certainty. The results of the Epilepsy Study Group of the Indonesian Neurologist Specialist Association in several hospitals in 5 major islands in Indonesia (2013) found 2288 people with epilepsy with 21.3% new patients.3
The most common age is the productive age, with the most common etiology of epilepsy is a head injury, central nervous system infections, strokes, and brain tumors. Poor sleep can induced seizures. Sleep is a physiological and recurring form of reversal of consciousness that reverses a decline in cognitive function globally so that the brain does not respond adequately to the surrounding stimulus. The average sleep cycle starts from phase 1 NREM followed by phase 2, then SWS after that returns to phase 2 and continues with the REM cycle. In healthy adults, this cycle can occur 5–7× each sleep period. The cycle time is around 90min, and in general, the first cycle occurs the shortest compared to other cycles. In 1/3 of the sleep period, the SWS predominates, whereas the first REM usually occurs 70–90min after sleep begins. In adults experiencing 2–5% of the sleep period is in phase 1 NREM, 45–55% in phase 2, 13–23% in the SWS phase, and 20–25% in the REM phase.4,5 The duration and distribution of the sleep phases vary at each age of human life. In stone born babies, the duration of each cycle lasts for approximately 60min, whereas in young adults, approximately 90min. Sleep duration decreases according to a person's age (Table 1).
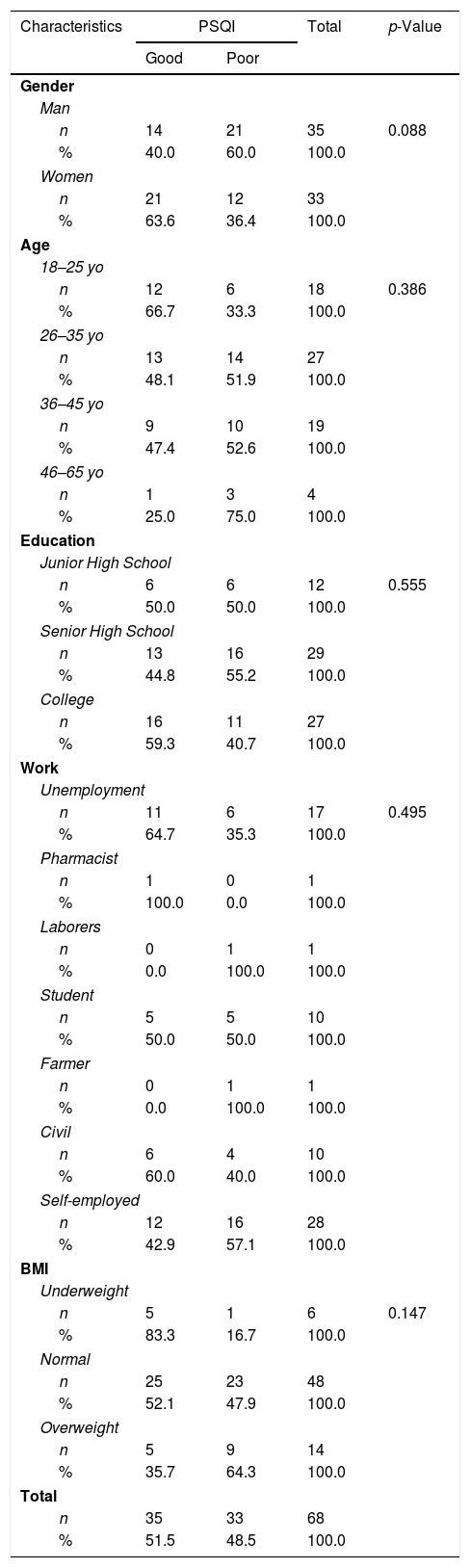
The characteristics of the research subjects are related to PSQ.
