Technology Enhanced Medical Education International Conference (THEME 2019)
Más datosInvagination is a type of strangulation in which blood vessels in the mesentery of proximal intestine enter the distal intestine (intussusception) trapped between the two intestinal walls to allow necrosis. The purpose of this study was to determine the distribution of invagination cases based on demographic characteristics, clinical manifestations, type of invagination, management, and outcomes.
MethodsThis study was a retrospective study conducted at our institution based on the medical Records section by collecting data on invagination patient within 2013–2017.
ResultsThere are 37 cases were obtained, 33 cases of which performed surgery. The average incidence is 6.6 cases per year. The distribution of invagination cases by age group was highest in the age range of 0–6 months by 11 cases (33.3%). Based on sex, most of the males with 24 cases (72.7%), the most predisposing factor is diarrhea with 18 cases (54.5%). Based on the chief complaint, the most complaint is the red currant jelly stool which was 17 cases (45.4%), the duration of the incident until the patient gets treat, the most at 3 days with 9 cases (27.2%). Based on the type of invagination the most was ileocolic, which was 15 cases (45.4%), the most type of treatment was anastomose resection, which was 21 cases (63.6%). And based on the surgery results of 33 invaginated patients, the most were 27 cases (81.8%) patients alive (cured).
ConclusionInvagination is predominant in male, with the most predisposing factor is diarrhea, and the main complaint is the presence of red currant jelly stool. There were excellent or good surgical outcomes in 27 patients.
Invagination is an acute abdominal condition in children that must be immediately treated because it is a potentially dangerous, not only obstruction but also includes a type of strangulation in which blood vessels in the mesentery of proximal intestine enter the distal intestine (intussusception) trapped between the two intestinal walls to allow intussusception necrosis.1,2
In strangulation cases, a delay of surgery for 1 hour will increase morbidity by 50%, so after invagination diagnosis is established, it must get immediate treatment. Patients usually die from toxic conditions and endotoxin shock.3–5
Pain is the most typical symptom and is almost always present. With the onset of pain/colic that increases and reaches its peak, and then disappears altogether, the diagnosis can almost be made. Pain is related to passage from intussusception. Between attacks with subsequent attacks, the baby or adult can be completely symptom free.6–8
It is very important to know when the patient first shows signs of colic, because this is related to the prognosis, strangulation, delay of surgery for 1 hour will increase morbidity by 50%, so in cases of invagination after diagnosis is established, immediate treatment must be given. Usually sufferers die from toxic conditions and endotoxin shock.3–5,9
The purpose of this study was to determine the distribution of invagination cases based on demographic characteristics, clinical manifestations, type of invagination, management, and outcomes.
MethodsThis study was a retrospective study conducted at main referral hospital in the Makassar, Indonesia by collecting medical records data on invagination patient within 2013–2017. Inclusion criteria: invagination patients who were treated at our institution and were willing to join the study. Exclusion Criteria: patients who have incomplete data on medical records. From the data obtained, recorded gender, age, chief complaint, predisposing factors, duration of complaints to get treat, type of invagination, type and results of surgery. The data that has been collected then processed, analyzed, and presented in tabular and narrative form.
