Emphysematous pyelonephritis (EP) is a severe necrotizing bacterial pathology caused by gas-forming species that mainly affect the renal parenchyma, collecting system and adjacent perirenal structures.1–3 It is a rapidly progressive infection that can lead to a fatal outcome, which is why it is considered a urological emergency.1,2,4 Death can occur as a result of complications from the infection, such as sepsis, septic shock, acute renal failure, and severe metabolic dysregulation, among others.1,2,5,6
In the past, Type 2 Diabetes Mellitus (DM2) was considered a sine qua none condition in the genesis of EP, but it has also been described in polycystic kidney disease, renal tumors, end-stage renal disease, drug abuse, obstructive uropathy and neurogenic bladder.2–4 EP has been mainly described in women, particularly in those in their sixth decade of life.2–5
By 2020, according to the National Health Survey (ENSANUT) the prevalence of DM2 in Mexico was 15.6% of adults over 20 years of age. The figure in recent years is estimated to be the highest in the continent, at 14.7%.
Regarding renal lithiasis, Ortegon-Gallareta et al. reported that this condition leads to hospitalizations throughout the republic, but with much greater frequency in the state of Yucatan.7 This high frequency may be associated with a combination of factors including high environmental temperatures, water hardness, obesity, high consumption of bottled soft drinks and chronic dehydration, and genetic susceptibility, among others. It has even been proposed that some genetic component in the Mayan-mestizo population may be involved as a probable predisposing factor in the development of lithiasis in Yucatan.7
Based on the above, the aim of this article is to establish the manifestations and outcomes in patients admitted due to emphysematous pyelonephritis from a tertiary level public hospital, and to analyze their outcomes and condition at discharge.
Materials and MethodsThe present submission derives from a study approved by the Board of Research and the Board of ethics at HRAEPY, approval #2020-055. Written Informed Consent was obtained from all patients. Retrospective analytical observational study constituting a clinical series including all cases of hospital discharge due to emphysematous pyelonephritis between January 2016 and December 2019.
The conditions at admission, management, and clinical outcome, as well as the reasons for discharge, were established through a review of files and paraclinical records. For data analysis, descriptive and inferential statistical methods were used, using measures of central tendency such as mean and standard deviation (SD) for variables with normal distribution, and median and interquartile range (IQR) for variables that did not meet this condition. Nonparametric independent Poisson regression analyses reporting risk ratios (1.00 as reference value) were performed. Significance values were set at p<0.05, and post hoc tests were used to ensure the goodness of fit, using Stata14 software.
