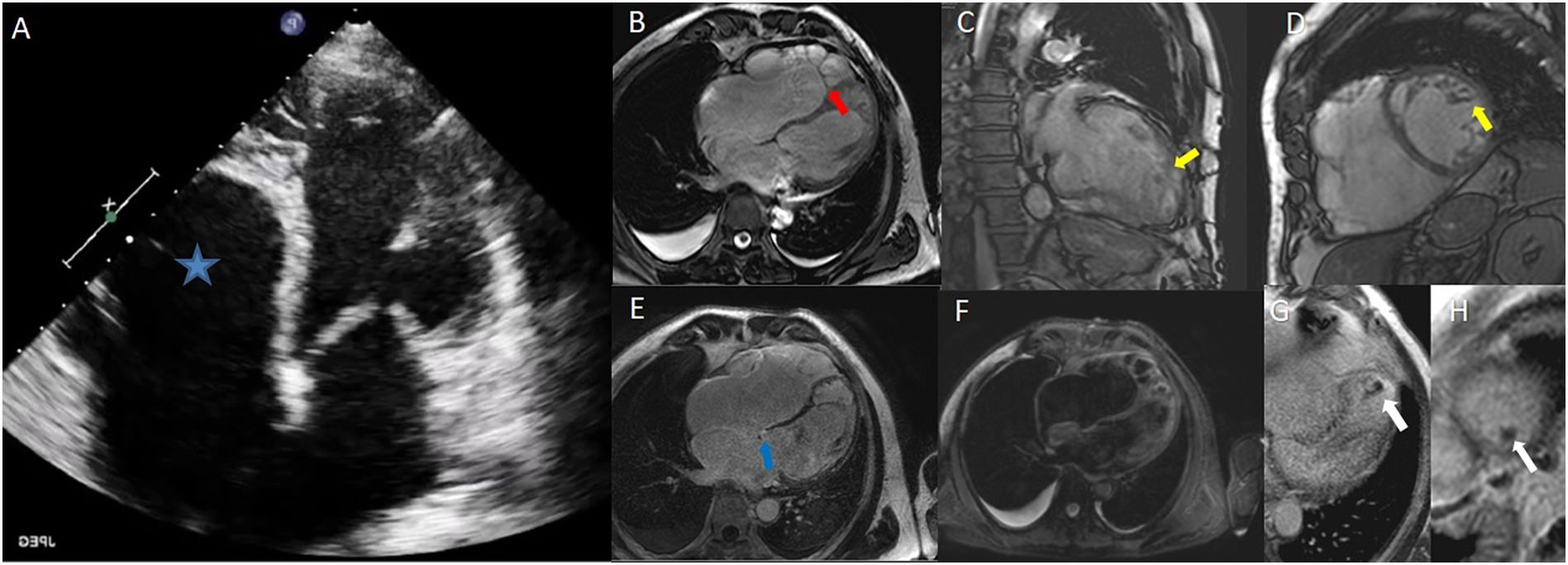
We present the case of a 70-year-old male patient with a history of hypertension, presented with dyspnea on exertion, orthopnea, bendopnea, and palpitations. Chest radiographs showed bilateral pleural effusion and alveolar edema, and blood tests revealed NT-ProBNP of 8022 pg/ml. Electrocardiogram showed atrial fibrillation at 110 beats per minute and bifascicular block (RBBB and left anterior fascicular block). The patient was admitted to cardiology department for acute heart failure. Transthoracic echocardiogram showed a non-dilatated left ventricle with an ejection fraction of 25% and hypertrabeculation (Fig. 1A) at the apical, mid-anterolateral, and mid-inferolateral segments (video 1 of the supplementary data). Furthermore, we observed an increased tricuspid valve-mitral valve offset, with no significant valve dysfunction (video 2 of the supplementary data), causes an atrialization of the right ventricle (asterisk) compatible with Ebstein’s anomaly type B (Carpentier´s classification). We performed and invasive coronariography with no coronary artery disease.
He underwent cardiovascular magnetic resonance imaging (CMR) which confirmed echocardiography conclusions. CMR showed a septal leaflet downward displacement (Fig. 1B, red arrow). Also, findings were keeping with left ventricular non-compaction (LVNC) (Petersen CMR criteria) (Fig. 1C, D, yellow arrow). Left ventricular ejection fraction was 28% with mild late gadolinium enhancement in basal inferior segment (Fig. 1E, blue arrow). STIR sequence did not reveal edema-like signal (Fig. 1F). Besides, we observed a small intraventricular thrombus (8x6 mm) located at the left ventricle apex (Fig. 1 G, H, white arrows).
Genetic testing was also performed for inherited cardiomyopathies (204 genes) with no relevant mutations.
LVNC and Ebstein´s anomaly is a known rare association. Few cases have been reported, some of them associated to pathogenic mutations in genes such as MYH7 and TpM1. CMR is essential in this clinical setting, allows detailed assessment of LVNC and its complications such as thrombus formation.
The following are the supplementary data related to this article.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mcpsp.2022.100349.