Olfactory carcinoma is a recently described malignancy that poses significant diagnostic challenges. Accurate histopathological analysis is essential to distinguish it from other sinonasal tumors with neuroendocrine differentiation.
Case reportWe present the case of a patient who reported a three-month history of left-sided nasal obstruction, hyposmia, and epistaxis. Nasal endoscopy and imaging (CT and MRI) revealed a polypoid, angiomatous mass originating from the left olfactory recess. Staging studies showed no evidence of metastasis or secondary lesions. The patient underwent surgical resection with clear microscopic margins. After one year of follow-up, there were no signs of recurrence or residual disease.
DiscussionDue to its recent classification, the natural history and optimal treatment approach for olfactory carcinoma remain unclear. Management decisions should be made by multidisciplinary head and neck oncology teams. Current treatment strategies are modeled after those used for similar tumors, such as olfactory neuroblastoma and small- or large-cell neuroendocrine carcinomas. Combined treatment with surgery and adjuvant radiotherapy appears more effective than monotherapy.
ConclusionTherapeutic consensus is urgently needed for this newly recognized malignancy to guide effective clinical decision-making and improve patient outcomes.
El carcinoma olfatorio es una neoplasia recientemente descrita que plantea importantes desafíos diagnósticos. Un análisis histopatológico preciso es esencial para diferenciarlo de otros tumores nasosinusales con diferenciación neuroendocrina.
Caso clínicoPresentamos el caso de un paciente con historia de tres meses de obstrucción nasal izquierda, hiposmia y epistaxis. La endoscopia nasal y las imágenes (TC y RM) revelaron una masa polipoide y angiomatosa originada en el receso olfatorio izquierdo. Los estudios de estadificación no mostraron evidencia de metástasis ni de lesiones secundarias. El paciente fue sometido a una resección quirúrgica con márgenes microscópicamente libres. Tras un año de seguimiento, no se observaron signos de recurrencia ni enfermedad residual.
DiscusiónDebido a su reciente clasificación, la historia natural y el enfoque terapéutico óptimo para el carcinoma olfatorio aún no están claramente definidos. Las decisiones terapéuticas deben ser tomadas por equipos multidisciplinarios de oncología de cabeza y cuello. Las estrategias actuales de tratamiento se basan en las utilizadas para tumores similares, como el neuroblastoma olfatorio y los carcinomas neuroendocrinos de células pequeñas o grandes. El tratamiento combinado con cirugía y radioterapia adyuvante parece ser más eficaz que la monoterapia.
ConclusiónEs necesario alcanzar un consenso terapéutico para esta neoplasia recientemente reconocida, a fin de orientar una toma de decisiones clínicas efectiva y mejorar los resultados en los pacientes.
Sinonasal malignancies with neuroendocrine differentiation are rare, with an estimated incidence of eight cases per million.1 Within this type of tumors, three distinct entities are classically identified: olfactory neuroblastoma (ONB), small-cell neuroendocrine carcinoma, and large-cell neuroendocrine carcinoma (NEC). However, an additional entity known as olfactory carcinoma (OC) has been recently described. It is characterized by the presence of both neuroendocrine differentiation (seen in ONB) and epithelial elements such as glandular formation or cytokeratin positivity (present in NEC).2 To date, only a few cases have been reported and there is no clear consensus in terms of considering OC as a new entity or an atypical histological variation of previously known sinonasal malignancies with neuroendocrine differentiation. We report a case diagnosed and treated in our center to contribute to a better understanding of this entity.
Case presentationA man in their fifties presented with a three-month history of left nasal airway obstruction, hyposmia, and left-sided epistaxis. He smoked twenty cigarettes per day and had no relevant history of exposure to volatile compounds. Nasal endoscopy (Fig. 1A) and imaging (computed tomography (CT) and magnetic resonance (MR) revealed the presence of a polypoid-angiomatous mass originating from the ipsilateral olfactory recess. It displaced the medial orbital wall laterally, but it was not infiltrated (Fig. 1B–E). Extension studies, including positron emission tomography and computed tomography (PET-CT), did not show the presence of metastasis or secondary lesions.