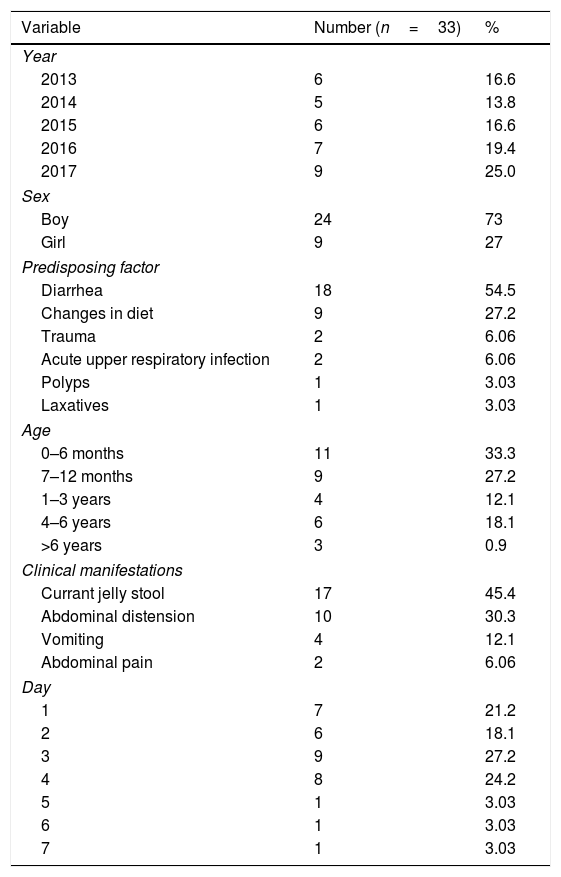
ResultsThe obtained data during the period of 2013–2017 in our institution shows 37 cases of invagination patient, 33 cases of which were operated on. There cases are fluctuations from year to year. The most cases in 2017 with 9 cases (25.0%) and the lowest cases in 2014 were 5 cases (13.8%) (Table 1).
Patient characteristics.
| Variable | Number (n=33) | % |
|---|---|---|
| Year | ||
| 2013 | 6 | 16.6 |
| 2014 | 5 | 13.8 |
| 2015 | 6 | 16.6 |
| 2016 | 7 | 19.4 |
| 2017 | 9 | 25.0 |
| Sex | ||
| Boy | 24 | 73 |
| Girl | 9 | 27 |
| Predisposing factor | ||
| Diarrhea | 18 | 54.5 |
| Changes in diet | 9 | 27.2 |
| Trauma | 2 | 6.06 |
| Acute upper respiratory infection | 2 | 6.06 |
| Polyps | 1 | 3.03 |
| Laxatives | 1 | 3.03 |
| Age | ||
| 0–6 months | 11 | 33.3 |
| 7–12 months | 9 | 27.2 |
| 1–3 years | 4 | 12.1 |
| 4–6 years | 6 | 18.1 |
| >6 years | 3 | 0.9 |
| Clinical manifestations | ||
| Currant jelly stool | 17 | 45.4 |
| Abdominal distension | 10 | 30.3 |
| Vomiting | 4 | 12.1 |
| Abdominal pain | 2 | 6.06 |
| Day | ||
| 1 | 7 | 21.2 |
| 2 | 6 | 18.1 |
| 3 | 9 | 27.2 |
| 4 | 8 | 24.2 |
| 5 | 1 | 3.03 |
| 6 | 1 | 3.03 |
| 7 | 1 | 3.03 |
Distribution of patients by sex is boy as many as 24 patients (73) while girl were 9 patients (27%), with a ratio of boy:girl=8:3. Distribution most cases of invagination by age group in the age range of 0–6 months were 11 cases (33.3%), followed by age groups 7–12 months by 9 cases (27.2%), in the age group between 1 and 3 years as many as 4 cases (12.1%), age group 4-6 years as many as 6 cases (18.1%), and lowest age group >6 years as many as 3 cases (0.9%). The oldest age is found in women with age 11 years and the youngest is men with age 3 month. The most predisposing factors for invagination were diarrhea of 18 patients (54.5%), changes in diet of 9 patients (27.2%), trauma 2 patients (6.06%), Acute upper respiratory infection 2 patients (6.06) %), Polyps 1 patient (3.03%) and laxative administration 4 patients (3.03%) (Table 1).
Chief complaints of patients when they first came to the hospital were the Currant Jelly Stool for 17 patients (45.4%), abdominal distension for 10 patients (30.3%), vomiting for 4 people (12.1%) and abdominal pain 2 patients (6.06%).