ResultsThe 60 patients admitted in the urology department and intensive care unit of the HRAEPY met the diagnostic criteria of a CT scan compatible with EP. The median age was 49 years, while 80% of which occurred in the female sex. Half of the patients with EP were suffering some underlying chronic diseases, 48.3% had DM2, 30.0% systolic arterial hypertension (SAS) and 46.6% chronic kidney disease. Regarding the patients with DM2, the mean time since diagnosis was 120 months (24–180) and 13.7% of patients had glycemic imbalance on admission.
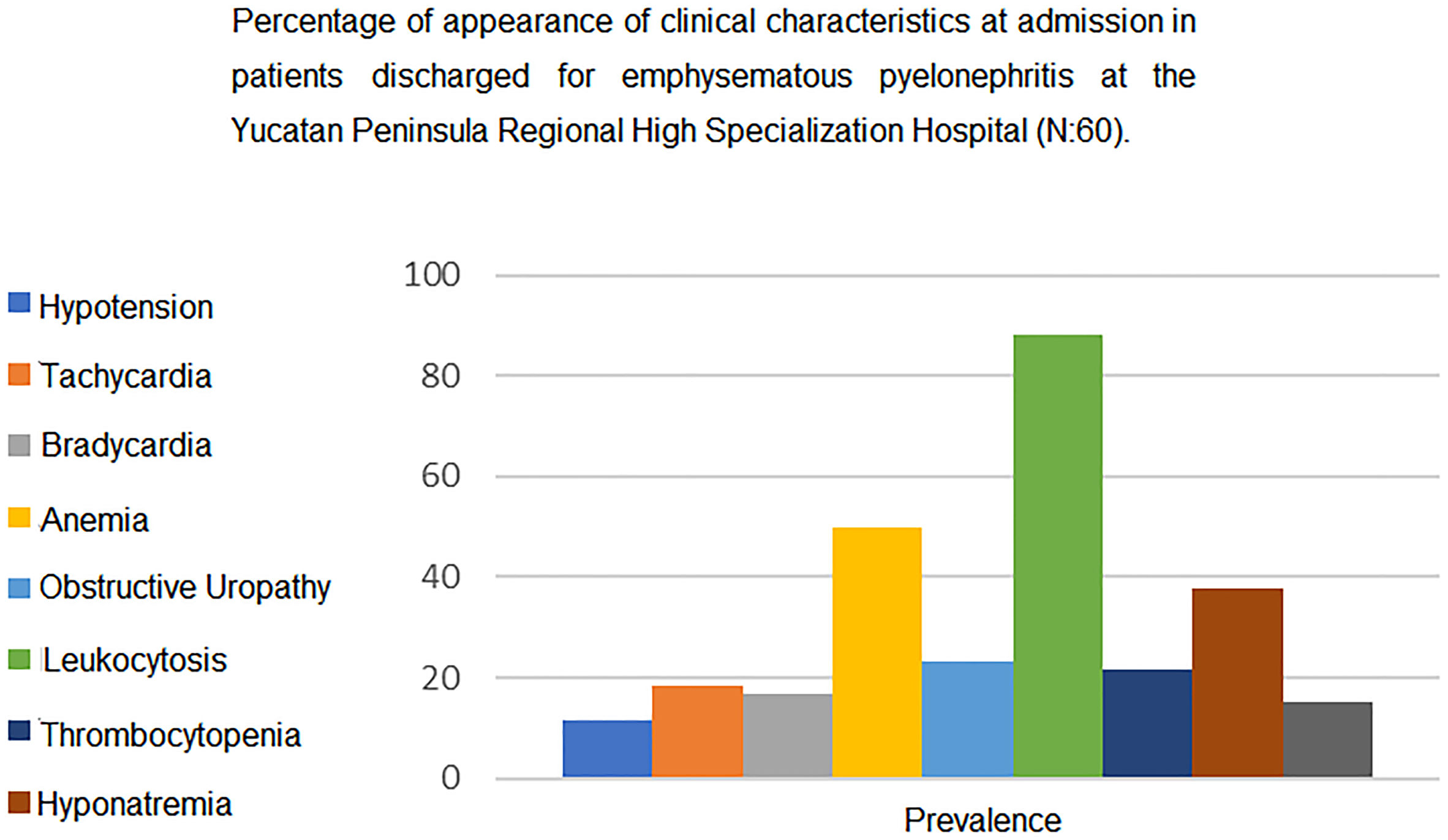
Clinical presentation at admission is shown in Figure 1. Average values included hemoglobin of 9.9 (8.3–11), hematocrit of 31 (26.7–34), leukocytes of 17.9 × 103/mm3 (12.3–22.2), platelets of 347.5 × 103/mm3(220.8), glycemia of 116.5 mg/dL (92.7–192), blood urea of 66.8 mg/dL (34.5–101.3), creatinine of 1.8 mg/dL (1.1–3.3), sodium of 136 mg/dL (132–138), potassium of 4.2 (0.7), chlorine of 105.1 (102–109), and a glomerular filtration rate according to CKD-EPI of 33.6 mL/min/1.73 m2 (16–78.8). In 23.3% of the patients a diagnosis of sepsis of urologic origin was added at some point during their in-hospital stay.
As for the tomographic findings, the most frequent involvement was in the left kidney with 48.3%, followed by right kidney and bilateral involvement with 43.3 and 8.3%, respectively. In 53 out of 60 of the admission CT scans, some type of obstructive uropathy was identified, all of them due to lithiasis, with stone location on the ipsilateral side to the affected kidney. As regards the type of lithiasis, 39.6% were in the ureter and 60.3% in the kidney.
In the urine cultures that were carried out on admission, 37 cases were reported positive, and 1 negative. The microorganisms found in descendent order were: Escherichia coli, Acinetobacter, Klebsiella pneumoniae and polymicrobial flora (including Proteus mirabilis, Enterococcus faecalis, Enterococcus faecium, Enterobacter cloacae, and Candida albicans)
Regarding treatment modalities and outcomes, they are shown in table 1. It is worth mentioning that the initial therapeutic plan included only one patient who was a candidate for nephrectomy from the beginning, and the presence of 13.3% monorenal patients ruled out the possibility of nephrectomy in these cases. The mean and standard deviation of days of hospital stay and days in the intensive care unit were 10.7 and 7.3, respectively.
