The following case illustrates the poor prognosis of invasive infection by Aspergillus spp. among HIV-infected individuals, despite the use of specific treatment. Early diagnosis and aggressive specific treatment are needed to avoid fatal progression of the disease.
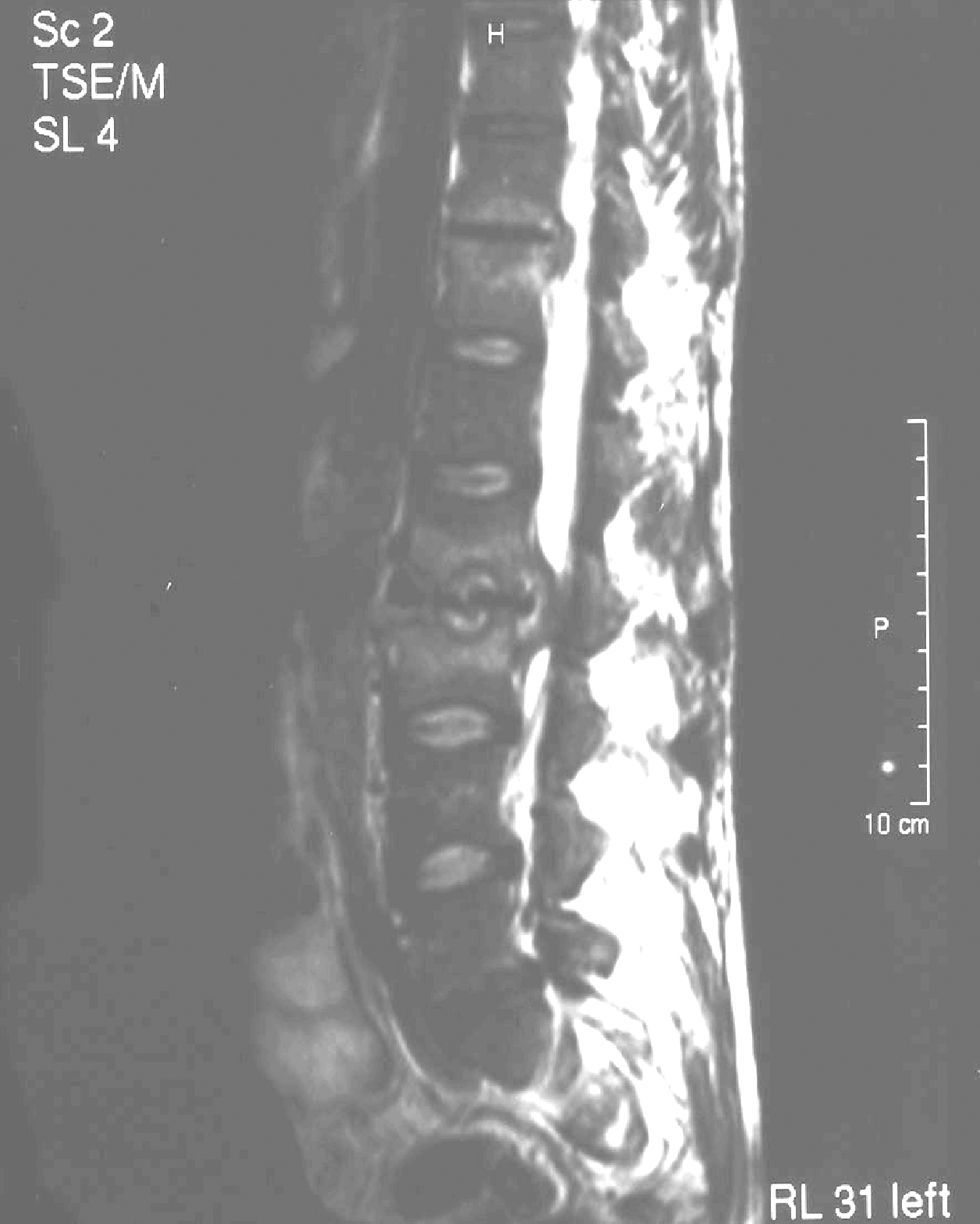
Case reportIn December 2001, a 35-year-old man was admitted for diplopia and inflammatory lumbar pain which had been lasting for one week, without fever or other symptoms. He had formerly been an intravenous-drug user, and HIV infection had been diagnosed in November 1993. He had had disseminated tuberculosis, toxoplasmic encephalitis, and pneumonia due to Nocardia sp. Despite combined antiretroviral therapy (cART) over the last 5 years, his CD4+ T-lymphocyte count remained below 100/μL. At admission, CD4 count was 20/μL and HIV RNA was 174,178copies/mL. Physical examination at admission did not disclose any findings of interest, other than a positive Lasségue sign, and diplopia. Routine laboratory results were normal except for lymphopenia (846/μL). The chest X-ray showed a large cavity with a fluid-air level in the left inferior lobe. X-ray of the lumbar spine demonstrated a lesion at the L2–L3 disc, suggestive of spondylitis. MRI confirmed this finding and revealed another lesion at D11–D12 (fig. 1). Orbit CT scan showed occupation of the maxillary and ethmoidal sinus and the floor of the right orbit (fig. 2). Aspergillus fumigatus grew in a specimen obtained by fine needle aspiration of the L2–L3 intervertebral space, as well as on biopsy of the orbit. Treatment with liposomal amphotericin B (Ambisome®) 300mg/24h was started, but it was withdrawn 15 days later because of impaired renal function (serum creatinine 3.5mg/dL). Itraconazole was then administered (200mg tid). Nevertheless, diplopia did not improve, and neuropathic pain developed in both lower limbs. Dexamethasone (16mg/d) was added. Lumbar CT showed a new epidural abscess at L2–L3. Debridement of the abscess was performed, resulting in a reduction in lumbar pain. Cultures obtained during the procedure yielded A. fumigatus. Fifty days after admission, the patient presented hemoptysis secondary to bronchopulmonary fistulas, which were embolized. CT of the lung showed irregular bullae, one of them with an internal hyperdense image. However, bronchoalveolar lavage culture did not yield A. fumigatus. Some days later, the patient presented respiratory failure in the setting of a septic syndrome caused by Salmonella enteritidis, and died. Autopsy was not authorized.