The history of the disease to being taken to the hospital is as follows: 1 day for 7 patients (21.2%), 2 days for 6 patients (18.1%), 3 days for 9 patients (27.2%), 4 days were 8 patients (24.2%), 5 days were 1 patient (3.03%), 6 days were 1 patient (3.03%) and 7 days were 1 patient (3.03%) (Table 1).
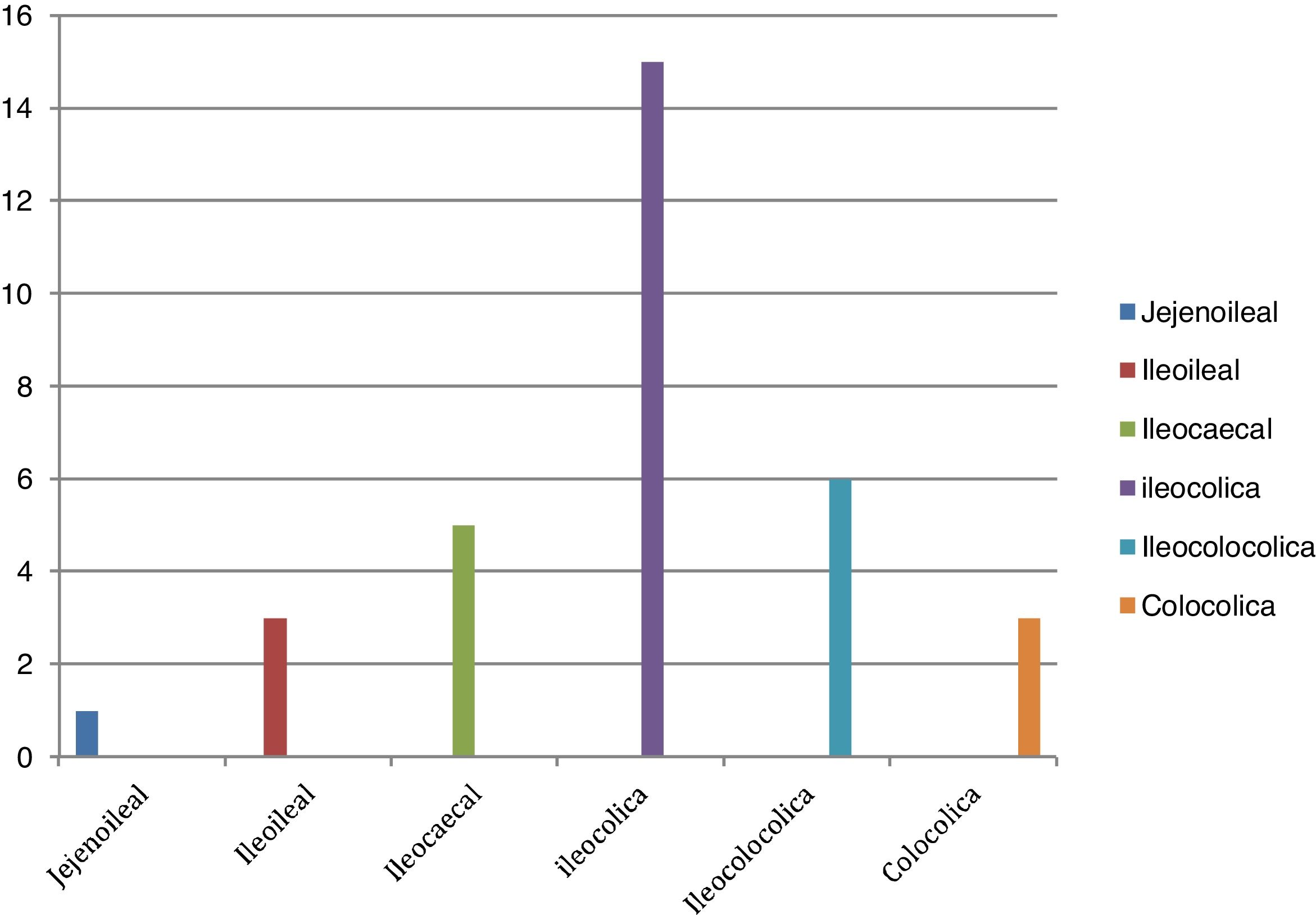
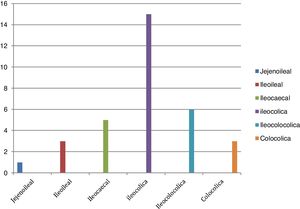
Fig. 1 shows that 70 patients undergoing exploratory laparotomy surgery found the most invagination types were Ileocolic type 15 cases (45.4%), then Ileocolocolica 6 cases (18.1%). Ileocecal in 5 cases (15.1%), and the least were colocolica in 3 cases (9.09%), ileoileal in 3 cases (9.09%) and jejunoileal in 1 case (3.03%).