| Characteristics | PSQI | Total | p-Value | |
|---|---|---|---|---|
| Good | Poor | |||
| Gender | ||||
| Man | ||||
| n | 14 | 21 | 35 | 0.088 |
| % | 40.0 | 60.0 | 100.0 | |
| Women | ||||
| n | 21 | 12 | 33 | |
| % | 63.6 | 36.4 | 100.0 | |
| Age | ||||
| 18–25 yo | ||||
| n | 12 | 6 | 18 | 0.386 |
| % | 66.7 | 33.3 | 100.0 | |
| 26–35 yo | ||||
| n | 13 | 14 | 27 | |
| % | 48.1 | 51.9 | 100.0 | |
| 36–45 yo | ||||
| n | 9 | 10 | 19 | |
| % | 47.4 | 52.6 | 100.0 | |
| 46–65 yo | ||||
| n | 1 | 3 | 4 | |
| % | 25.0 | 75.0 | 100.0 | |
| Education | ||||
| Junior High School | ||||
| n | 6 | 6 | 12 | 0.555 |
| % | 50.0 | 50.0 | 100.0 | |
| Senior High School | ||||
| n | 13 | 16 | 29 | |
| % | 44.8 | 55.2 | 100.0 | |
| College | ||||
| n | 16 | 11 | 27 | |
| % | 59.3 | 40.7 | 100.0 | |
| Work | ||||
| Unemployment | ||||
| n | 11 | 6 | 17 | 0.495 |
| % | 64.7 | 35.3 | 100.0 | |
| Pharmacist | ||||
| n | 1 | 0 | 1 | |
| % | 100.0 | 0.0 | 100.0 | |
| Laborers | ||||
| n | 0 | 1 | 1 | |
| % | 0.0 | 100.0 | 100.0 | |
| Student | ||||
| n | 5 | 5 | 10 | |
| % | 50.0 | 50.0 | 100.0 | |
| Farmer | ||||
| n | 0 | 1 | 1 | |
| % | 0.0 | 100.0 | 100.0 | |
| Civil | ||||
| n | 6 | 4 | 10 | |
| % | 60.0 | 40.0 | 100.0 | |
| Self-employed | ||||
| n | 12 | 16 | 28 | |
| % | 42.9 | 57.1 | 100.0 | |
| BMI | ||||
| Underweight | ||||
| n | 5 | 1 | 6 | 0.147 |
| % | 83.3 | 16.7 | 100.0 | |
| Normal | ||||
| n | 25 | 23 | 48 | |
| % | 52.1 | 47.9 | 100.0 | |
| Overweight | ||||
| n | 5 | 9 | 14 | |
| % | 35.7 | 64.3 | 100.0 | |
| Total | ||||
| n | 35 | 33 | 68 | |
| % | 51.5 | 48.5 | 100.0 | |
In adults, the duration of sleep lasts between 7.5 and 8h each day. Recent research shows that the global effects of epilepsy are quite high. Surveys show that patients with epilepsy have the opportunity to have a lower quality of life than the general population. Sleep disorders in people with epilepsy are 2–3 times more frequent than in the general population.3 Sleep disorders are generally not too problematic for healthy people, but a considerable influence on patients with chronic diseases, especially in patients with epilepsy, the consequences are more severe, sleep deprivation can cause memory dysfunction, severe drowsiness during the day, and directly can contribute to the emergence of seizures. The causes of sleep disorders in epilepsy patients are similar to the average population in general, such as lack of sleep, sleep-hygiene.4 During epilepsy seizures, abnormal electrical discharges occur that synchronize in the local area or throughout the brain. The observation supports the effect of sleep on epilepsy that in specific epilepsy syndromes, seizures occur in the NREM phase, and in all epilepsy syndromes, the interictal epileptic discharge is more common in the NREM phase than in the REM phase.6
Neuronal synchronization in the thalamocortical pathway during the NREM phase causes more even neuronal excitability, and this can facilitate seizures in most partial epilepsy. Neuronal synchronization stops when waking up or transitioning to REM. Sleep disturbance in epilepsy patients can directly or indirectly affect the quality of life of patients, which can be measured by one measuring instrument in the form of a questionnaire called QOLIE-31. QOLIE-31 is a questionnaire that has been studied and proven useful in determining the quality of life of epilepsy patients. Therefore, researchers want to compare the quality of life of epilepsy patients who have sleep disorders compared with epilepsy patients without sleep disorders using the QOLIE-31 questionnaire. Based on the description above, the researcher wants to conduct a study that examines the comparison of the quality of life of epilepsy patients with sleep disorders and without sleep disorders.3,4,6,7
MethodResearch designThis research is a type of observational comparative analytic study using cross-sectional studies. The affordable population is all patients with epilepsy who seek treatment at the Nerve Poly Wahidin Sudirohusodo Education Hospital and Network Hospital, as well as private practices in April–May2019.