Treatment modality and outcomes in patients with emphysematous pyelonephritis at the Yucatan Peninsular Regional High Specialization Hospital (N:60).
| Variable | No. | Percentage |
|---|---|---|
| Antibiotic therapy | ||
| Piperacillin/Tazobactam | 15 | 25 |
| Meropenem | 12 | 20 |
| Imipenem | 10 | 16.7 |
| Ceftriaxone | 10 | 16.6 |
| Ertapenem | 8 | 13.3 |
| Others | 3 | 8.4 |
| Definitive treatment | ||
| Antibiotic therapy only | 27 | 45 |
| Nephrectomy | 21 | 35 |
| Double J catheter | 8 | 13.3 |
| Double J catheter plus nephrostomy | 4 | 6.6 |
| Outcome | ||
| Survival | 54 | 90 |
| Mortality | 1 | 1.8 |
| Unreported | 5 | 8.3 |
| Recurrence within 3 months | 13 | 21.6 |
| ICU admission | 6 | 10.7 |
ESBL: extended spectrum B-lactamase; ICU: Intensive care unit.
Regarding the association between admission conditions and exclusive antibiotic therapy management, Poisson's analysis showed that glucose values, number of urinary tract infections and blood pressure values were inversely associated with the probability of exclusive antibiotic management, while the absence of abscess also reduced the probability of this type of management (Table 2).
Poisson analysis of factors related to exclusive antibiotic treatment.
| Variable | Risk Ratio | p | IC 95% | |
|---|---|---|---|---|
| Sex (Female) | 0.78 | 0.437 | −2.33 | 5.39 |
| Age | 0.06 | 0.952 | 0.18 | 0.08 |
| Glucose levels | 0.18 | 0.047 | 8.07 | 0.33 |
| Systemic arterial hypertension | 0.24 | 0.016 | 0.03 | 0.70 |
| Respiratory frequency | 0.40 | 0.688 | 0.32 | 2.12 |
| Cardiac frequency | 0.09 | 0.931 | 0.07 | 0.11 |
| Recent urinary infections | 1.15 | 0.031 | 0.08 | 1.89 |
| Chronic Kidney Disease | 2.11 | 0.035 | 0.31 | 8.48 |
| Hematocrit reading on admission | 1.46 | 0.144 | 0.00 | 0.05 |
| DM2 | 0.30 | 0.760 | 0.08 | 0.59 |
| Renal Lithiasis | 1.03 | 0.304 | 0.45 | 1.42 |
| Average arterial pressure | 0.23 | 0.02 | 0.15 | 0.40 |
| Hemoglobin | 0.28 | 0.782 | 0.18 | 2.40 |
| Platelet count | 1.40 | 0.16 | 0.10 | 0.71 |
| Presence of abscess | 0.24 | 0.01 | 0.13 | 0.33 |
| E. coli ESBL | 1.81 | 0.071 | 0.24 | 5.97 |
ESBL: extended spectrum beta-lactamase carrier.
Significant values with p<0.05 are presented in bold and italic fonts.
In the association model which takes length of hospital stay as the dependent variable, it was determined by Poisson regression (Table 3) that a higher respiratory rate, an absence of chronic kidney disease, lower hematocrit and platelet counts, and the presence of abscess on admission, were all associated with a longer hospital stay.
Poisson analysis of factors related to days of hospital stay.
| Variable | Risk Ratio | P>z | IC 95% | |
|---|---|---|---|---|
| Female sex | 0.61 | 0.542 | 0.57 | 1.29 |
| Age | 1.55 | 0.120 | 0.99 | 1.01 |
| Glucose levels | 4.10 | 0.000 | 1.00 | 6.00 |
| Arterial hypertension | 1.56 | 0.118 | 0.96 | 1.34 |
| Respiratory frequency | 6.70 | 0.000 | 5.08 | 7.15 |
| Cardiac frequency | 5.80 | 0.000 | 3.80 | 7.01 |
| Recent infection | 1.15 | 0.251 | 0.92 | 1.33 |
| Chronic Kidney Disease | 0.83 | 0.409 | 0.80 | 1.09 |
| Hematocrit | 2.49 | 0.013 | 1.98 | 3.99 |
| DM2 | 1.40 | 0.162 | 0.95 | 1.30 |
| Lithiasis | 1.67 | 0.095 | 0.66 | 1.03 |
| Average Arterial Pressure | 1.26 | 0.209 | 0.98 | 1.00 |
| Hemoglobin | 1.24 | 0.215 | 0.94 | 1.01 |
| Platelet count | 0.23 | 0.022 | 0.11 | 0.59 |
| Abscess | 5.93 | 0.000 | 1.36 | 8.86 |
| E. coli ESBL | 0.09 | 0.928 | -0.83 | 1.17 |
ESBL: extended spectrum beta-lactamase carrier.