A. Intraoperative endoscopic view of the left nasal cavity. The OC has a polypoid-angiomatous appearance and originates from the ipsilateral olfactory recess. Fig. 1B–E. Preoperative sinonasal imaging: CT (1C. Axial view; 1D. Coronal view) and T2-weighted MR (1B. and 1E. Coronal view). Large left nasal neoplasm (5 x 1.7 x 4.8 cm) that affects the left nasal cavity, involving all three ipsilateral turbinates, extending to the left nasopharynx, sphenoid sinus, ethmoid air cells, and ipsilateral maxillary sinus, showing extensive contact with the nasal septum, lamina papyracea, and cribriform plate. It occludes the left sphenoethmoidal and frontal recesses, causing mucosal retention, protruding into the sphenoid sinus, bulging, and deforming the inner wall of the left orbit, with secondary displacement of the left medial rectus muscle without apparent intracranial or ipsilateral orbital tumor infiltration, causing erosion in the walls of the described structures.
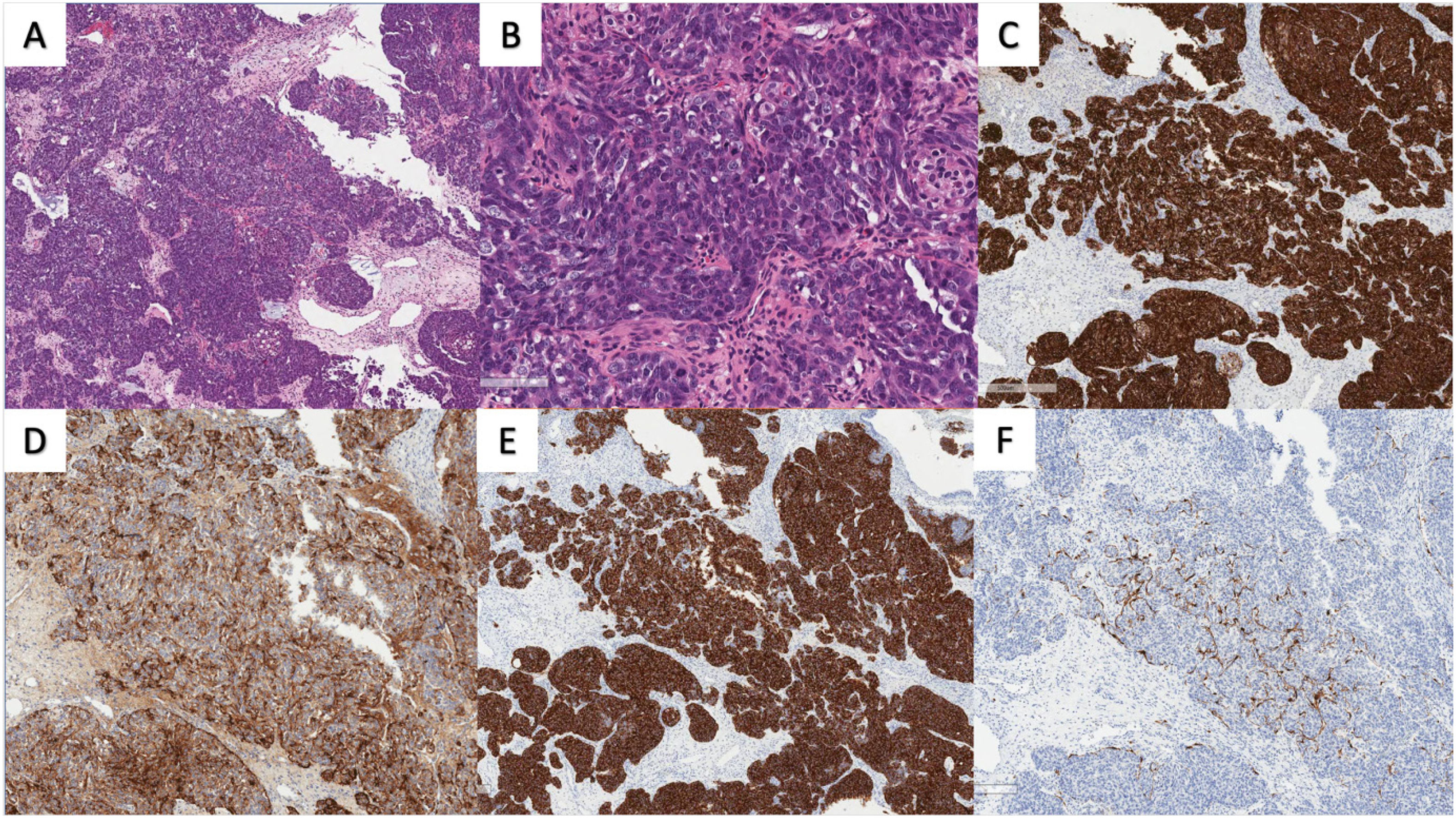
Biopsies were obtained at the outpatient clinic under local anesthesia. Histopathology and immunohistochemistry reports described a high-grade malignancy with mixed features of ONB and NEC (Fig. 2). An atypical cellular proliferation consisting of nodules, confluent nests, and rosettes was observed. In addition, cells presented large basophilic nuclei, granular salt-and-pepper chromatin, and visible nucleoli with moderate nuclear pleomorphism and cytoplasm. The sample showed a high proliferation index (Ki67 20%), but no signs of necrosis. Immunohistochemistry showed positivity for chromogranin, synaptophysin, CKAE1/AE3, and CD117. Also, S100 was positive in sustentacular cells. These findings suggested a common progenitor stem cell origin, most likely at an olfactory basal cell.