Samples were taken from the study population based on the order of admission to the hospital (consecutive sampling). The sample size required for two-sided testing is obtained by the formula (Lemeshow, 1997) with a minimum sample of 24 people per group.
Research samples and sampling techniquesThe study was conducted at the Neurology Polyclinic at Wahidin Sudirohusodo General Hospital, Network Hospital, and private practice in April–May 2019. The sample of this study was epilepsy sufferers, who met the inclusion criteria. The sample is obtained by consecutive sampling method, which is taking a sample that is in accordance with the conditions or requirements of the sample from a particular population that is most easily reached or obtained.3
ResultThe total research subjects who met the inclusion criteria were 68 people, from a minimum sample of 24 subjects from each group. Baseline data from the study subjects showed that the male and female gender composition in this study was almost balanced, with 35 men (51.5%) and 33 women (48.5%), with the highest age distribution at ages 26–35 in 27 subjects (39.7%), then 18–25 years were 18 subjects (26.5%), and in the age group, 46–50 subjects were four people (5.9%).
The highest level of education is senior high school, which is 29 subjects (42.6%), where most of the research subjects are private or independent workers. A total of 40 study subjects (58.8%) underwent epilepsy treatment under ten years. The number of seizures in the last one month was grouped into three groups, namely <1× monthly generation, 1–5× monthly and >5× monthly, and the highest number of subjects in the study with 1–5× monthly frequency was 34 subjects (50%).
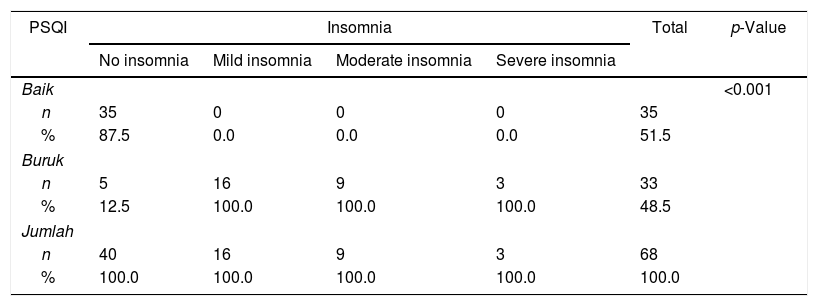
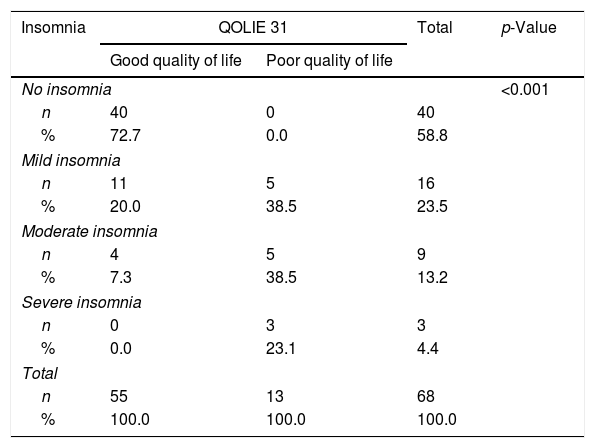
Most of our research subjects had a normal BMI of 48 subjects (70.6%). Of 68 research subjects, 35 people (51.5%) had good sleep quality, while as many as 33 people (48.5%) research subjects had poor quality. From 33 people with poor sleep quality, five people did not have insomnia (15.2%), 16 people with mild insomnia (48.5%) had mild insomnia, nine people had moderate insomnia (27.3%), and 3 had severe insomnia (4.4%). Overall, there were 55 subjects with good quality of life and (80.9%) and 13 people had poor quality of life (19.1%), all of whom were insomnia patients, 5 of whom were mild insomnia (38.5%), five moderate insomnia (38.5%) and three severe insomnia (23.1%)