A total of 60 cases attended in the urology department and intensive care unit (ICU) of the HRAEPY over a period of 4 years were recorded. Regarding regards comorbidities, urolithiasis was the main associated condition, and even when DM2 has been associated in several series as the predisposing factor with the greatest implication in the development of EP, in a percentage that ranges from 66%-95%.4,8,9, in this study only 48.3% patients presented this condition. In relation to the main predisposing factor, a prospective observational study was carried out including 53 patients, where the presence of lithiasis was found to be the second emphysematous pyelonephritis predisposing factor in 24.5% of patients, after diabetes mellitus with 67.9. 6 This is consistent with a retrospective study conducted in India where out of 74 patients, 85.15% and 32.43% had diabetes mellitus and urolithiasis, respectively.8 These results differ with our study where the majority of the patients’ presented urolithiasis as the main predisposing factor.
As for the sociodemographic results, the average age (49.9 years) coincided with Olvera-Posada et al., (2014) but differed from the age reported by other research outside Mexico (55-60 years).1,4,9,11 Although high blood glucose availability has been described as a predisposing factor for growth, gas production, and fermentation in the bacteria causing EP, only 13.7% of cases reported figures compatible with the criteria for glycemic imbalance on admission, which reinforces our conclusions that glucose and DM are not the most implicated factors in cases of EP in southeast Mexico.7 The presence of abscess was related to a higher risk of requiring a nephrectomy and more days of hospital stay, while its absence was related to a higher probability of requiring only isolated medical management and fewer days of hospital stay, in agreement with the reports of other authors.10–11
The most frequently isolated microorganism was E. coli (53.6%), which coincides with the reports of several series carried out in this country, and with the systematic review published by Aboumarzouk et al.4,9,11 However, it is worth mentioning that the proportion of E. coli in comparison with other agents was much lower than that reported in the sources consulted.
Nephrectomy was part of the original treatment plan in only one case at the time of hospital admission, which is congruent with the recommendations to opt for this procedure only in severe cases and when there are factors suggesting a poor prognosis.1,10 However, in total there were 21 patients in whom clinical deterioration and paraclinical evidence led to the clinical decision to perform a nephrectomy. The in-hospital mortality rate of 1.8% coincides with other recent studies5 but differs from clinical series in contexts in which nephrectomy was the most viable alternative.1,4,11 As regards recurrence, 13 cases (21.6%) were reported in a period of 3 months after discharge, which coincides with studies from other countries5, while the survival rate of 90% was like that reported in the series of Adapala et al.3.
In both Poisson regressions, higher respiratory and heart rate figures, and lower hematocrit and platelet count were found, which could condition a longer hospital stay. A longer stay also coincided with the tendency to tachypnea and tachycardia, which are clinical criteria for sepsis according to the qSOFA scale.2,11
Among the limitations of this study are those inherent to its retrospective design and the fact that it refers to a single center, which is in a region with a peculiarly high prevalence of both diabetes and urolithiasis; therefore, caution is required when extrapolating these findings to populations with different epidemiological characteristics.
ConclusionsIn the clinical series from the Yucatan Peninsula Regional High Specialization Hospital, the concomitant pathology in 60 patients discharged for emphysematous pyelonephritis was obstructive uropathy in 83% of cases, while DM2 was present in 43% of the patients. Treatment was guided by conditions at admission, as well as the outcomes during the hospital stay, such that in 45% of cases the condition were resolved with exclusive antibiotic therapy. In-hospital mortality was 1.6%. Monitoring from admission and paying attention to both clinical conditions and paraclinical parameters, can translate in taking timely measures in a planned manner, improving the prognosis of the patients and possibly, prevent recurrences. This study shows that the prevalence of urolithiasis in the population under study was even more frequent than DM2, which adds to the multiple reasons for establishing preventive measures for urolithiasis, particularly in vulnerable populations.
Declaration of interestsThe authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Does not apply