DiscussionThe incidence of invasive aspergillosis (IA) has risen in recent decades in line with the increase in the population at risk.1 Patients with hematological malignancies, and bone marrow and solid organ transplant recipients are commonly affected. A low CD4 count due to HIV infection is also a risk factor for IA, but this scenario has probably become less frequent since the introduction of cART.2 However, the use of cytotoxic chemotherapy and corticosteroids to treat other opportunistic infections or malignant disease is likely related with a higher incidence of Aspergillus spp. infection in these patients.3
To our knowledge, this is the first report of hematogenous spondylitis due to Aspergillus spp. in an HIV-infected patient. The lungs and paranasal sinuses are the most frequent locations of IA. Aspergillus can extend either locally, from the paranasal sinuses to adjacent organs such as the brain, orbit or ears, or by hematological dissemination. Both mechanisms were seen in our patient: direct extension through the paranasal sinuses to the orbit and hematological spread to the spine. Previous reports have shown that disseminated disease has a drastically lower survival than localized disease.3 Another case of spondylitis by Aspergillus spp. was described in 1990, but it was caused by direct extension from a primary pleural and pulmonary infection.4
The present report illustrates the poor prognosis of invasive infection by Aspergillus spp. despite specific treatment. Early diagnosis and aggressive treatment, including surgery in most cases, remain the most effective therapeutic strategies.5 In patients with disseminated disease, however, antifungal therapy is the only option. Although survival in IA seems to be improving with the development of new antifungal agents such as voriconazole and echinocandins, much work remains to be done before the currently gloomy prognosis of IA can be changed.6–8