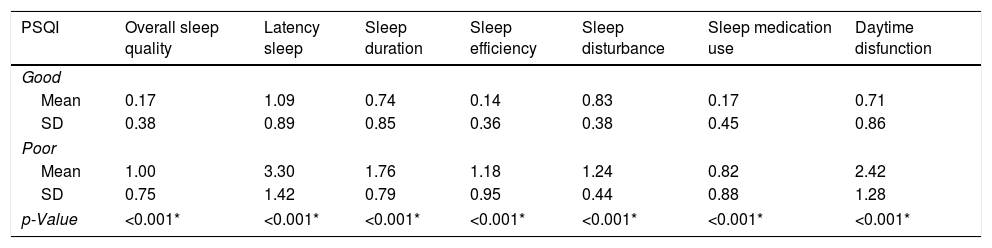
Characteristics of samplesTable 2 shows a group of study subjects with good sleep quality (PSQI<5) and research subjects with poor sleep quality (PSQI>5). PSQI has seven components, namely subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleeping pills, and activity dysfunction. The table below illustrates the differences in each component in PSQI in research subjects with good sleep quality and poor sleep quality.
Characteristic PSQI components.
| PSQI | Overall sleep quality | Latency sleep | Sleep duration | Sleep efficiency | Sleep disturbance | Sleep medication use | Daytime disfunction |
|---|---|---|---|---|---|---|---|
| Good | |||||||
| Mean | 0.17 | 1.09 | 0.74 | 0.14 | 0.83 | 0.17 | 0.71 |
| SD | 0.38 | 0.89 | 0.85 | 0.36 | 0.38 | 0.45 | 0.86 |
| Poor | |||||||
| Mean | 1.00 | 3.30 | 1.76 | 1.18 | 1.24 | 0.82 | 2.42 |
| SD | 0.75 | 1.42 | 0.79 | 0.95 | 0.44 | 0.88 | 1.28 |
| p-Value | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* |
Table 3 shows the relationship between research subjects with PSQI both and Uruk with the degree of insomnia and quality of life. In QOLIE-31, the quality of life of epilepsy patients is assessed in general, then broken down into seven components, namely anxiety generation, quality of life, emotional disturbances, energy or fatigue, cognition, treatment effects, and social functions.
DiscussionSleep disorders are generally not too problematic for healthy people, but considerable influence on patients with chronic diseases, especially in patients with epilepsy, the consequences can be more severe, lack of sleep can cause memory dysfunction, severe drowsiness during the day and directly can contribute to the emergence of seizures. The causes of sleep disorders in epilepsy patients are similar to the average population in general, such as lack of sleep, sleep-hygiene, circadian rhythm disorders (Table 4).