Anatomophatological images of olfactory carcinoma exhibiting atypical cellular proliferation forming lobules, trabeculae, and rosettes (A). The tumor cells were high-grade, with large nuclei, salt-and-pepper chromatin, and prominent nucleoli (B), demonstrating moderate pleomorphism and eosinophilic cytoplasm. Glandular cells showed strong positivity for cytokeratin (C), while neuroectodermal cells displayed variable expression of neuroendocrine markers such as chromogranin (D) and synaptophysin (E). Sustentacular cells exhibited positivity for S100 protein (F).
Management was discussed with the local head & neck cancer multidisciplinary team, and it consisted of surgery (transnasal endoscopic approach) and adjuvant radiotherapy. Surgery was successful and resulted in free microscopic margins (R0). The resection resulted in a mild cerebrospinal fluid leak due to a small dehiscence at the ipsilateral lateral lamella (overlying the olfactory mucosa). The defect was repaired in a single-layer fashion during the procedure, using a free mucosal flap from the middle turbinate and a fibrin sealant. The postoperative period went uneventful, but the patient refused the adjuvant radiotherapy. One year after surgery, the patient is asymptomatic, and close follow-up (including head & neck examination and MR) showed no signs of recurrence or residual disease.
DiscussionThe incidence of OC is unknown; to date, only a few cases have been reported and a precise histopathological study is essential to differentiate this entity from ONB and NEC.3 In our patient, the tumor presented a nested structure, lobules and Homer Wright pseudorosettes like ONB, combined with areas that showed epithelial differentiation conforming glands similar to NEC. However, immunohistochemistry was decisive to achieve the diagnosis, due to the positivity for neuroendocrine markers (chromogranin, synaptophysin and S100 in sustentacular cells) and cytokeratin markers (CKAE1/AE).4,5
Therapy should be discussed with the local head & neck cancer multidisciplinary teams. It is based on that of malignancies with similar histopathology features and location, such as ONB and NEC. For ONB, surgery (transnasal endoscopic approach, if possible) followed by adjuvant radiotherapy showed 5-year survival rates of 80 and 40%, for low- and high-grade tumors, respectively. Recurrence is observed in 30% of the cases, and it may have a late onset (up to 5 years after therapy).6 On the other hand, NEC is very rare and there is no clear consensus on the most appropriate treatment strategy, but surgery with adjuvant radiotherapy appears more beneficial than a single-modality treatment.7 Further reports on histopathology, natural history, recurrence, and survival rates are key to establishing the most appropriate management for OC. We share the histopathology features of our case, which support the presence of differential features compared to other sinonasal malignancies with neuroendocrine differentiation. In our case, R0 resection was achieved but the patient refused adjuvant radiotherapy. The analysis of the recurrence and survival rates after being treated with single-modality treatment (surgery) will help in understanding the behavior of this entity. To date, the are no signs of recurrence and the patient is under close follow-up (head & neck examination and MR). Late recurrence rates observed in ONB should keep clinicians aware of the importance of close follow-up.
List of abbreviationsConsent for publicationOral and written consent was obtained to publish the images.
Ethics approval and consent to participateProcedures followed here were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 1983. We have not used patients' names, initials or hospital numbers.
FundingNo specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Availability of data and materialThe datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions- -
ITT performed the writing of the manuscript.
- -
MSB performed the revision of the paper.
- -
MAC performed the surgery and supervised the work.
- -
SA contributed to the initial development of this paper.
The authors have declared no conflicts of interest.
Not applicable