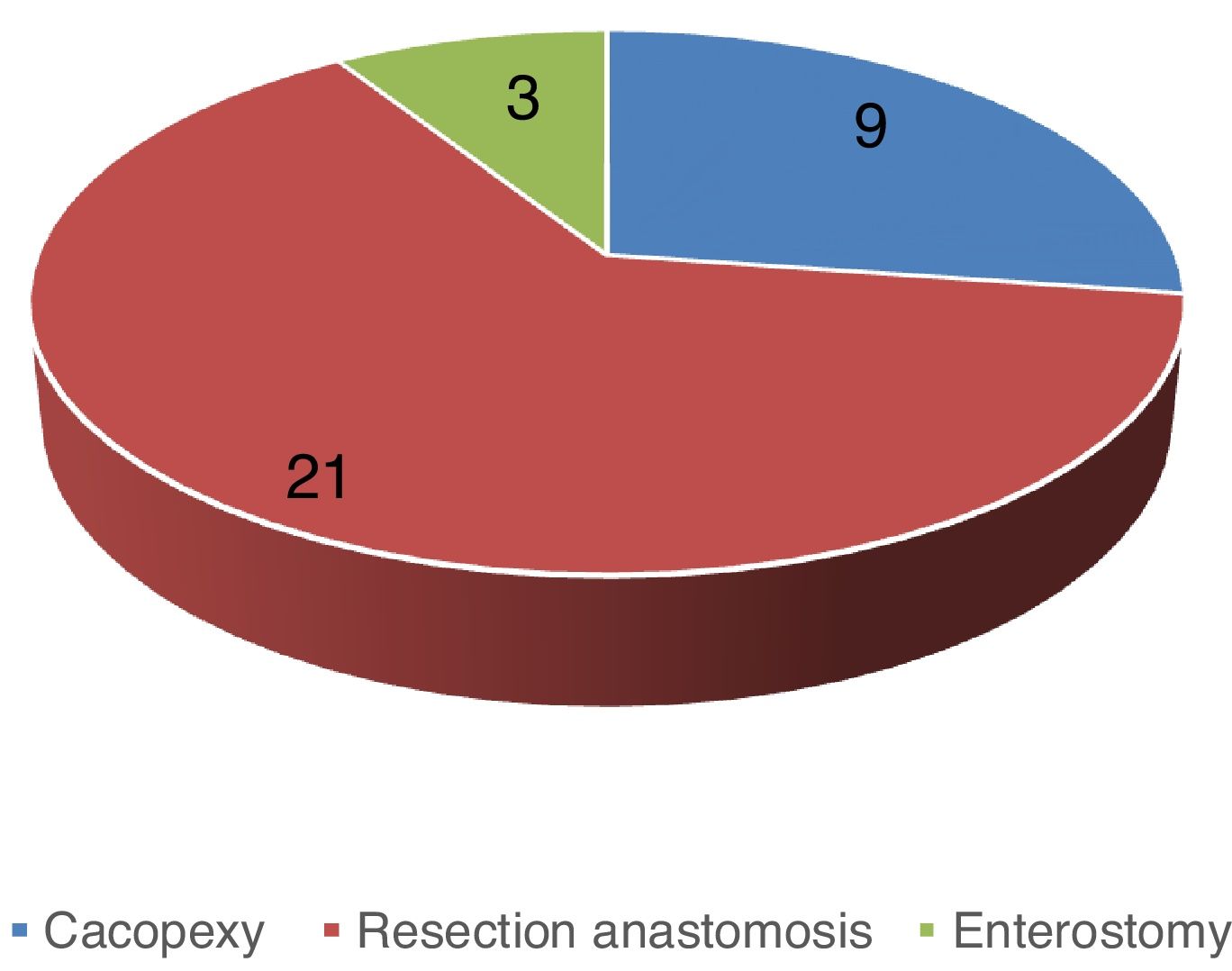
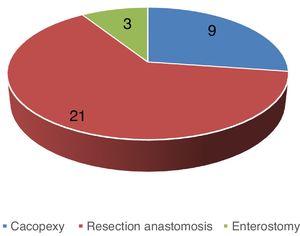
Fig. 2 shows that 3 types of surgery treatment on invagination case management found cecopexy performed in 9 patients (27.2%), resection of anastomose in 21 patients (63.6%) and enterostomy in 3 patients (9.09%).