Relationship of the degree of insomnia with QOLIE-31.
| Insomnia | QOLIE 31 | Total | p-Value | |
|---|---|---|---|---|
| Good quality of life | Poor quality of life | |||
| No insomnia | <0.001 | |||
| n | 40 | 0 | 40 | |
| % | 72.7 | 0.0 | 58.8 | |
| Mild insomnia | ||||
| n | 11 | 5 | 16 | |
| % | 20.0 | 38.5 | 23.5 | |
| Moderate insomnia | ||||
| n | 4 | 5 | 9 | |
| % | 7.3 | 38.5 | 13.2 | |
| Severe insomnia | ||||
| n | 0 | 3 | 3 | |
| % | 0.0 | 23.1 | 4.4 | |
| Total | ||||
| n | 55 | 13 | 68 | |
| % | 100.0 | 100.0 | 100.0 | |
* Chi-Square test.
In our results the distribution of male and female research subjects, most were unmarried, and most age distributions were below 35 years, we did not include research subjects with age above 50 years because the sleep quality of elderly patients tended to be worse, according to Sang-Ahm Lee's research, 2015. Most of the educational levels of research subjects were high school, while we did not include subjects with mental retardation. The most extensive distribution of treatment duration is less than ten years, with most types of seizures frequent. The weight of our study subjects was mostly healthy. We did not include research subjects with BMI>30 to avoid bias because obese patients often experience OSA (Table 5).
Sleep quality of the subjects on PSQI has a relatively low cut-off value, where subjects with a questionnaire value >5 out of a total score of 21 are said to have poor sleep quality. There is no further explanation regarding the reduced level of sleep quality difference between patients with PSQI>5. There were no statistically significant differences in the characteristics of the study subjects such as gender, age, level of education, occupation, and length of education, all of which gave a value of p>0.05. Of all these characteristics, only the sex showed the most difference, where sleep quality in male subjects was worse than in women, but it was not statistically significant (p=0.08). Not all patients with poor sleep quality had insomnia, from 33 people with poor sleep quality were five without insomnia, 16 mild insomnia, nine moderate insomnia, and three severe insomnia (Table 6).
Relationship of PSQI and QOLIE-31 components.
| PSQI | QOLIE31 | Seizure worries | Quality of life | Emotional well-being | Energy/Fatigue | Cognitive | Medications effect | Social function |
|---|---|---|---|---|---|---|---|---|
| Good | ||||||||
| Mean | 69.45 | 13.92 | 11.00 | 10.77 | 8.14 | 34.16 | 4.35 | 16.23 |
| SD | 10.41 | 6.56 | 1.68 | 2.01 | 1.51 | 12.51 | 2.02 | 3.46 |
| Poor | ||||||||
| Mean | 40.89 | 12.70 | 9.80 | 8.04 | 5.76 | 30.57 | 4.87 | 12.30 |
| SD | 6.18 | 6.57 | 6.34 | 2.31 | 1.78 | 14.60 | 2.27 | 3.71 |
| p-Value | 0.018** | 0.256** | <0.001** | <0.001* | <0.001* | 0.261** | 0.897** | <0.001* |
Overall there was a significant difference in the quality of life of patients with sleep disorders compared with those without sleep disorders (p=0.018) after a statistical test with Mann–Whitney. This is consistent with a study conducted in Taiwan by Hsui-Fang Chen in 2016 who examined 260 patients epilepsy and sleep disorders are found to be one of the things that affect the quality of life of epilepsy patients. However, if the components of QOLIE-31 are broken down, there is no difference in anxiety (p=0.256) as measured by the independent t-test, at the level of cognition (p=0.261), and the treatment effect (p=0.897 as measured by the Mann t-test Whitney.
ConclusionThere is a difference in the overall quality of life of epilepsy patients with sleep disorders and without sleep disorders, where the quality of life of epilepsy patients with sleep disorders is worst. Besides, there are differences in emotions, fatigue, and social function in epilepsy patients with sleep disorders and epilepsy patients without statistically significant sleep disorders. There are differences in seizure anxiety, cognition, and treatment effects in epilepsy patients with sleep disorders and epilepsy patients without sleep disorders, but not statistically significant.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.