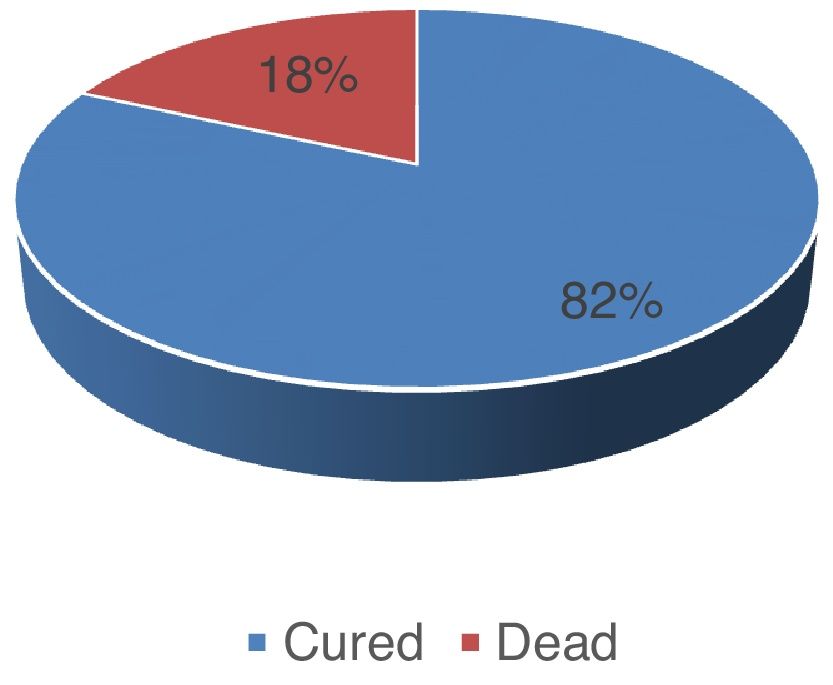
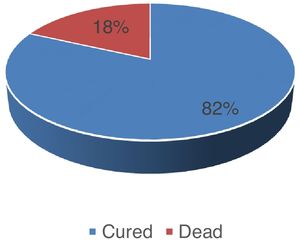
Fig. 3 shows the surgery results of 33 invaginated patients who underwent surgery, 27 (81.8%) patients were alive (cured) and 6 (18.1%) of them died.
DiscussionDuring the period within 2013–2017, 33 invagination cases were found. From year to year the number fluctuates with an average of 17.2 cases per year in children. The incidence is relatively low compared to other pediatric surgery cases. In America, the incidence of invagination occurs in infants 22 cases per 100,000 infants.10 From the available data, boy gender groups suffer more cases of invagination than girl. According to the literature that there are more boy than girl by a ratio of 3:2,5,11,12 and according to other literature 3:1.13 The majority of patients with invagination are healthy babies, boy are more frequent than girl with a ratio of 2:1.14,15 In this study 6.1:3.8 was obtained. In children older than 4 years, the incidence ratio of boys to girls is 8:1.16,17
From the distribution of cases by age group, it was found that the most cases were at 0–6 months and 7–12 months, this result is in line with the literature where most cases at 6–9 months,16–18 3–12 months. From the case report, invagination occurs at the age of the first 2 years (95% of cases).18,19
Based on the distribution of cases according to the invagination predisposing factors most cases cause by diarrhea followed by changes in the type of food, respiratory infections, and trauma this is in accordance with the literature that predisposing factors usually because of diarrhea and changes in the type of food from a liquid diet towards semi-solids and solid food.20 Most cases of invagination with predisposing factors to diarrhea due to viruses cause hyperperistaltic and hypertrophic lymph node follicles in terminal ileum which are the triggering factors for invagination.8,21,22 Also, a previous history of Acute Upper Respiratory Infection will cause an increase in peristalsis coupled with stimulation from changes in feeding types from liquid to semi-solid and solid.1,23 In the literature it is said that the provision of food other than milk when the age is less than 4 months will adversely affect the baby, because the baby's digestive system at this age is not fully developed yet.1 Feeding at that age has the potential for invagination of the small intestine. Whereas at the age of more than 4 years it is usually due to mechanical factors such as polyps and trauma, this was also found in this study.
Based on the chief complaint when the patient comes to get treat, from the literature it is said that most came with complaints of vomiting 85%, 83% abdominal pain, 53% red currant jelly stool and a mass in abdominal palpation Author links open overlay panel.24 In this study, most cases present with the chief complaint of red currant jelly stool and abdominal distension. While overall clinical symptoms, red currant jelly stool was present in 92.3% of cases, and abdominal distension was in 92.3% of cases. In this study, in general all cases contained triad invagination symptoms. Based on the onset of complaints until the patient comes down to get treat, generally arrive late (>1×24h). Rarely come<24h. This might be due to ignorance from the patient's parents and the delay in the previous diagnosis. In the literature it is said that the slower the patient is brought to get treat from the moment of onset of colic signs, meaning the prognosis is getting worse. The emergence of paroxysmal pain in children and toddlers should be suspected of invagination. This symptom is usually followed by the discovery of blood and mucus in the rectum which occurs within 12–24h later which progressively develops and becomes harder.23
From the distribution of cases by invagination type, the most cases of invagination were ileocolic (38.6%) then ileocolocolica (25.7%). This is consistent with the literature that 80–90% of ileocolic cases and 15% ileoileal.25 Generally, the authors agree that most often intussusception regarding ileocecal valvula. However, the incidence ratio for each type of intussusception is still not clear. Perrin and Linsay gave the description: 39% ileocecal, 31.5% ileocolic, 6.7% enteric, 4.7% colicemic, and the rest are rare and non-typical forms.26 In general, anastomose resection was performed, this surgery done because the patient arrives late when there is already intestinal necrosis in the intussusception. Some of them have been successfully done manually by milking and cecopexy done and some are doing enterotomy. The outcome/prognosis of surgery depends on the onset of complaint until it comes to get treat. Invagination with therapy as early as possible has better prognosis.
ConclusionInvagination is predominant in male, with the most predisposing factor is diarrhea, and the main complaint is the presence of red currant jelly stool. There were excellent or good surgical outcomes in 27 patients.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Technology Enhanced Medical Education International Conference (THEME 2019). Full-text and the content of it is under responsibility of authors of the article.